Personality disorders—like the patients who suffer from them—are complex phenomena, stubbornly resisting the trend in medical and psychiatric nosology toward simplification and standardization.
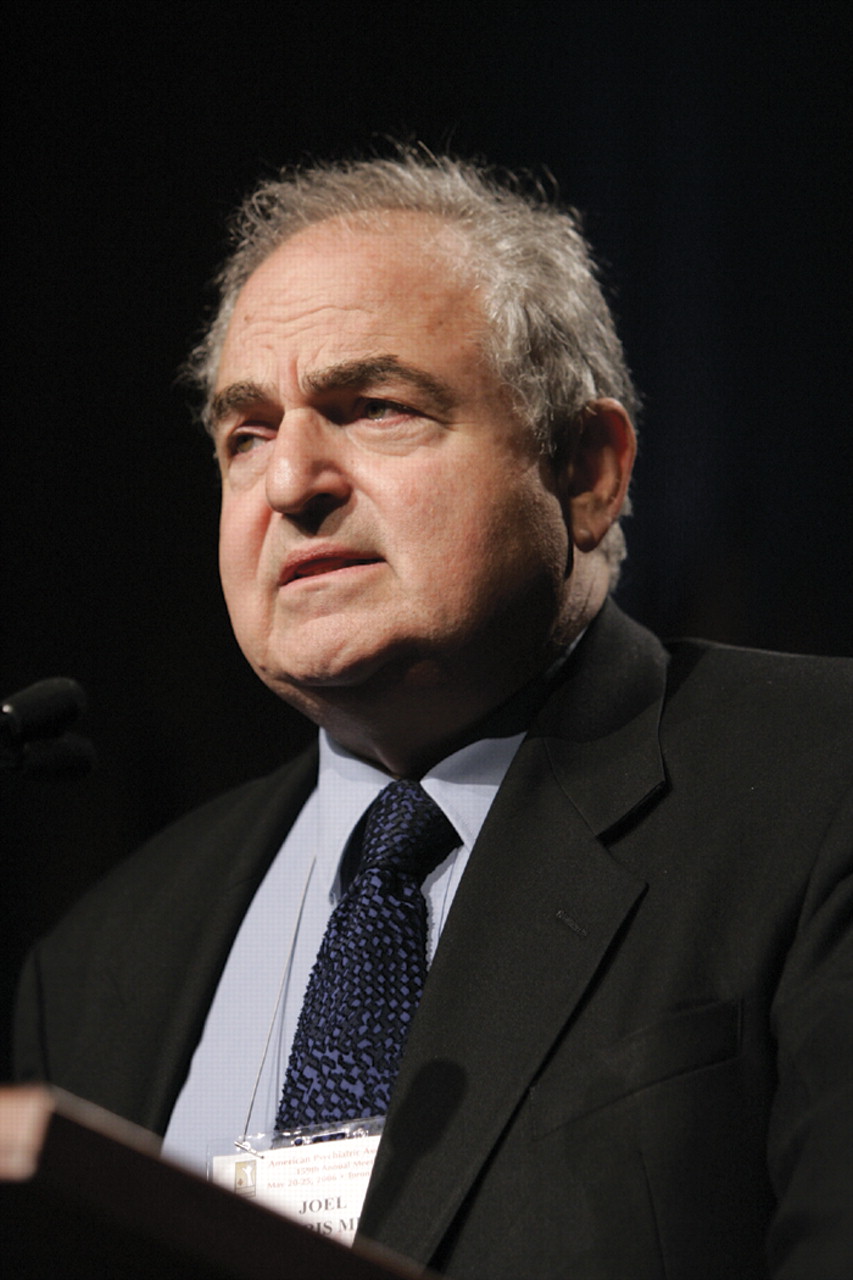
Much about them, including prevalence, etiology, biology, course, and treatment, remains to be learned or better elucidated, and their diagnostic classification is badly in need of refinement or overhaul, said Joel Paris, M.D., in a lecture at APA's 2006 annual meeting in Toronto in May.
Paris, who has published extensively on the subject of personality disorders, especially borderline personality disorder (BPD), said there have been repeated efforts to redefine personality disorders as variants of Axis I disorders—especially bipolar disorder and posttraumatic stress disorder—a move toward simplification that he said should be resisted.
“People want to have simple, well-defined diagnostic entities with specific treatments using drugs,” Paris said. “Some Axis I diagnoses fit that model, but personality disorders don't. People try to explain them away in other ways. But what this is really about is the fact that the world is complicated, and personality disorders are complicated, even if no one wants it to be that way.”
Paris noted, for instance, that some in the field have focused on the mood instability characteristic of BPD and have tried to suggest that BPD is really an expression of bipolarity.
“I think that's wrong, but it's a very popular idea,” Paris said. He cited fellow BPD researcher John Gunderson, M.D., of McLean Hospital in Belmont, Mass., who has noted that it is difficult to find a BPD patient who has not been diagnosed with bipolar disorder and treated with a mood stabilizer. yet mood stabilizers do not work as well with patients with BPD.
