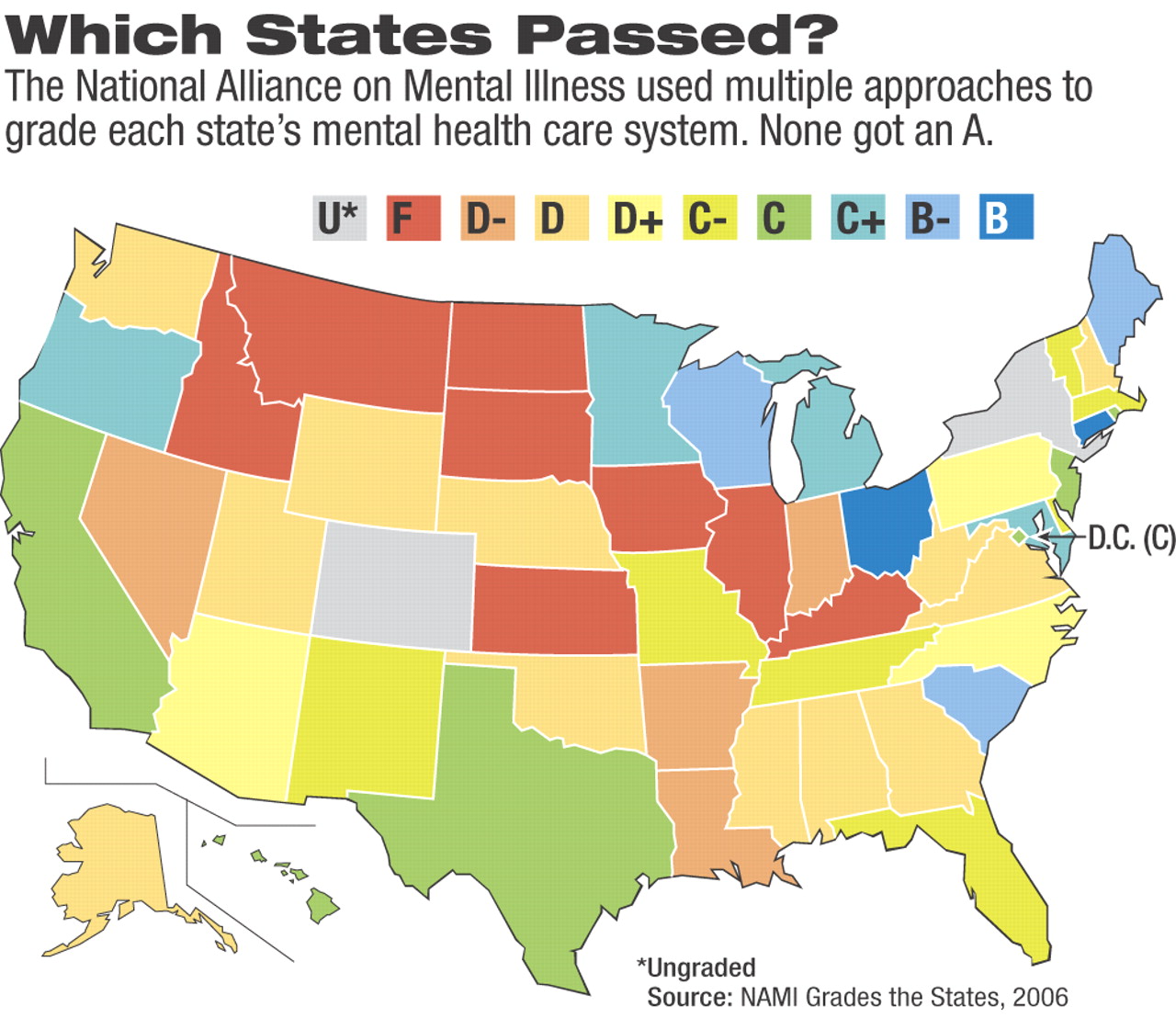
State public mental health care systems generally earn poor-to-failing grades in terms of the mental health care they offer their residents, according to a national “report card” issued by the National Alliance on Mental Illness (NAMI). But the report also hailed some states' innovative efforts and commitment to mental health care in the face of budget shortfalls.
The report assessed mental health care accessibility, affordability, and quality in all but two states and rated the majority with Ds or Fs. Colorado and New York officials declined to participate so were left without a grade.
The grades were based on how well each system met a series of 10 elements, which included comprehensives services and support, access to acute and long-term treatment, and sufficient funding.
