Since nerve growth factor was identified half a century ago, other chemicals that stimulate nerve development have been discovered as well. One is brain-derived neurotrophic factor (BDNF). BDNF is not just the most ubiquitous growth factor in the brain; it seems to be involved in a number of mental illnesses as well, investigators are finding.
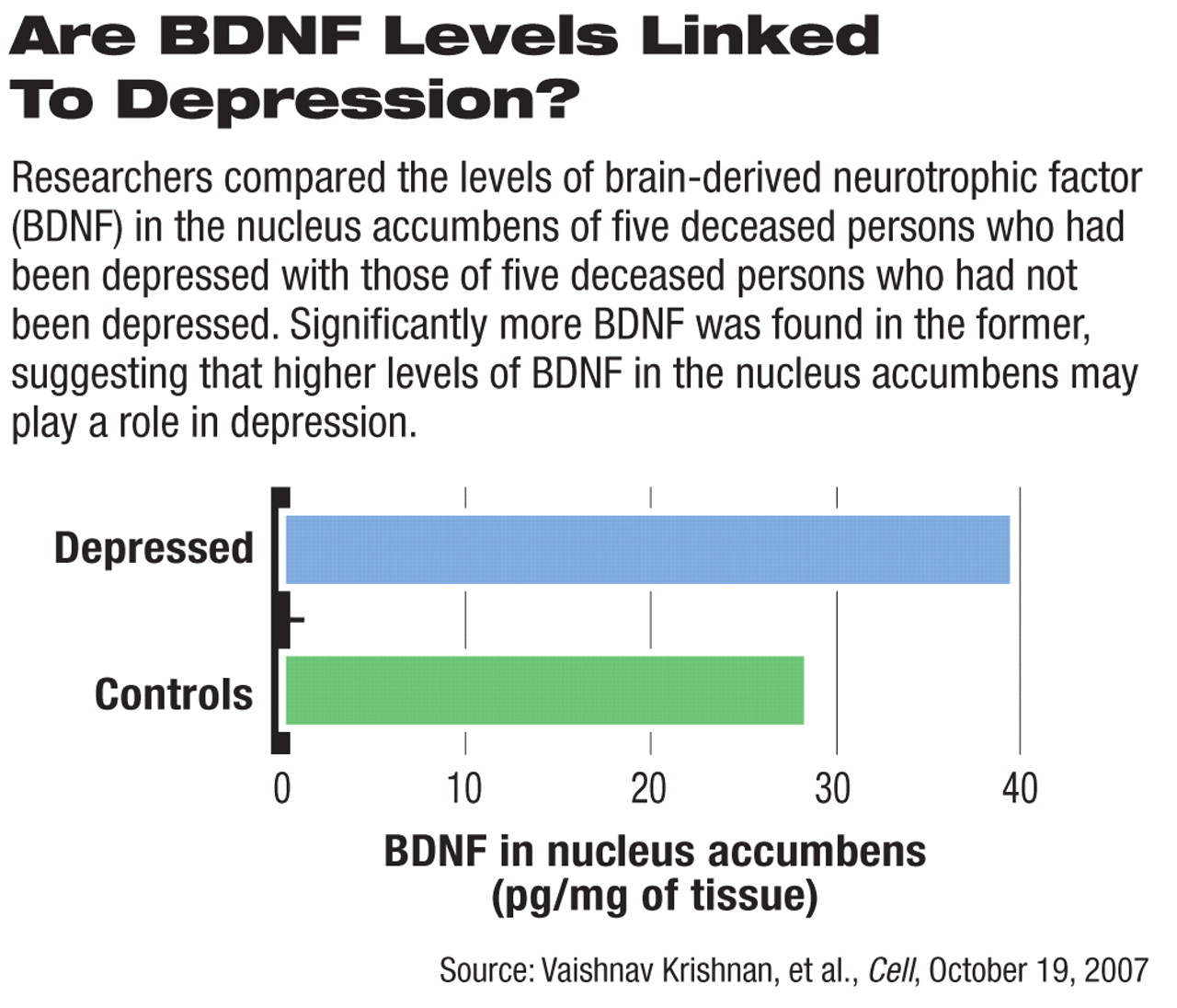
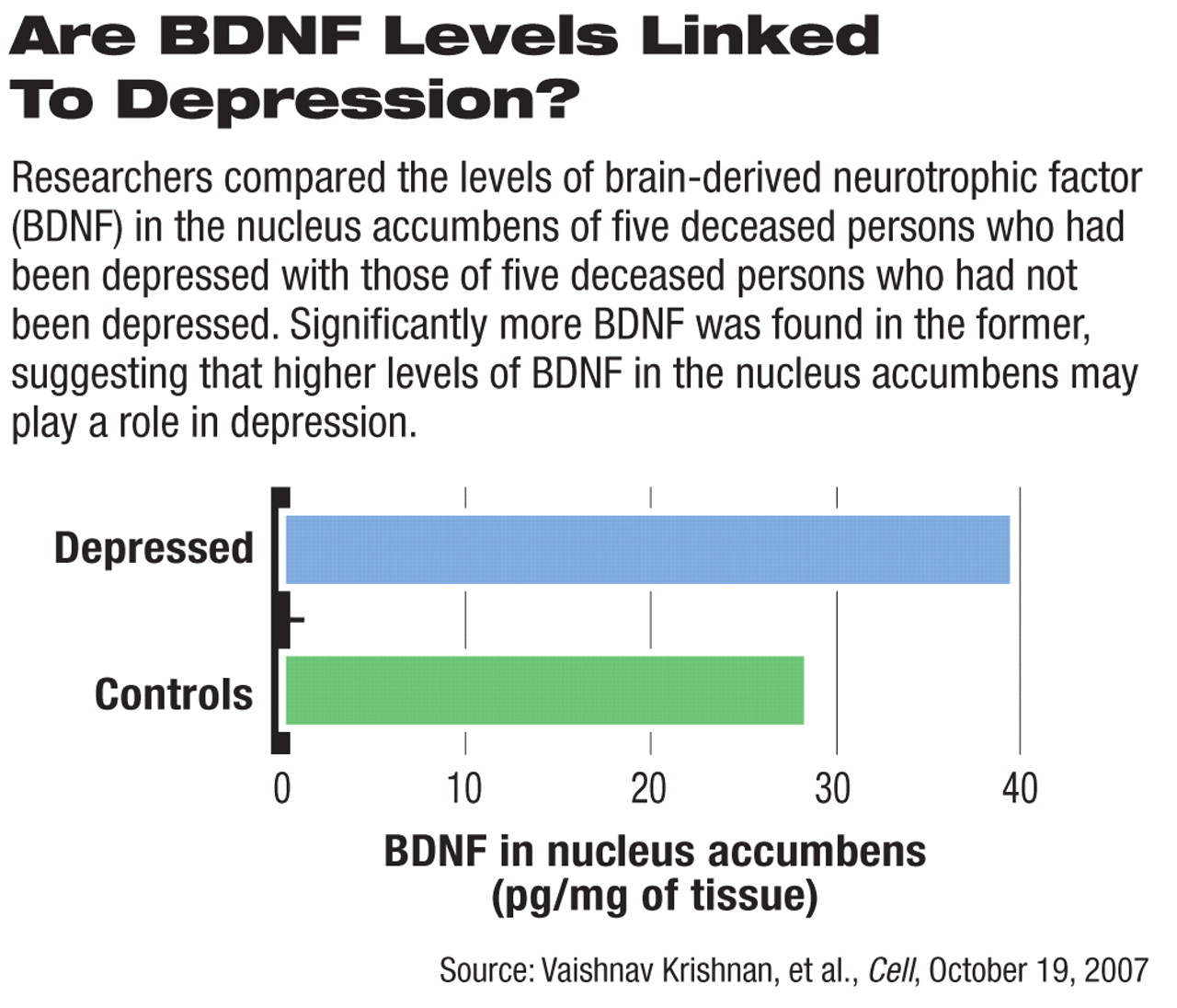
For example, untreated depressed persons have been found to have unusually low levels of BDNF in their blood, and low levels of BDNF in the hippocampus have been linked with depression (Psychiatric News, December 19, 2003). In contrast, having ample amounts of BDNF in a reward center of the brain—the nucleus accumbens—may contribute to depression, not counter it. Vaishnav Krishnan, an M.D.-Ph.D. student at the University of Texas Southwestern Medical Center, and colleagues compared brain tissue from deceased persons with and without a history of depression and found significantly higher levels of BDNF in the former's nucleus accumbens. They reported their findings in the October 19 Cell.
High levels of BDNF in the nucleus accumbens also seem to contribute to stress susceptibility. During stressful situations, Krishnan and his colleagues found, stress-susceptible mice experienced excessive nerve firings in the ventral tegmental area of the brain, and this excessive firing in turn led to a flooding of BDNF into the nucleus accumbens.
BDNF has also been implicated in some other psychiatric illnesses. For example, decreased levels of BDNF have been found in the blood of patients with eating disorders. And now Beng-Choon Ho, M.D., of the University of Iowa and colleagues reported in the December American Journal of Psychiatry that “a particular version of the BDNF gene may be one of several factors affecting progressive brain-volume changes in schizophrenia.”
Specifically, there are two versions of the BDNF gene—the methionine (met) version and the valine (val) version. The researchers grouped 119 subjects with recent-onset schizophrenia according to which version the subjects possessed. They then measured the size of the subjects' brain volumes over the next three years. They found that subjects with the met gene version had significantly greater reductions in frontal gray matter volume than did the subjects with the val version.
