Medication errors are a major cause of patient morbidity and mortality in nearly all medical specialties. More than 7,000 deaths each year in the United States are attributed to medication errors, according to a recent Institute of Medicine report, and researchers have estimated that nearly 60 percent of all adverse events are the result of medication errors. Nonetheless, few studies have examined medication errors in psychiatry.
Medication errors can result either from a prescribing error or a dispensing error or a combination of both. A new study by a group of British pharmacists suggests that in psychiatry, prescribing errors are fairly common.
David Taylor, Pharm.D., the chief pharmacist at Maudsely hospital in London, teamed with pharmacists at other U.K. National Health Service mental health centers to evaluate all prescriptions written in a one-week (five working days) period in June 2004. Their report appears in the July Journal of Psychopharmacology. The study was funded by the United Kingdom Psychiatric Pharmacy Group.
A total of 22,036 prescriptions were reviewed from eight outpatient acute mental health centers and one inpatient psychiatric hospital to identify errors in the writing of the prescription that could result in “an unintentional significant reduction in the probability of treatment being timely and effective, or an increase in the risk of harm when compared with general accepted practice.”
Prescribing errors were categorized by pharmacists at the nine sites as grade 1, an error or omission of doubtful or negligible importance; grade 2, an error or omission likely to result in minor adverse effects or worsening of condition; grade 3, an error or omission likely to result in serious effects or relapse; or grade 4, an error or omission likely to result in fatality. A panel of five “expert psychopharmacologists” reviewed all grade 3 and grade 4 errors and assigned a consensus rating.
Of the more than 22,000 prescriptions checked, 11,668 (52.9 percent) were for psychotropic medications. Prescribing errors meeting the study definition were detected in 523 (2.4 percent) prescriptions. More errors occurred with prescriptions for antipsychotics (17 percent) than for any other category. Hypnotics and anxiolytic medications were involved in the second highest proportion of prescription errors (13.2 percent).
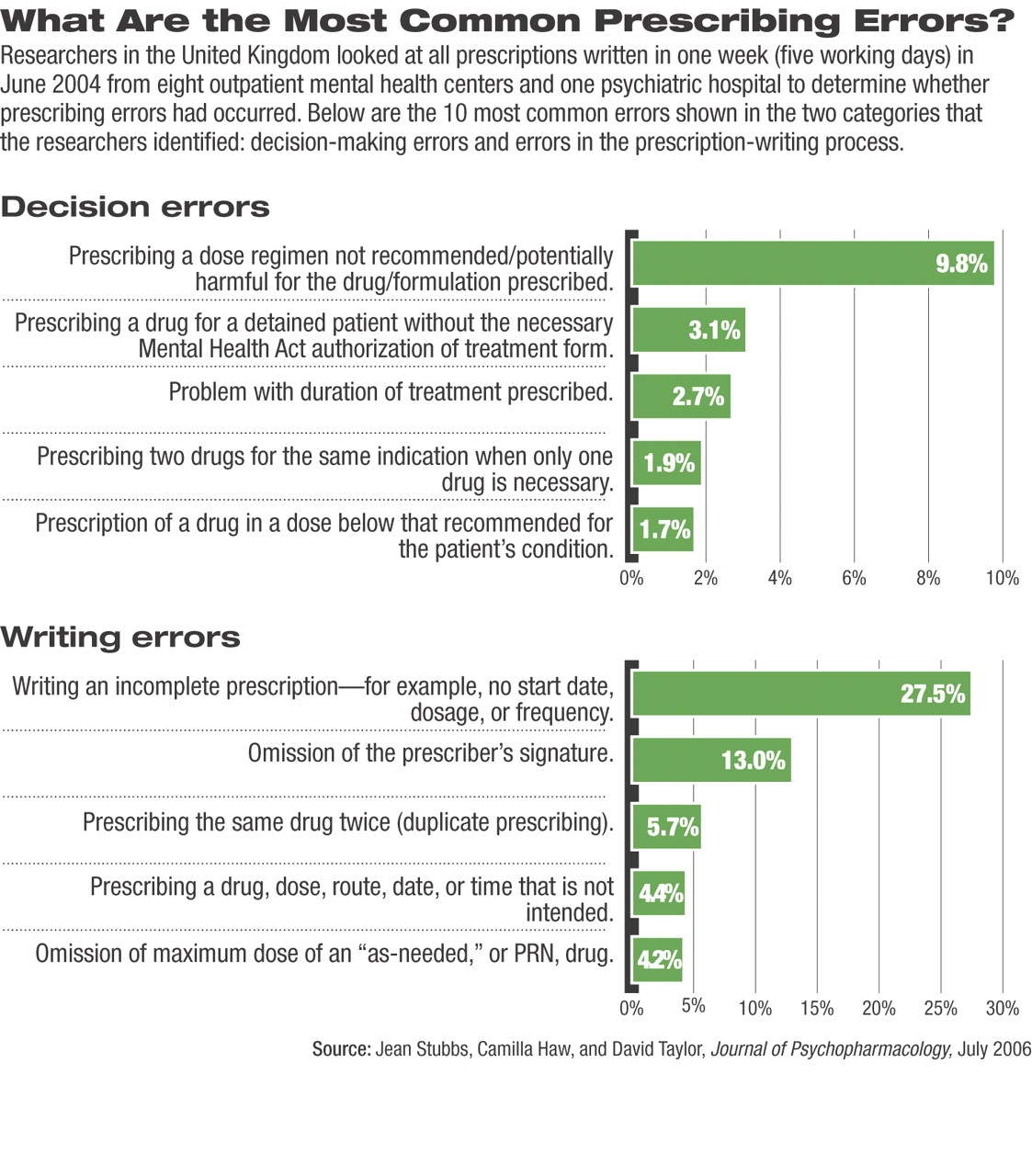