“These are things we value and think people should actually have,” said Kenneth Duckworth, M.D., NAMI's medical director. “The report says the programs should be accountable to the consumers who use it.”
The two highest-scoring states—Ohio and Connecticut—were praised for innovative uses of jail-diversion programs and bilingual services, respectively. Conversely, Connecticut was chided for long emergency room wait times for hospitalization, while Ohio was criticized for lacking a mental health care parity law. Both states received a “B” in the report.
Michael Fitzpatrick, NAMI's executive director, said the highest rankings stemmed in part from those states' “consistency of vision over time,” the use of consumer feedback, and a regular examination of program outcomes. An “A” is possible when a state meets the“ B” goals and provides a comprehensive range of programs, he said.
Although the report examined each state's efforts in specific areas, such as the provision of supportive and affordable housing to those recovering from mental illness, its emphasis was on what new initiatives each state was trying.
Jeffrey Geller, M.D., a member of the APA Council on Social Issues and Public Psychiatry and incoming Area 1 trustee, said the report did an excellent job with an impossible task. The approach was limited because it largely depended on the states to assess their own efforts, which leaves the findings highly vulnerable to personal slant, he said.
The report's findings were also based in part on a “test drive,” in which the report's contributors used a series of questions they believed would provide them with a clear picture of mental health services in the states. The reports also were based in part on interviews with consumer and family advocates, as well as legal and policy experts on their perspectives of each state's system.
The report, Geller said, did an excellent job of highlighting the overall poor level of care the states provide for their citizens with mental illness.
The list of state innovations may provide less incentive for other states to improve their programs, however, than “putting in their face the disgraceful way they treat those with mental illness,” Geller said.
Among the eight states given failing grades, Iowa was praised for its establishment of the statewide Technical Assistance Center for Evidence-Based Practices to promote their use in mental health care.
“There are some good things happening, even in abysmal states,” Duckworth said.
The report described another failing state, Kansas, as a place where good intentions exist but the rhetoric often doesn't match reality. The state was criticized for lagging in the decriminalization of mental illness and lack of access to acute inpatient treatment. The report's authors were also puzzled as to why the state lacks an Assertive Community Treatment (ACT) program, one of the oldest and most effective evidence-based practices and a critical component in a comprehensive mental health system.
The report criticized Iowa for a lack of effort to expand access to services for people who have severe mental illness and live in rural jurisdiction, which are the vast majority of the state's jurisdictions.
The report examined only the public mental health systems of the states because they fund the majority of mental health care, and even affluent residents with serious mental illness are statistically likely to require some care in the public system eventually.
The report identified some hopeful trends, including the increasing use of jail-diversion programs. The report noted that the effort's importance is underscored by research that estimates that 16 percent of the nation's inmates, or 300,000 people, suffer from serious mental illness.
Another growing trend is the provision of services by peers, who may offer case management, drop-in centers, and outreach programs.
Some innovative mental health program financing has been adopted by states, according to the report, such as California's Proposition 63 initiative in 2004, which provides a stable, significant source of revenue for mental health services through a so-called millionaire's tax.
NAMI representatives said they hoped the report might serve to educate state officials and legislators, who may not realize or remember that cuts to vital services for people with mental illnesses raise rather than reduce the overall costs to society. The issue is especially important this year with states slated to cut billions of dollars from their Medicaid systems, which pay for 50 percent of the mental health services that states administer. Some Medicaid changes under consideration are likely to impact people with mental illness.
Among the Medicaid options Congress recently approved for states is the institution of higher copayments.
“Copays for mental health services discourage people from seeking help,” Duckworth said.
Some states were hailed for their efforts to bolster their Medicaid mental health programs, even in the face of a reduced federal financial commitment to the state and federal partnership.
Although the report found few states have increased their mental health funding in recent years, it cautioned that additional funds only benefit mental health care consumers when they flow through effective and efficient treatment and assistance programs. The skepticism of some administrators and legislators toward mental health care may be justified if evidenced-based and emerging best practices are not emphasized by mental health professionals, Duckworth said.
The report praised the efforts in this area by the federal Substance Abuse and Mental Health Services Administration and the National Association of State Mental Health Program Directors.
The grades are the first follow-up of NAMI's previous mental health systems“ report card” issued 15 years ago. NAMI plans to rate the states again in three years.
The report is posted online at<www.nami.org/grades>.▪