Problems continue to plague the new Medicare Part D prescription drug program, with some states extending emergency coverage of “dual eligibles” transitioning from Medicaid into the program.
And a recent poll shows that fewer than half of American seniors had enrolled in the program or a plan by the last week of February or were planning to do so.
Irvin (Sam) Muszynski, J.D., director of APA's Office of Healthcare Systems and Financing, said that his office is continuing to receive reports through the Part D monitoring system it established regarding serious problems with enrollment of patients in the program and lack of access to necessary psychotropic drugs for patients who did get properly enrolled.
“There's a large gap between the Centers for Medicare and Medicaid's [CMS] policy on continuity of care for medically vulnerable patients and the drug plans' compliance with them,” he said.
“The amount of time we are spending with prior authorizations is bringing the rest of our work to a standstill.”
Muszynski added that CMS has continued to assure APA that psychotropic drugs are supposed to be made available through every participating drug plan.“ The draft 2007 formulary guidelines were sent to us on February 23 by CMS, and these continue the `all or substantially all' protections that are supposed to be in place for antidepressants, antipsychotics, and anti-convulsants” (see
page 1).
(In the run-up to January 1, CMS had said that “all or substantially all” of six classes of drug would be included on drug formularies. Those included antidepressants, antipsychotics, anticonvulsants, anti-neoplastics, immunosuppressants, and HIV drugs.)
APA members can contact the Association's Part D monitoring system by e-mail at
[email protected] or by phone at (866) 882-6227. APA is continuing to post information with its partners about the program at<www.mentalhealthpartd.org>. APA is particularly interested now in information about how the prior authorization and appeals process is working.
Psychiatrist Andrea Stone, M.D., medical director of the Carson Center for Human Services in Westfield, Mass., has reported to Psychiatric News a host of problems with the new program since its beginning on January 1. Those include unexpected copayment requirements, failure to ensure continuity of care for dual-eligible beneficiaries transitioning from drug coverage under their Medicaid plan, and utilization review requirements that detract from clinical duties and sometimes result in lengthy delays in receiving medication.
More than six weeks into the start of Part D, and after Massachusetts instituted emergency coverage for dual eligibles and other beneficiaries unable to access their medication, Stone told Psychiatric News that she and her staff are still busy coping with enormous problems associated with the program.
She acknowledged that while many beneficiaries may be smoothly receiving their medications, it is the problem cases that command attention, and those problems are not insignificant, she said.
Requirements for prior authorization that are burdensome and sometimes clinically illogical appear to be the most persistent complaint.
“The amount of time we are spending with prior authorizations is bringing the rest of our work to a standstill,” she said. “This is affecting every level. The secretaries are spending enormous amounts of time on hold with the prescription drug companies, nurses are trying to get people medications by whatever means possible in the short term, and the doctors have to fill out forms providing clinical information on patients in order to justify prior authorizations. Meanwhile, we are not getting responses very quickly.
“The kind of information they want includes previous treatments and reasons for failure, and for some patients who have been stable for 10 years, that kind of information can be very difficult to track down,” she said.“ We understood that if people were stable on meds by January 1, they would have no problem receiving their medication. That may be happening in some cases, and we only hear about the problems, but it's not happening for everyone.”
