Without Congressional action, psychiatrists will on average face cuts in Medicare reimbursement of 7 percent on January 1, 2007, as a result of a final rule issued by the Centers for Medicare and Medicaid Services (CMS) last month.
The impending cuts are the result of two separate adjustments in the formula by which physicians are paid under Medicare: a 5 percent overall payment reduction for all physicians, as part of an annual update issued by CMS, stemming from a change to the “conversion factor” that is adjusted from year to year to maintain budget neutrality; and a separate adjustment to work and practice expense relative-value units (RVUs).
(The work and practice expense RVUs are components of the Resource-Based Relative Value Scale, the elaborate formula used to calculate physician payment under the Medicare program; another component is the malpractice insurance expense RVU. To calculate a payment for each CPT code, the three components, adjusted for geographical differences, are added together and multiplied by the conversion factor.)
On average, psychiatrists will face a 3 percent decrease due to the change in work RVUs, in addition to the across-the-board 5 percent cut resulting from the change to the conversion factor; they will receive an increase of 1 percent due to recalculation of the practice expense RVU.
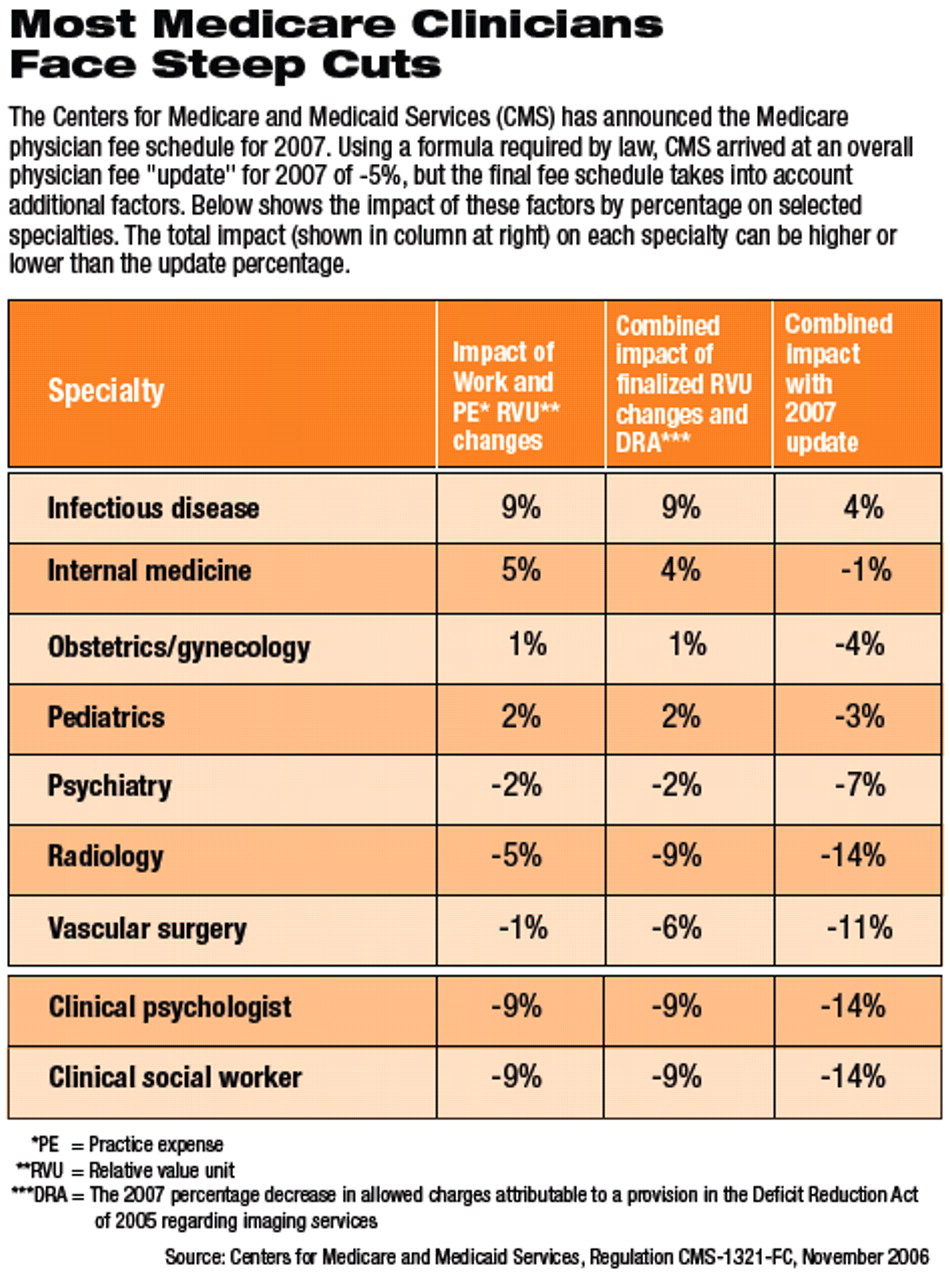
The cuts also apply to other providers of Medicare services (see
table on page 28), and some will be hit harder than psychiatrists.
