A landmark report on comorbid medical and mental illness recommends that people with serious mental illness (SMI) be designated as a distinct health-disparities population under the federal government's initiative to reduce disparities in health outcomes.
That was just one recommendation in the extensive report “Morbidity and Mortality in People With Serious Mental Illness,” released by the National Association of State Mental Health Program Directors (NASMHPD).
The report documents striking evidence from state studies showing that people with serious mental illness die on average 25 years earlier than the general population and that about 60 percent of these premature deaths are from natural causes such as cardiovascular and pulmonary disease.
On the basis of that evidence, the report urges that this population be included in the federal Health Research and Services Administration's Health Disparities Collaborative. That initiative is designed to reduce disparities in health outcomes for poor, minority, and other underserved populations.
The report also recommends changes to national health surveillance activities that would incorporate information about the health status of people with serious mental illness. In particular, the report calls for tracking of deaths and “key data elements” of morbidity in this population across states.
Psychiatrist Benjamin Druss, M.D., a consultant on the report, said its findings and recommendations are likely to be used as a model for other mental health advocacy organizations.
“The issue of the poor physical health and health care for people with serious mental illness has really come onto the clinical and policy radar screen in the last one or two years,” Druss told Psychiatric News. “This report is really the first to explicitly address this issue and certainly is the most comprehensive that has ever been written on the topic.
“The core message is derived from the President's New Freedom Commission report, which began with the statement that mental health is essential to overall health,” Druss said. “The NASMHPD report is addressing the corollary—that overall health is essential to mental health.”
He added that the recommendation that people with SMI be designated as a health disparities population is a recognition that the issue is one of fairness.
“The statistics on premature death were really the impetus,” Druss said. “These patients are dying younger, and it's a very troubling and unambiguous statistic. This issue is one of fairness in that a vulnerable population is dying younger and that makes it extremely compelling.”
The recommendation for new surveillance measures specific to this population is also significant. “It calls for monitoring at the state level of things like morbidity and mortality rates in this population,” he said. “You cannot do anything about a problem you are not tracking.”
Psychiatrist Dale Svendsen, M.D., medical director at the Ohio Department of Mental Health and co-author of the NASMHPD report, told Psychiatric News that the report grew out of an initial study of health outcomes for people with serious mental illness in Massachusetts. The study found that between 1998 and 2000, people aged 25 to 44 served by the department had a cardiovascular mortality rate 6.6 times that of the general population.
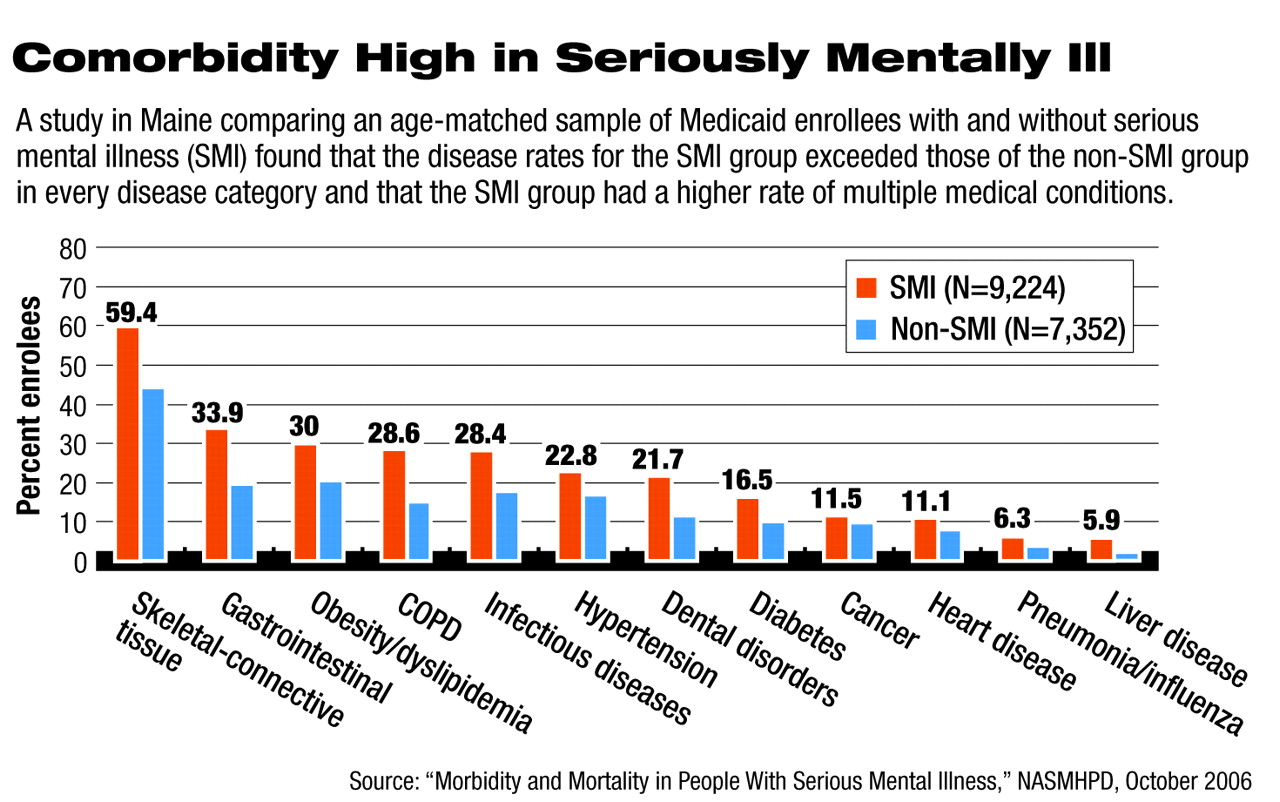
That study led to a 16-state report and separate studies in Ohio and Maine (see graph on
page 5) showing similar results.
“It was really a wake-up for all of us when we brought together a group of state medical directors and became aware that people with serious mental illness are dying 25 years earlier than the general population,” Svendsen said. “Here in Ohio, we looked at people over a six-year period who were discharged from our state hospital system. We had access to their inpatient records and all of their diagnoses, and we also looked at death records. We found that people who had been in our hospitals died at three times the expected rate with a loss of life of 32 years. The major reason for death was cardiovascular disease.”
The NASMHPD report is unequivocal about the role of antipsychotic medications in the development of metabolic syndrome among patients with serious mental illness and especially about problems with polypharmacy. In addition to specific recommendations for federal and state policymakers, the report has four broad recommendations for clinicians and health systems:
•
Adopt as policy that mental health and physical health care should be integrated.
•
Help individuals to understand the hopeful message of recovery, enabling their engagement as equal partners in care and treatment.
•
Support wellness and empowerment of persons being served, to improve their mental and physical well-being
•
Implement care-coordination models.
The last item entails having a specific practitioner in the mental health system who is responsible for ensuring that each person's needs for other kinds of medical care are being addressed and that all services are coordinated; and for ensuring that health-status assessment and planning are a part of treatment planning and goal setting for every person with serious mental illness.
Within each of those broad recommendations are extensive and detailed recommendations, especially regarding screening for metabolic symptoms and cardiovascular disease and counseling regarding lifestyle and behavior.
“Psychiatrists need to pay attention to weight, lipid levels, blood pressure, and exercise in our patients with serious mental illness,” Svendsen said. “The psychiatrist of the future is going to have to be more of a general physician than in the past, and our training programs are going to need to adapt.”