Taylor and his colleagues found that “prescription-writing errors” were far more common (77.4 percent) than “decision-making errors” (22.6 percent). Errors categorized as involving the writing of the prescription most frequently involved writing an incomplete prescription (27.5 percent of total prescribing errors), such as not specifying a start date or failing to completely specify dosage, dosage route, or frequency of administration. In 13 percent of prescriptions, the prescriber neglected to sign the prescription. The problem with 1.5 percent of the prescriptions was illegible handwriting that could not be accurately transcribed by a pharmacist. Other prescription-writing errors involved writing milligrams when the drug strength should have been written as micrograms or misspelling a drug name.
“Decision-making errors” most frequently involved the“ prescribing of a dose regimen that is not recommended for the drug/formulation prescribed” (9.8 percent of all prescriptions). Other errors were categorized as involving prescribing a drug for a longer period than recommended or approved (2.7 percent) or prescribing two drugs for the same indication (1.9 percent). Dosages below the recommended effective dose range for a patient's condition were somewhat less common (1.7 percent), as was the failure by the prescriber to consider a potentially significant drug interaction (1.1 percent).
The majority of patients receiving a prescription containing an error were inpatients (83.4 percent) and were between the ages of 18 and 64 (69.2 percent). In 280 of the 523 errors (53.5 percent of prescription errors), the medication was administered to the patient before the error was identified.
Fortunately, the majority of the errors identified in the study were grade 1 (47.8 percent) or grade 2 (45.9 percent). Only 17 errors (3.3 percent) were classified as grade 3 or grade 4. Most of these 17 errors involved the prescribing of high doses of single drugs or of multiple drugs that when taken together could result in serious central nervous system depression, potentially precipitating respiratory failure.
Overall, Taylor and his colleagues concluded, “pharmacy staff detected on average one prescribing error for every 42 prescriptions checked.” Over three-fourths of the errors amounted to “slips of the pen,” that is, were a prescription writing error. Thankfully, they noted, “most errors were of doubtful or minor importance, but “1 in 33 errors was deemed likely to result in serious effects or death.”