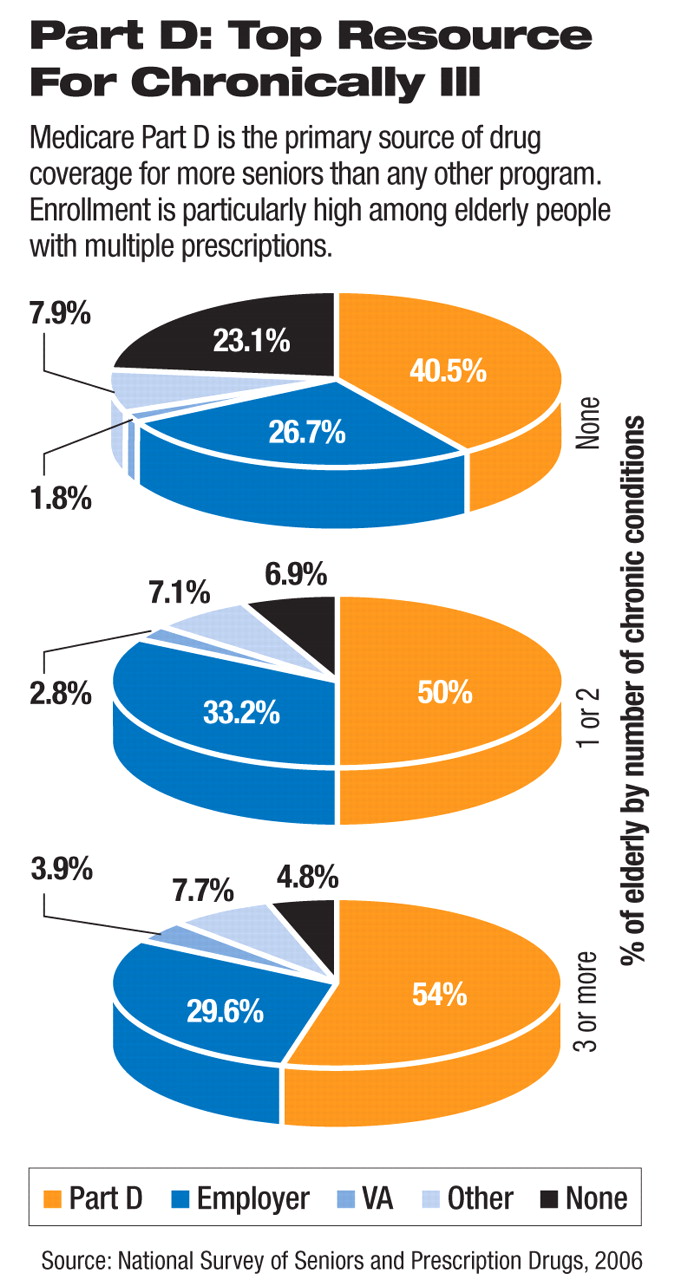
Senior citizens with chronic illness were more likely to receive prescription drug coverage through the Medicare Part D program, which began at the start of 2006, than through other options, but that program was likely to cost them significantly more than other coverage, according to a recent survey.
The results of the survey, conducted in fall 2006 by the Kaiser Family Foundation, Commonwealth Fund, and Tufts-New England Medical Center, were published in the August Health Affairs.
The survey included a national, random sample of more than 16,000 seniors and looked at their out-of-pocket spending and cost-related experiences, broken out by type of drug coverage, with a more in-depth look at the experiences of seniors with low incomes.
The survey found that a larger share of seniors in Part D than those in employer-sponsored or VA insurance programs spent more than $300 monthly, despite taking a similar or smaller number of medications. Part D enrollees were twice as likely to spend at least $300 monthly as seniors with employer-sponsored coverage, and they were three times as likely to do so as were VA beneficiaries.
The differing impact of drug costs on chronically ill enrollees was even more pronounced than among Medicare beneficiaries in general. Among seniors with multiple chronic illnesses, Part D enrollees took the same number of medications as others, on average, but spent “significantly more out of pocket” with significantly higher rates of cost-related nonadherence. The survey found that 11 percent of chronically ill Part D enrollees, 8 percent in employer plans, and 7 percent in the VA spent more than $300 monthly on prescriptions.
The survey results also indicated that older Americans enrolled in a Medicare Part D plan had more medication-access problems than those who relied on other sources of drug coverage, such as employer-sponsored coverage or benefits from the VA.
Part D enrollees decided against or delayed filling or refilling prescriptions at twice the rate of seniors who got their prescription coverage through employer plans or the VA. Part D enrollees were more than twice as likely as seniors in employer plans to delay or avoid filling or refilling prescriptions because of cost, which the researchers called“ cost-related nonadherence.”
The study authors said that more research is needed to clarify the reason for the higher spending by Part D beneficiaries, but they said it was likely attributable, in part, to the coverage gap that exposes Part D enrollees to 100 percent cost sharing after their total spending exceeds a certain threshold. The so-called “donut hole” coverage gaps are rare in employer-sponsored plans and are not a feature of VA benefits.
“We still have a lot of work to do to make sure that Medicare beneficiaries—particularly those who are most vulnerable because of low incomes or chronic illness—can get the drugs they need and are not subject to burdensome out-of-pocket costs,” said Karen Davis, president of the Commonwealth Fund, in a written statement.
Medication Switching Common
The survey reported that another notable change in Part D enrollees' prescription-drug practices was a high level of medication switching.
One-fourth of Part D enrollees reported switching to a cheaper medication than the one they were originally prescribed after they enrolled in a Part D plan, with little variation by income. The change included moving from a high-cost to a lower-cost brand-name drug or from a brand-name drug to a generic drug.
“The relatively high rate of switching to cheaper medications might be a function of beneficiaries moving into plans that use financial incentives (such as tiered copayments) and cost-management tools (such as step therapy) to steer enrollees toward lower-cost medications,” the survey authors said.
The survey also identified aspects of the Part D program that had a particular impact on the approximately 6 million low-income enrollees eligible for both Medicare and Medicaid, known as dual eligibles. Dual eligibles include many beneficiaries with psychiatric drug prescriptions. The survey found that 1 in 5 dual eligibles said they needed to obtain “special permission” from the Part D insurance plan that covered them to get a prescription filled, which was double the rate of higher-income Part D beneficiaries.
The researchers attributed the higher rate of special permission required for dual eligibles to the nature of the medications they are prescribed or their plan's use of tools such as prior authorization, which might restrict access to “the high-cost medications used disproportionately by dual eligibles.”
Many of the findings on access difficulties and higher costs reflected problems in the first year of the program identified in a study by the American Psychiatric Institute for Research and Education (APIRE), of psychiatric patients' experience with Part D. The study was the first to compile clinically detailed, national data on the impact of drug-plan management practices under Medicare Part D on dual-eligible psychiatric patients' medication access, compliance, and clinical outcomes (Psychiatric News, May 18 and July 20).
The APIRE survey of 1,183 psychiatrists in the first eight months of 2006 and another 1,600 in the last four months of that year reported clinically detailed information on one systematically selected, dual-eligible Part D patient under the care of each surveyed psychiatrist.
The study found that large numbers of patients had problems filling their prescriptions and that many psychiatrists reported changing or discontinuing their patients' clinically indicated medications rather than pursuing appeals or exceptions. A growing number of psychiatrists also had to ask drug plans for exemptions to their drug coverage rules so that patients could get needed psychotropic medications.
Other problems identified in the APIRE study were difficulty accessing medication refills and insurance-plan requirements to switch to a different medication because clinically preferred medication refills were not covered or approved.