Cognitive-behavioral therapy (CBT), whether combined with fluoxetine or placebo, is highly effective in treating major depressive disorder in adolescents who also have a substance use disorder (SUD) and conduct disorder, according to a randomized, double-blind study by researchers from the University of Colorado at Denver.
While medication was a little more effective than placebo in reducing depressive symptoms, giving a placebo along with weekly CBT sessions designed to treat substance use problems worked almost as well.
The authors, led by Paula Riggs, M.D., an associate professor at the Department of Psychiatry at the University of Colorado, enrolled 126 adolescents between 13 and 19 years old who were diagnosed with major depression as well as SUD and conduct disorder. Based on the participating physicians' overall assessment, 67 percent of the 63 patients in the placebo-plus-CBT group and 76 percent of the 63 patients in the fluoxetine-plus-CBT group were deemed “very much improved” or“ much improved” after being treated for four months.
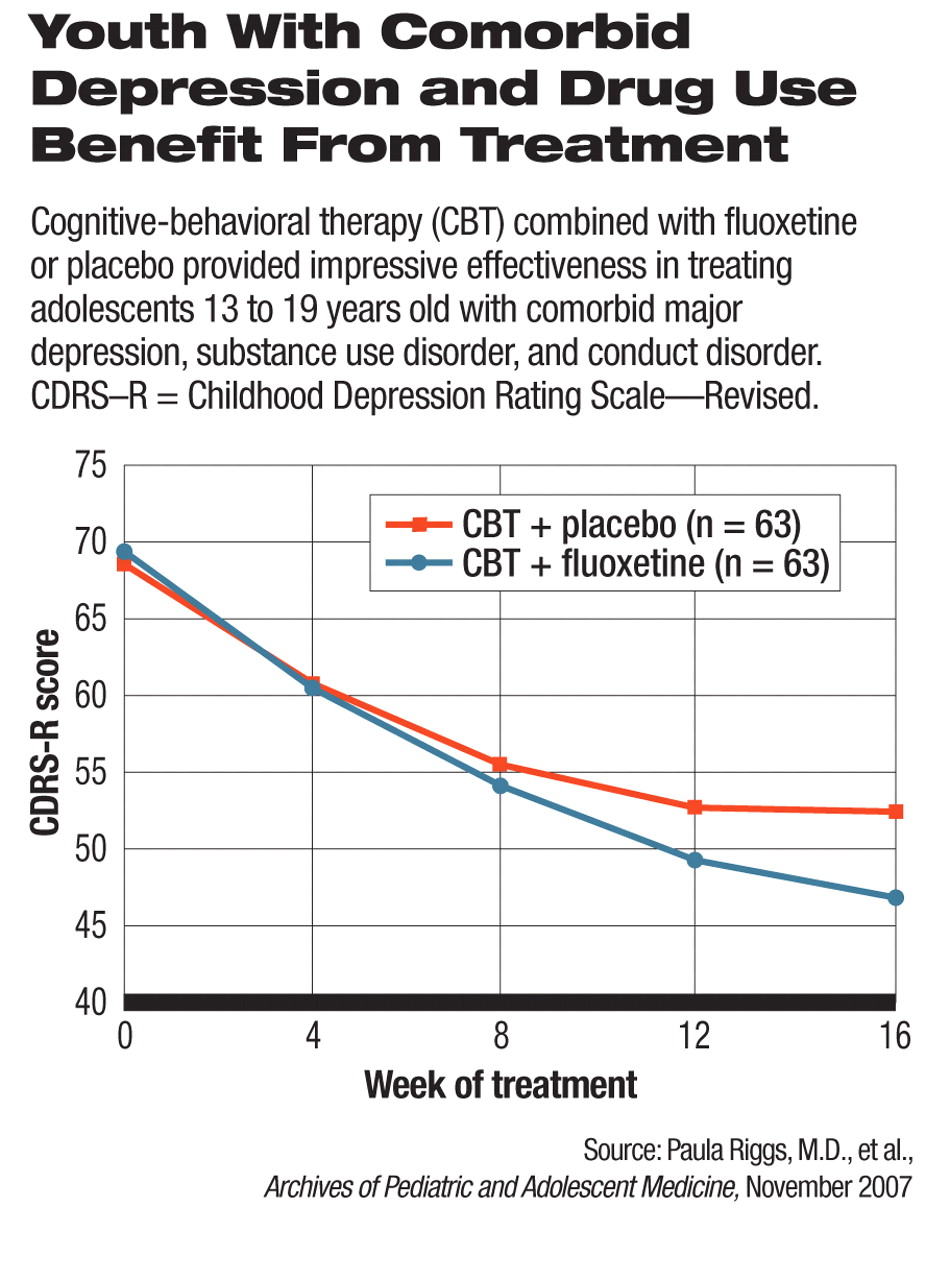
The difference in effectiveness between fluoxetine and placebo was not statistically significant in terms of physicians' ratings of symptom improvement, but was statistically significant in scores of the Childhood Depression Rating Scale—Revised (CDRS-R), an overall rating of depression severity based on a clinician-conducted, semistructured interview with the patient. About 69.8 percent of patients in the fluoxetine-CBT group and 52.4 percent of the placebo-CBT group reached remission for their depression (defined as CDRS-R score of 28 or less); this difference did not reach statistical significance.