These various BDNF findings have clinical implications. For instance, antidepressants are known to increase the level of BDNF in the blood and in the hippocampus. “Pharmacological strategies that increase BDNF bioavailability and enhance the neuroplastic effects of BDNF could potentially begin to address the currently unmet need for interventions that curb brain-volume reduction in schizophrenia,” Ho and his group wrote in their report. And Krishnan and his group have found something especially provocative—they were able to enhance resistance to stressful situations in stress-susceptible mice by blocking BDNF action in their nucleus accumbens.
Specifically, they infused a virus into the mice's nucleus accumbens that overexpressed a particular gene. This gene in turn blocked BDNF action. This viral-mediated-gene-transfer technique has also been used on some humans—patients with severe cases of Parkinson's disease or Huntington's disease, with some success, Krishnan said during an interview. However, it is a complicated surgical technique that would not be appropriate for patients with psychiatric disorders, he said. Nonetheless, now that he and his colleagues have identified BDNF's link with stress susceptibility in the nucleus accumbens, drug companies could try to develop drugs to block BDNF's action there, he said. Such drugs, he believes, might reduce susceptibility to psychological stress in stress-sensitive individuals and thereby help shield them from depression, posttraumatic stress disorder, or other psychiatric conditions triggered by stress.
An abstract of the research conducted by Krishnan and his group,“ Molecular Adaptations Underlying Susceptibility and Resistance to Social Defect in Brain Reward Regions,” is posted at<www.cell.com/content/article/abstract?uid=PIIS0092867407012068&highlight=Kri...>. The article by Ho and his colleagues, “Association Between Brain-Derived Neurotrophic Factor Val66Met Gene Polymorphism and Progressive Brain Volume Changes in Schizophrenia,” is posted at<http://ajp.psychiatryonline.org> under the December issue. ▪