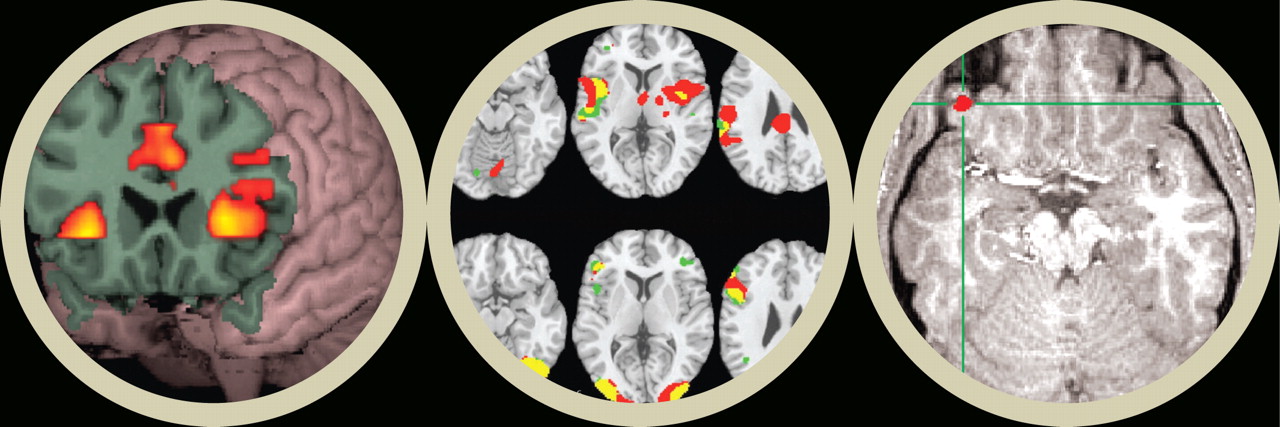
Scientists working in psychiatric brain imaging are obtaining spectacular snapshots of the living human brain.
For example, they can see the hippocampus of a posttraumatic stress disorder patient glow as she experiences a flashback. They can see the basal ganglia and prefrontal cortex of a Tourette's syndrome patient brighten as he emits grunts or curses. They can see the visual cortex of a schizophrenia patient light up while he “experiences” a decapitated head issuing commands. But what is the point of all this? What has the field achieved so far?
It all started a quarter century or so ago. Two brain-imaging techniques—computed tomography (CT) and single photon emission computed tomography (SPECT)—became available and allowed psychiatrists to peer into the living human brain as they had never been able to do before. CT and SPECT were then followed by magnetic resonance imaging (MRI) and positron emission tomography (PET). And then in the early to mid-1990s, functional magnetic resonance imaging (fMRI) made its debut.
“Today, with some strong MRI scans, we can see down to the neural column level, which is really incredible,” Anthony Weiss, M.D., a Massachusetts General Hospital psychiatrist doing brain imaging of schizophrenia subjects, noted. “So these are beautiful pictures with exquisite detail of the brain.”
And as David Silbersweig, M.D., codirector of the Functional Neuroimaging Laboratory at Cornell Medical Center, pointed out at a recent meeting of the American Psychoanalytic Association, “What is so exciting about functional imaging is that we can make linkages between brain and mind.”
These advances have led to a plethora of valuable insights into the biological underpinnings of psychiatric disorders. For example, the orbitofrontal cortex and amygdala have been implicated in certain anxiety disorders. The negative symptoms of schizophrenia have been coupled with decreased activity in the dorsal lateral prefrontal system of the brain. There is a raft of neuronal underconnectivity in the brains of children with autism.
Neuroimaging scientists are also starting to see a synthesis of some of these findings. For instance, the amygdala appears to be a culprit in a number of psychiatric disorders associated with negative emotional states. The anterior cingulate gyrus and some regions of the frontal lobe have been implicated in both anxiety disorders and mood disorders. “These are probably parts of final common pathways of symptom expression that may not respect DSM boundaries,” Silbersweig told Psychiatric News.
Yet neuroimaging is not yet a clinical psychiatry tool. “The translation to clinical practice has actually not worked out as well as we had hoped,” Weiss observed. As Joshua Roffman, M.D., an instructor in psychiatry at Harvard University who is combining neuroimaging with genetics, added: “I don't want to knock imaging because it has helped us understand [mental illnesses] better, but it hasn't translated yet to the point where it is clinically useful. And many of us who are working with it are still aiming for that goal.”
So Why the Delay?