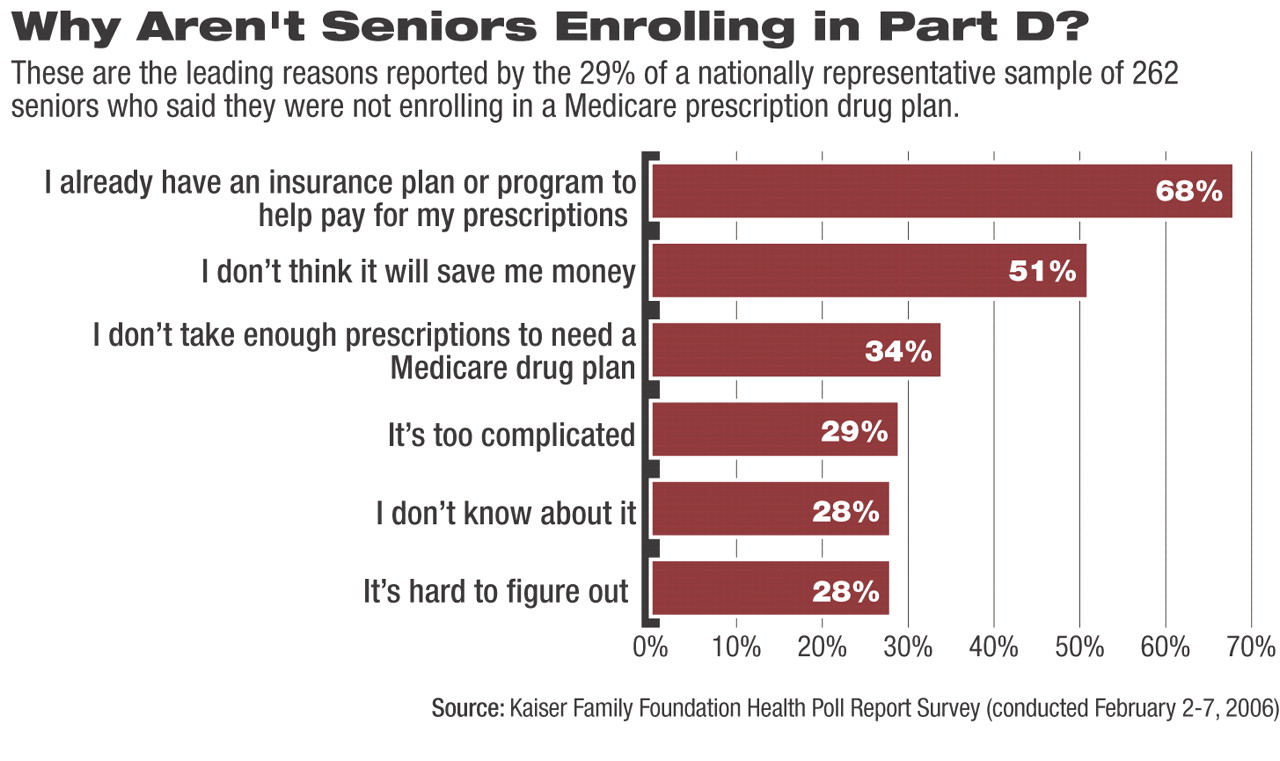
Meanwhile, a Kaiser Family Foundation tracking poll found that 45 percent of seniors said they enrolled or plan to enroll in a drug plan, 29 percent said they do not intend to enroll in a drug plan, and 23 percent said they are uncertain. The majority of those who do not plan to enroll said they have another program or plan that helps pay for their prescriptions.
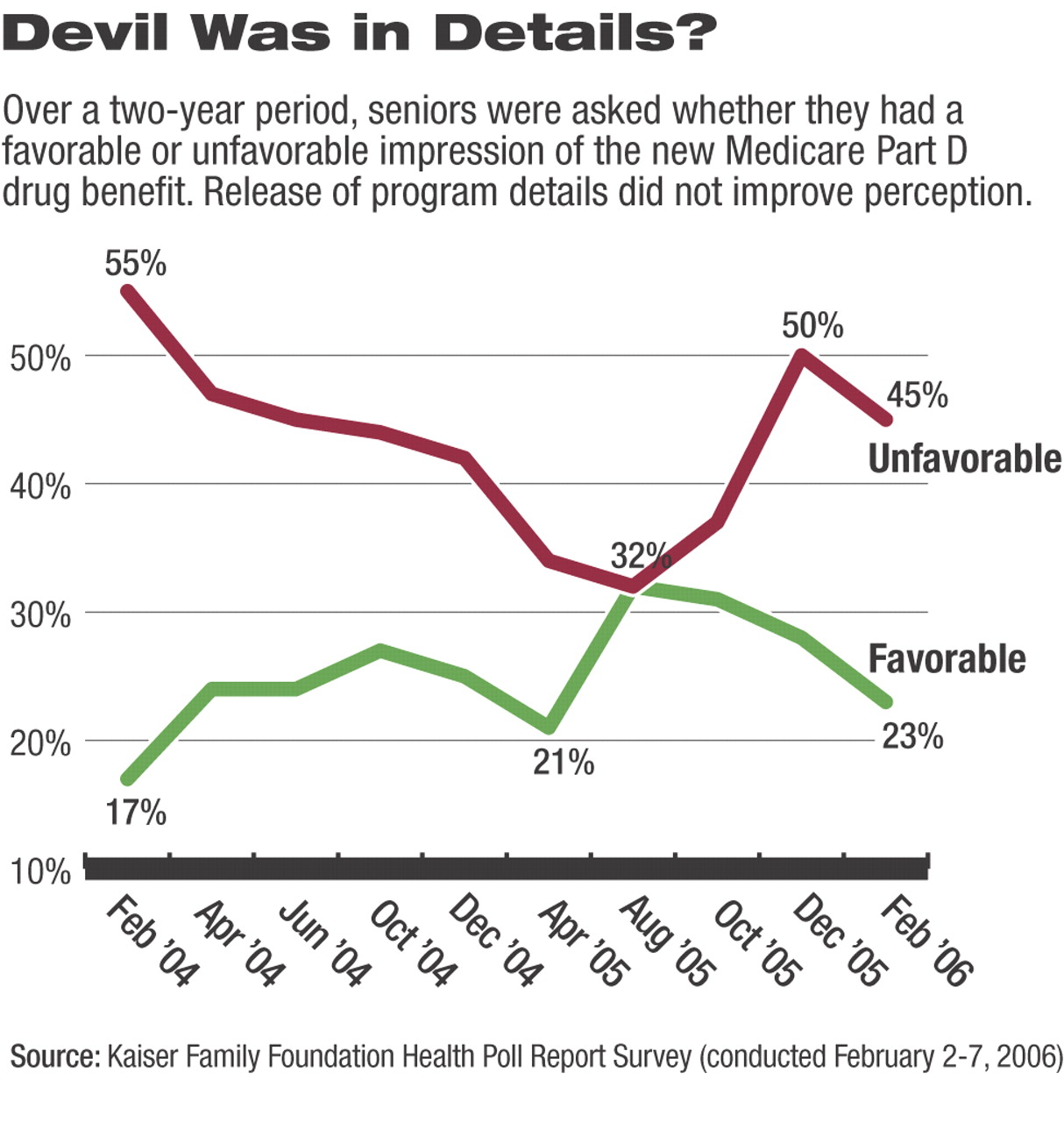
Though more seniors are enrolling in a drug plan each month, the tracking poll also showed that seniors have become less enthusiastic about the new Medicare drug benefit over the past six months. Seniors are now almost twice as likely to say they view the benefit unfavorably (45 percent) as favorably (23 percent). That finding reflects a shift since August, when seniors' positive views peaked, and they were as likely to view the benefit favorably (32 percent) as unfavorably (32 percent).
The nationally representative tracking poll was conducted among 262 seniors from February 2 to February 7, more than a month after the January 1 start date for the Medicare drug plan.
“A substantial number of beneficiaries are already enrolled, but a lot turns on what those who are on the fence decide to do between now and May 15,” said Drew Altman, president and CEO of Kaiser Family Foundation.
