Results from two studies reported in the July American Journal of Psychiatry bolster the position that antidepressants prevent suicides, not cause them.
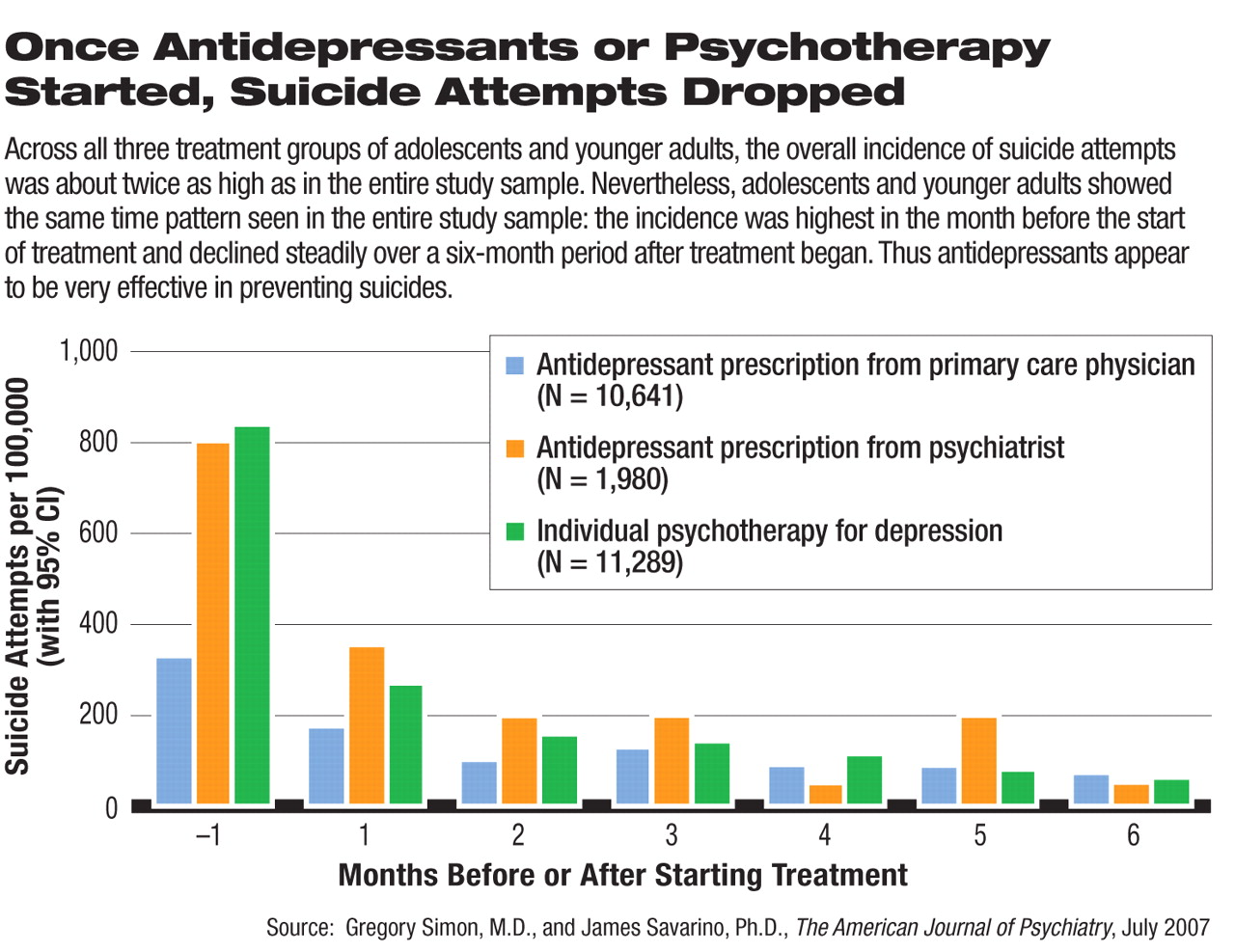
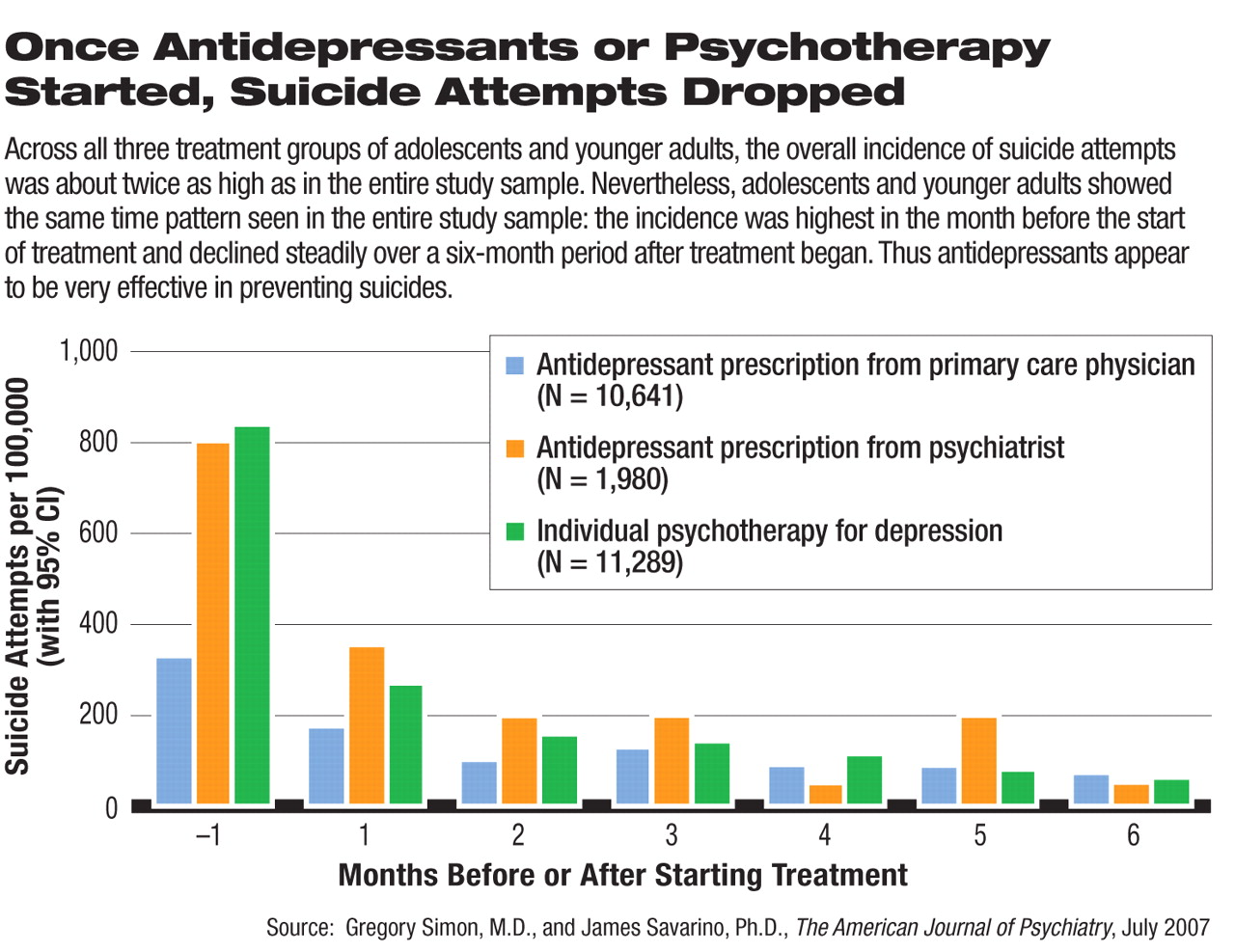
In the first study, two researchers at the Center for Health Studies of the Group Health Cooperative in Seattle—Gregory Simon, M.D., and James Savarino, Ph.D.—studied suicide-attempt patterns among 109,256 individuals in the Group Health Cooperative who were starting treatment for depression. The Group Health Cooperative is a prepaid health plan serving about 500,000 members in Washington state and northern Idaho. The individuals fell into three groups—those receiving antidepressants from a primary care doctor, those receiving antidepressants from a psychiatrist, and those receiving psychotherapy.