“Although it looks as if the technique is easy from the colorful brain pictures that result, actually it is not,” Silbersweig pointed out. “We take thousands of pictures and use statistics to test hypotheses. It is not just an expensive toy that lights up the brain. Also, one is dealing with some of the most complex functions in the most complex organ, and there is a lot of groundwork that needs to be laid to be able to progress rationally toward evidence-based clinical practice advances. Furthermore, it is an interdisciplinary field involving lots of high-tech equipment and therefore expensive work. So there are always issues of funding so that the field can move ahead.”
“To some degree there is a communication gap between researchers doing high-level imaging work and clinicians who are seeing patients,” Weiss explained. “Also, it can be difficult to frame imaging research in a way that can be more immediately relevant. In fact, sometimes if you want to make your research more clinically relevant, it can reduce the scientific quality of the study.”
Nonetheless, he said, imaging researchers should probably be focusing more on the clinically pertinent aspects of their work than they are currently doing. For example, a 2005 neuroimaging study impressed him because the researchers asked: “What would the sensitivity and specificity of this neuroimaging test be if it were used to diagnose schizophrenia?”
“One rarely sees such clinically relevant messages in papers about imaging and mental illness,” he said.
There is often a “disconnect between the clinical features of psychiatric illnesses and their biological underpinnings,” Gary Small, M.D., a professor of psychiatry at UCLA and an Alzheimer's brain-imaging scientist, observed. “Therefore it is hard to find informative surrogate markers. And that is what we need” if psychiatrists want to use imaging for diagnosis or to determine who is going to respond to treatment or to track whether treatment works.
Nonetheless, what most clinical psychiatrists want to know is, When will imaging research start benefiting their practices?
Alzheimer's Progress Encouraging
“I think that the work done Alzheimer's disease is further along than in any other area in terms of using imaging,” Weiss said. “Some scientists are now able to detect the plaques occurring in nerve cells while Alzheimer's patients are still alive. And that is a tremendous advance that has happened over the past 10 years.”
In fact, a brain-imaging test for Alzheimer's could become clinically available as early as four years from now, Small predicted. Specifically, Small and his colleagues have developed a radioactively labeled molecule (probe) called FDDNP that makes plaques visible on PET scans (Psychiatric News, September 6, 2002). FDDNP has been patented by UCLA and licensed to Siemens. Siemens has filed an investigational new drug application with the Food and Drug Administration, and if studies with FDDNP are further successful, it “could have FDA approval within four years,” Small said.
Some other clinical applications of imaging may also surface during the next five to 10 years.
Using brain imaging to predict treatment response is one, Weiss contended. Melissa DelBello, M.D., an associate professor of psychiatry at the University of Cincinnati and a brain-imaging investigator, believes this as well. Currently, DelBello and her colleagues are using SPECT and fMRI to identify predictors of treatment response in subjects with bipolar illness.
Roffman and Silbersweig, in fact, foresee brain imaging being combined with genotyping to predict treatment response. So does Weiss: “I think it is the wave of the future. These two streams—genetics and neuroimaging—have flowed throughout psychiatric research over the past 20 years, and they are starting to be brought together.”
Combining brain imaging with genotyping will achieve something else important, Konasale Prasad, M.D., an assistant professor of psychiatry at the University of Pittsburgh, said. It will lead to the identification of certain subgroups of mental disorders, and once such subgroups are identified, then treatments can be customized for them. “The use of neuroimaging to provide biomarkers and targets for novel therapeutics is an important goal,” Silbersweig said.
As neuroimaging unmasks the biology of various psychiatric disorders, still other clinical applications will undoubtedly emerge.
Take the case of autism. Even though autism research is often considered to be many years behind that for other types of psychiatric disorders, brain-imaging research in autism may eventually lead to some clinical applications, Nancy Minshew, M.D., a professor of neurology and psychiatry at the University of Pittsburgh and an autism expert, anticipates. For instance, since brain imaging has revealed underconnectivity of nerve cells in the brains of autism subjects, she and other autism scientists are devising new interventions for autism based on this finding—“the translation of this research,” she said.
And as new brain-imaging technologies develop, they could give the clinical application of psychiatric brain imaging a huge push.
A case in point is near infra-red spectroscopy (optical imaging). Like fMRI, it shows which areas of the brain are activated when someone is participating in a task or resting. But whereas a magnetic field does the job in the former, light does it in the latter.
What is especially tantalizing about optical imaging, both Roffman and Weiss believe, is that it is much less expensive and much more portable than fMRI. In fact, an optical-imaging unit is small enough to put on a cart and wheeled around in a psychiatrist's office. Thus, it could be used as an adjunct to psychiatrists' century-old diagnostic tools—questioning and observation. ▪