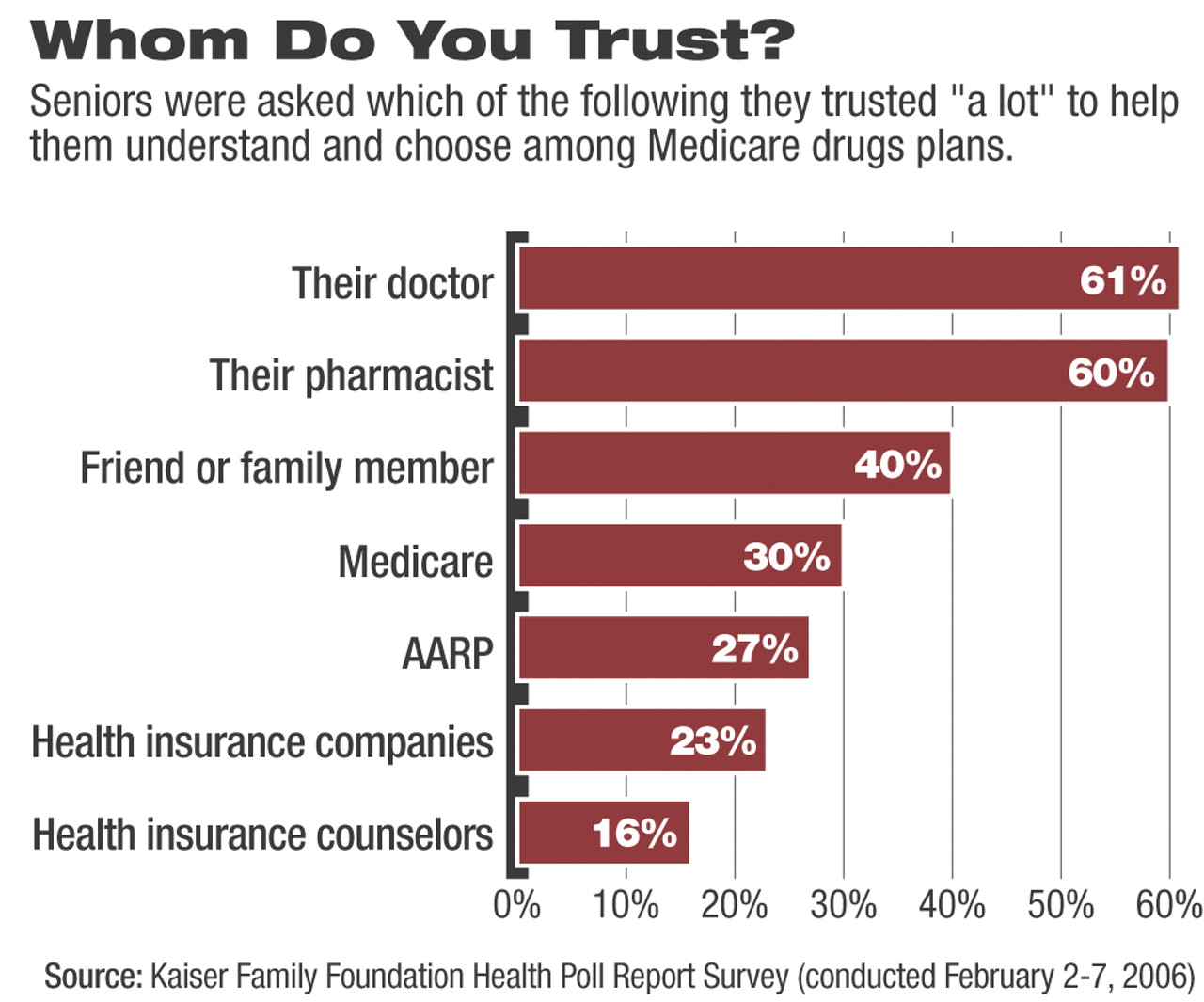
Mollyann Brodie, a Kaiser Family Foundation vice president and director of public opinion and media research, said, “The plan finder at<Medicare.gov> is the best way to compare Medicare drug plans, but relatively few beneficiaries and their helpers are using it to date.”
In other news, some states are seeking to extend emergency coverage of dual eligibles experiencing problems with access to drugs under the new program.
“We see no evidence that sufficient improvements have been made to the Medicare prescription drug program that would give the state any confidence that the most vulnerable clients in our state will be adequately served should we turn their drug coverage over to Medicare and its contractors,” wrote Ann Clemency Kohler, director of New Jersey's Division of Medical Assistance and Health Services, in a letter to CMS.
Kohler said that some 4,000 dual-eligible beneficiaries in the state were not yet enrolled in a prescription drug plan, and another 4,000 beneficiaries had been “auto-enrolled” in plans that did not even operate in New Jersey. And about 600 dead people were enrolled in Part D.
“To date we have paid $113 million in claims for our dual eligibles and... continue to pay $2.6 million per day,” Kohler wrote. “In light of the significant data issues, it is unlikely that the problems with Part D will be resolved” quickly. ▪