More notable, the researchers found the same time pattern of suicidal attempts in all three groups. The incidence was highest in the month before the start of treatment and declined steadily over a six-month period after treatment began.
The investigators then restricted their analyses to patients less than 25 years old, since concern about antidepressants possibly triggering suicides has focused primarily on that age group. Across all three groups, the overall incidence of suicide attempts was about twice as high as in the full subject sample. Nonetheless, adolescents and younger adults showed the same time pattern of suicidal attempts in all three groups as the full subject sample did.
The overall incidence of suicide attempts during the study period was highest among patients receiving antidepressant treatment from a psychiatrist; slightly lower among patients starting psychotherapy, and much lower among patients starting antidepressant treatment in primary care. “We do not interpret this difference as evidence that psychiatric care increases the risk of suicide,” Simon and Savarino wrote. “Instead, we would conclude that...patients at higher risk for suicide attempts are more often referred for psychiatric care.”
In the second study, Robert Gibbons, Ph.D., of the University of Illinois at Chicago, and coworkers studied 226,866 veterans diagnosed with depression during 2003 and 2004. They found not only a decrease in suicidal attempts among the subjects once treatment began, but also a lower rate of suicidal attempts in depressed veterans who took antidepressants compared with those who did not (see
VA Finds Antidepressants Reduce Suicide Risk).
“The study by Simon and colleagues is very interesting and helpful,” David Fassler, M.D., a clinical professor of psychiatry at the University of Vermont and an APA trustee-at-large, told Psychiatric News. “It confirms the general clinical consensus that treatment for depression, including treatment with medication, is associated with a significant reduction in suicide attempts. The take-home message is: if you think you're depressed, get help. Treatment works. The findings should be reassuring to physicians and patients.
“This study also highlights the growing concerns about the impact of the FDA's decision to add black-box warnings to all antidepressant medications. As a result of this action and the related media coverage, we've seen a precipitous decline in the use of these medications in the treatment of children and adolescents. Tragically, we've also seen the first increase in the actual adolescent suicide rate since the early 1990's.”
“These studies of treatment in actual clinical practice find a decrease in suicide attempts after treatment, regardless of whether the treatment is psychotherapy or drug therapy,” AJP Editor in Chief Robert Freedman, M.D., observed. “Patients and their doctors are concerned because of the FDA's black-box warning that antidepressants can cause suicide attempts. The studies in this issue provide more evidence that this side effect is rare, compared to the overall decrease in suicide attempts that occurs when treatment is initiated. Furthermore, suicide attempts in the first month of treatment [can] occur regardless of whether the treatment is psychotherapy or drug therapy, which suggests that these attempts are part of the natural evolution of symptoms in depression itself.”
Even though both studies bolster the position that antidepressants protect against suicide, not cause it, they do not rule out the possibility that antidepressants may increase suicide risk in a vulnerable subgroup of patients, Simon and Savarino stressed in their study report. The reason why, they explained, is that “randomized trials or large observational studies can only examine average effects.” “Given this uncertainty,” they concluded, “prescribers should certainly heed recommendations by the U.S. Food and Drug Administration to advise patients about their risk and to maintain close contact after patients start medication.”
The two studies were funded by the National Institute of Mental Health.
“Suicide Attempts Among Patients Starting Depression Treatment With Medications or Psychotherapy” and “Relationship Between Antidepressants and Suicide Attempts: An Analysis of the Veterans Health Administration Data Sets” are posted at<http://ajp.psychiatryonline.org> under the July issue. ▪