When the Food and Drug Administration (FDA) warned clinicians that antidepressants may increase the risk of suicidality in pediatric patients in 2003, the agency also urged clinicians to closely monitor patients, especially those who are started on these medications, for signs of suicidal ideation. The evidence suggests, however, that the recommendation is often not followed. Patients who were put on antidepressants did not seem to receive more vigilant care from their health care providers, according to a study published in AJP in Advance on November 6.
The effect of the FDA public health advisory and subsequent black-box warning for all antidepressants received extensive attention in the lay media, and clinical practice changes followed. The number of patients, including children and adults, taking these medications has declined ever since (Psychiatric News, September 7, 2007).
Researchers from the University of Colorado at Denver and University of Pittsburgh analyzed a large managed care claims database to determine how frequently patients on antidepressants visited their health care providers between October 1998 and March 2005. They compared visit patterns with the depression-treatment standards recommended by the National Committee on Quality Assurance's Health Plan Employer Data and Information Set (HEDIS) metric.
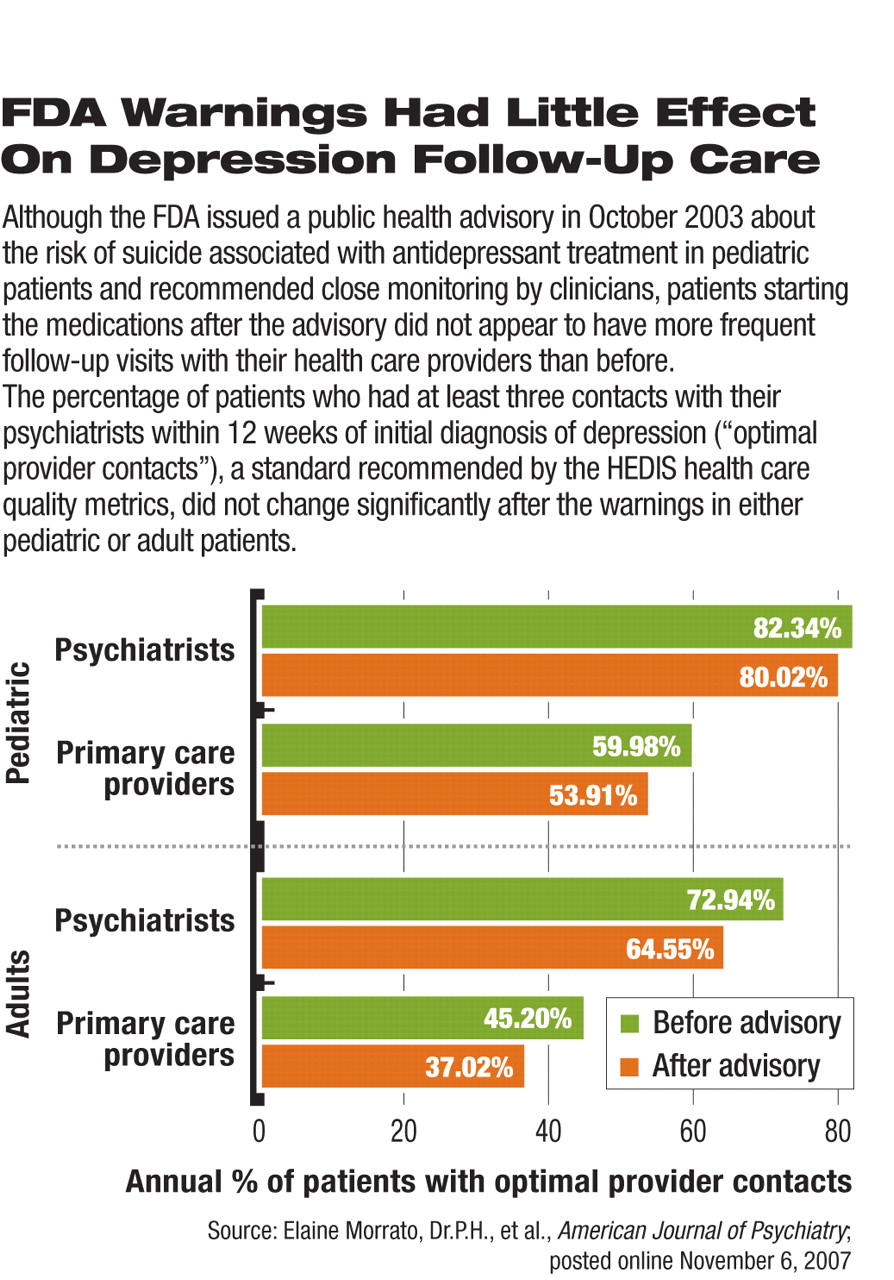
There were no statistically significant changes in the percentage of pediatric patients who had received “optimal practitioner contacts” before and after October 2003, when the FDA issued the antidepressant advisory. The percentage of adult patients who had follow-up visits as recommended was even lower than that for children.