“This is more of a hope than evidence-based medicine,” Paris said.
Another group has argued that BPD is a form of posttraumatic stress disorder, based on a belief in the prevalence of childhood trauma in patients' lives. yet research findings have shown that this isn't the case.
“Patients are assumed to have had a childhood trauma when they haven't,” Paris said. The effects of childhood abuse are broad and nonspecific, he said, citing community research showing that most people who experience some form of abuse never develop any mental illness.
“Most children are resilient, so abuse and trauma are risk factors but not causes,” he said.
Paris is a professor and chair of the Department of Psychiatry at McGill University in Montreal and editor in chief of the Canadian Journal of Psychiatry. He is also a past president of the Association for Research in Personality Disorders.
Paris said recent research is helping to clarify issues around personality disorders, including diagnostic specificity, treatment outcome, and long-term course. A substantial body of knowledge has accumulated on some of the disorders, especially borderline and antisocial personality disorders. But much more about personality disorders remains to be learned and reconceptualized, and much of Paris's lecture was a catalog of the challenges to understanding, diagnosing, and treating these patients.
Especially problematic is the widespread overuse of drugs in the treatment of patients with personality disorders. “These patients are clinically difficult and noncompliant, and drugs don't have predictable results,” Paris said. “They are vastly overused. Several patients have told me that when they learned they had a personality disorder, they were relieved. They said, `I thought I was just a bad patient because I didn't get better on Prozac like everyone else.'”
Paris said it is not uncommon for patients with a personality disorder to be treated with as many as five drugs: a combination of multiple antidepressants, mood stabilizers, and benzodiazepines. “The problem is that there is no science to support polypharmacy, and it's probably bad for patients,” he said.
Because comorbid depression is frequently a component of personality disorders, and clinicians are familiar with depression, they often opt to treat that aspect of a patient's condition with an antidepressant. But Paris said comorbidity is an artifact of the DSM system of classification, common to almost every condition in the manual.
“The response to medications is different,” he said of patients with BPD and other personality disorders. “When you give patients with classical depression an antidepressant, they may be cured in a few weeks. But you never see that in patients with borderline personality. It might take the edge off, but patients never go into remission.”
He added that several psychotherapies have been shown to be effective, though all are lengthy and expensive. For BPD, Marcia Linehan's dialectical behavior therapy is the most extensively researched model; also promising are schema therapy, mentalization-based therapy, and the transference-focused therapy pioneered by Otto kernberg, M.D.
Paris expressed dissatisfaction with guidelines for BPD that he said support polypharmacy and hospitalization. He said that hospitalization is“ toxic” for BPD patients and has not been shown to prevent suicide.
He was critical as well of the commonly cited prevalence figure of 10 percent for personality disorders. “I don't believe this figure; I think it's much too high,” he said. “By DSM criteria, it may be 10 percent, but we are cutting too broad a swath in thinking about personality disorders. We need to narrow down the concept. I would like to reserve the diagnosis for more severely affected populations.”
Paris was emphatic that the system for diagnostic classification of personality disorders was ripe for change, saying it should be substantially revised in DSM-V, due in 2011. He was especially critical of the current categorical approach to diagnosis, whereby a patient who meets an arbitrary number of criteria has a disorder.
Among the more popular competing ideas for how to reconceptualize personality disorders is a “dimensional” model, whereby patients are assessed according to dimensions of personality functioning. One prominent system is the Five Factor Model in which personality traits are grouped into five encompassing dimensions: neuroticism, extraversion, openness to experience, conscientiousness, and agreeableness.
Paris cited the Collaborative Longitudinal Personality Disorders Study (CLPS), which was summarized last year in a paper in the October 2005 Journal of Personality Disorders. That study suggested that personality disorders may be reconceptualized as hybrids of stable personality traits and intermittently expressed symptomatic behaviors.
One intriguing finding from the study was that patients often cease to meet diagnostic criteria over time. That finding complements other studies showing that specific symptoms of personality disorders appear to diminish after age 40, though underlying personality traits persist.
“Most patients don't keep their diagnoses,” Paris said at the Toronto lecture. “The question is whether they have really remitted. Even when they stop meeting DSM criteria, their functional scores don't change. They continue to have serious problems. Borderlines may stop cutting themselves and may stop overdosing—that's worth something—but it doesn't mean they are cured. To me the CLPS findings present an important challenge to the current criteria in DSM Axis II.”
Despite the difficulty that the concept of personality disorder presents to clinicians and researchers, it remains a valid diagnosis and applies to up to 25 percent of most psychiatrists' patients. For this reason, he said personality disorders have been referred to as a “stepchild” of psychiatric nosology—challenging to embrace, but undeniably a member of the family.
“Psychiatry's stepchildren may have come of age,” Paris said.“ They are unique disorders, not simply variants of Axis I disorders, and diagnoses of personality disorders are associated with serious morbidity. Etiology and pathogenesis need a lot more research, but the prognosis is much better than we used to think. BPD does seem to improve over time, so we can tell our patients, `yes, you have borderline personality, but you are going to get better.'” ▪