The impending cuts riled doctors at the AMA meeting last month (see article at right) and have added urgency to physician groups' demand that Congress replace the payment formula, especially the much derided sustainable growth rate component. That component pegs fee changes to Congressionally designated spending targets that do not reflect year-to-year changes in practice expenses. The AMA has been trying to get Congress to intervene legislatively to reverse the payment reductions.
“If Congress does not act, we fear that physicians will be forced to make a difficult decision,” said AMA Board Chair Cecil Wilson, M.D., in a statement released after last month's AMA meeting in Las Vegas.“ Nearly half of physicians say Medicare cuts will force them to decrease or stop taking new Medicare patients. Current Medicare payments in 2006 are about the same as they were in 2001, and nine years of cuts to physicians totaling about 40 percent will have a severe impact on seniors' ability to get health care.
“Eighty senators and 265 representatives have called on Congress to take action in this session of Congress to stop the cuts, and Congress' own advisory committee on Medicare has recommended tying Medicare payments to practice costs,” said Wilson.
Tom Leibfried, deputy director for congressional affairs in APA's Department of Government Relations, told Psychiatric News that members of Congress from both parties have been saying that some action to preserve Medicare payments is a priority. At press time, the Senate Finance Committee was expected to propose by December 5 a small percentage increase in overall physician payment.
But Leibfried said Congress must act before its session concludes before Christmas. And he said the recent election that turned majority control of both houses of Congress back to the Democrats has added to the potential political variables, making prognostication more complicated.
One certainty, Leibfried said, is that congressional intervention to preserve or increase physician payments will be tied to participation in quality-reporting programs such as the CMS program for pay for performance, which is itself the subject of much opposition among physicians (see box on page 6). Some Democrats, however, have “indicated an interest in putting pay for performance on a slower track, to give physician groups and CMS more time to test them before trying them out.”
The five-year review of work RVUs, which was completed this past summer, is designed to allow for a reassessment of the intensity of work required of physicians for each procedure they perform. For example, some procedures may have become easier or harder to perform over time because of the introduction of technology.
The government's recommendations for changes to the work RVUs are based on those submitted by the AMA's Relative Value Scale Update Committee, a 29-member body including representatives from all major medical specialties. However, changes to the payment formula are required by law to be“ budget neutral”—in this case, it meant that changes in work RVUs that resulted in an increase or decrease in overall outlays of more than $20 million had to be compensated for by adjustments in other areas.
CMS has said that the changes in payment for evaluation and management codes—which was significantly increased this year—and increases in the valuation of other codes were expected to increase overall expenditures by $4 billion. Because of the budget-neutrality requirement, CMS created a separate “work adjuster” that it applied to the work RVUs, which reduced those values by 10 percent. The work adjuster will likely vary from year to year depending on Medicare spending.
“Nearly half of physicians say Medicare cuts will force them to decrease or stop taking new Medicare patients.”
APA and the AMA had urged CMS to adjust for budget neutrality by shifting the cut to the conversion factor—that factor that is multiplied by the sum of the RVUs. This would have the effect of spreading out the negative impact across all the RVUs—work, practice expense, and malpractice—and would mitigate the negative impact on psychiatrists since most of their RVUs are part of the work component (Psychiatric News, September 15). However, that recommendation has not been heeded, and CMS is proceeding with its original plan. This has resulted in average payment reductions for 2007 of more than 10 percent for physicians overall and approximately 7 percent for psychiatrists.
Information on the Medicare physician fee schedule for 2007 and background documents can be accessed at<www.cms.hhs.gov/SustainableGRatesConFact/>.▪