The HEDIS metric defines optimal practitioner contacts as at least three contacts with care providers in the first 12 weeks after the initial antidepressant prescription. Billable telephone contacts were considered a valid visit.
“We had expected some change in the intensity of monitoring after the FDA's advisory,” said Robert Valuck, Ph.D., a coauthor of the study.“ We were surprised by the findings given the immediate and accelerated drop in the diagnosis and overall treatment of depression and all the media attention and scrutiny.”
The same group of researchers had found that after the FDA advisory was issued in 2003, fewer diagnoses of depression were made and, for those who were diagnosed with new episodes of depression, any treatment decreased as well (Psychiatric News, August 3 and September 7). They found no compensatory increase in treatment alternatives such as psychotherapy to accompany the plunge in antidepressant prescriptions.
Meanwhile, it appears that patients who were prescribed antidepressants in this period did not receive more frequent care from their treatment providers despite the FDA's recommendations. “Our data don't answer why,” he said. The authors suggested a number of possibilities, including obstructed access to care, logistical difficulties in arranging for more frequent visits, and insurance-plan restrictions.
The HEDIS quality indicators were derived from expert consensus on clinical practice; the depression-specific indicators have been tracked since 1998. This study found that the quality of follow-up care for patients newly diagnosed with depression, at least in terms of contact frequency between clinicians and patients, did not change significantly after the FDA warnings about increased suicide risk.
The FDA recommended a more intensive schedule (seven visits in the first three months) of follow-up care in a medication guide released in 2003. This recommendation was removed in a revision to the guide earlier this year after psychiatrists complained about the lack of clinical evidence to support this stepped-up schedule.
Trends in follow-up care remained consistently flat across specialties. The study authors found that more psychiatrists kept up with antidepressant monitoring compared with other types of providers. About 80 percent of pediatric patients seen by psychiatrists had follow-up visits that met the HEDIS standard, a percentage higher than those seen by pediatricians (60 percent) and primary care physicians (54 percent). However, changes in the rates of meeting the HEDIS optimal practitioner contact standard before and after October 2003 were not statistically significant within each provider type, indicating a lack of influence on practice by the FDA advisory.
Included in the analyses were more than 27,000 pediatric patients and 193,000 adult patients in the managed care claims database who had a new episode of depression and received antidepressant medication within 30 days of the diagnosis. A new episode of depression was defined as having no depression-related diagnosis during the 120 days before the diagnosis and no antidepressant prescription claims during the 90 days before. “We have a robust dataset that is representative of national managed care populations and trends in clinical practice,” said Valuck.
According to data recently released by the Centers for Disease Control and Prevention, suicide rates among youth increased by 8 percent from 2003 to 2004, which paralleled the drop in antidepressant prescriptions after the FDA warning (Psychiatric News, October 5). The public health effects of the mandated black-box warnings for antidepressants are still hotly debated.
“Frequency of Provider Contact After FDA Advisory on Risk of Pediatric Suicidality with SSRIs” is posted at<ajp.psychiatryonline.org/cgi/reprint/appi.ajp.2007.07010205v1>.▪