“Developments in neurosciences over the last 50 years have been phenomenal, but the impact on the practice of psychiatry has been weak,” maintains Randolph Schiffer, M.D. Schiffer trained as a psychiatrist and as a neurologist before becoming chair of neurology, neuropsychiatry, and behavioral science at the Texas Tech University Health Sciences Center in Lubbock.
Today he's trying to nudge the two fields closer together in the context of his department's residency training program. It may be slow going, if results of a survey of residency training directors are any indication.
As part of their APA/GlaxoSmithKline fellowship in 2003-2004, Joshua Roffman, M.D., and five colleagues created a 28-question survey and sent it to directors of all psychiatry residency programs in the United States and Canada. The results appeared in the May American Journal of Psychiatry.
“Residents know neuroscience is important, but how it will play out in the future is still a mystery,” said Roffman in an interview. He is now an instructor in psychiatry at Harvard Medical School and a psychiatrist at Massachusetts General Hospital, where he also holds a postdoctoral fellowship in neuroimaging and genetics.
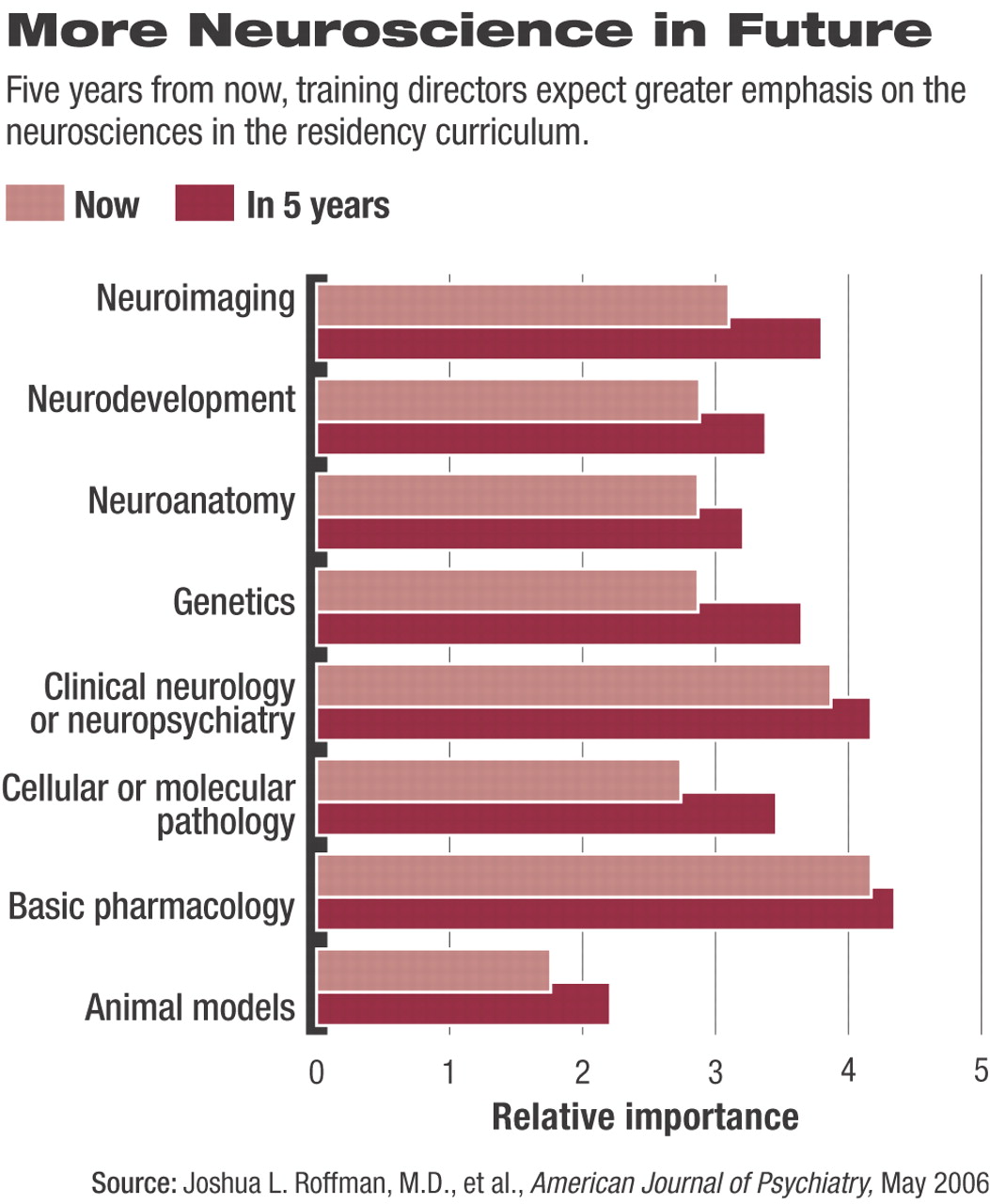
The researchers defined neuroscience as including neuroanatomy, neurodevelopment, neuroimaging, cellular and molecular pathology, genetics, animal models, neuropsychiatry, and basic pharmacology (such as neurotransmitter systems, receptors, and neural circuitry), but not clinical pharmacology.
They received replies from 77 of 182 training directors; Roffman said that the response rate is similar to that of other surveys and fairly represents the range of institutions covered.
Neuroscience is now a fixture in residency programs, Roffman and colleagues concluded. Just 19 percent used a stand-alone approach in which the subject is presented isolated in time from the rest of the curriculum. About 38 percent of the programs organized neuroscience training to run parallel with other courses, and 40 percent used a combination of the two approaches.
“More neuroscientific teaching took place in formal lectures or other less-clinical settings than in wards, clinics, or case conferences,” said Roffman. That could change in the next decade as neuroscience research becomes better integrated with clinical practice, something that residency training directors seem to expect, even if it happens only modestly in the present.
Residents and practicing psychiatrists know neuroscience is important, but they're still trying to figure out how to apply it in their day-to-day work.
“The role of neuroscience in psychiatry reminds me of opening the door to the refrigerator,” said Schiffer. “You know the light goes on and off, but you don't know why.”
To bridge that gap in his department at Texas Tech, residents are involved with neuroscience and neurology for all four postgraduate years. That includes not just lectures but being on call for neurology in their third and fourth years. Away from the clinic, residents study topics such as intensive care neurology and neuroimmunology.
“In their third year, we now place them in the memory disorder research clinic to improve their understanding of cognition,” said Schiffer.
Nationally, neuroscience training accounts for 12 percent of the residents' curriculum, although the directors thought it should occupy about 20 percent. More than 8 out of 10 said they expected continued growth over the next five years, with major increases in time allotted to genetics, neuroimaging, and cellular and molecular pathology.
Where the time will come from is an interesting question. About 80 percent of training directors said that psychotherapy training time had remained the same over the last five years, and 73 percent expected it will do so over the next five years, though 18 percent said content will increase in that time. There's no consensus yet on what parts of the curriculum will be reduced to accommodate an expansion.
“Nearly all respondents believed that neuroscience education is relevant even for those residents who will ultimately become primarily therapists or analysts,” said the authors.
“Psychotherapy isn't going to die, but neuroscience will provide more of a context,” added Roffman.
“Most psychiatrists go into psychiatry because they want to be clinicians,” said Ronald Krasner, M.D., interim chair of the Department of Psychiatry and Behavioral Sciences at the Feinberg School of Medicine of Northwestern University and president of the American Association of Directors of Psychiatric Residency Training. “They want to know how neuroscience will help them when they sit down with a patient. Maybe in 25 years, we'll have ways of using neuroscience in the consulting room, and psychiatric residency will be completely different. But at the moment, I don't have an MRI in my office.”
Overall though, said Krasner, “this paper pulls us into the future.” There are both immediate and long-term needs for neuroscience training, but design of residency training programs is not easy to change. For instance, only about one-third of programs are directly connected to medical schools, with limited access to academic resources and researchers in neuroscience for the rest.
Also, programs are controlled not only by their training directors, but assume their final form after pulling and pushing by department chairs, medical specialty groups, the AMA, American Hospital Association, Association of American Medical Colleges, American Council on Graduate Medical Education, and others.
Graduate medical education is funded in part by Medicare, which imposes more constraints through a complicated formula filtered through hospitals and hemmed in by clinical service requirements. As a result, any change will come slowly, he said.
“Psychiatry isn't at a dead end now, but it is on a narrow road,” said Schiffer. “We need to go down some new roads and one of those is neuroscience.”