Some study participants were recruited from the social-service and juvenile-justice systems. The authors pointed out that most large, controlled clinical trials of antidepressants in young patients exclude those with substance use disorders despite the high rates of comorbidity. Because of the lack of research data, “clinicians are often reluctant to prescribe antidepressants for depressed adolescents with SUD” and “such youths are...expected to complete substance treatment and achieve...abstinence before antidepressant medication is considered.”
The study was published in the November 2007 Archives of Pediatric and Adolescent Medicine and was funded by National Institute on Drug Abuse (NIDA) grants.
Understudied Population Assessed
“Adolescents with major depression, substance abuse, and behavior problems may be a clinically complex group, but unfortunately not an uncommon one,” said Christopher Kratochvil, M.D., a child psychiatrist at the University of Nebraska Medical Center. “The investigators should be congratulated for the clinically relevant and important work with this understudied patient population.”
According to survey data compiled by NIDA, the rate of illicit drug use (use of such drugs at once within the prior month) in 2006 was 16.8 percent in 10th graders and 21.5 percent in 12th graders. Another study published in the same issue of Archives of Pediatric and Adolescent Medicine by a group of Massachusetts researchers found, through screening in the primary care setting, that 14.8 percent of adolescents between ages 12 and 18 had substance use problems. Many of these youths have comorbid psychiatric disorders and have little access to mental health treatment until they are picked up by the social-service or juvenile-justice systems, Riggs told Psychiatric News. “About 80 percent of the study participants were not court-mandated and came voluntarily, but they were just as sick [in terms of] substance use disorders. They cannot afford treatment, and their parents cannot afford it, and they haven't entered the social or criminal-justice systems that pay for treatment.”
Offer It, and They Will Come
The researchers were surprised by the high rates of treatment compliance and completion by the youth in the study. Of the 126 participants, only six were lost to follow-up, and two withdrew consent; 12 could not complete because they went to jail or residential facilities, or moved out of the area.“ It really begs the question of whether we as a society ought to offer free treatment to these kids,” said Riggs. “If you offer the treatment, they will come.”
In this study patients received weekly, standardized, one-hour CBT sessions specifically targeting SUD, not depression. The youth learned cognitive and behavioral techniques to better manage the negative thoughts and feelings that can trigger substance use, with the goal of reducing such use. “It's clear the coping skills, the empathic approach, the weekly monitoring...of CBT were very effective,” said Riggs. The high rates of response and remission in the placebo-CBT group might have obscured the impact of fluoxetine on depression, the authors suggested in their report.
The participants' self-reported frequency of substance use and conduct disorder symptoms went down in both treatment groups during the study. The placebo-CBT group actually improved a little more on average in terms of SUD and conduct disorder outcomes than did the fluoxetine-CBT group, but the differences were not statistically significant. “In the context of CBT and controlling for fluoxetine use, we found that remission from depression was a significant predictor of decreased substance use,” said Riggs.
Integrated Treatment Needed
Riggs urged physicians to provide integrated, not sequential, treatment for comorbid mental health issues and drug abuse problems. Adolescents with such comorbidities responded to treatment in rates as high as those without these comorbidities in depression studies, and the safety and efficacy of combined CBT and fluoxetine were satisfactory, she pointed out.
This finding should convince clinicians not to wait for patients to stop substance use before they initiate depression treatment. “Start with CBT, but if they don't respond to the treatment in a month or so, physicians shouldn't hesitate to add fluoxetine to treat the depression,” she concluded.
An abstract of “A Randomized Controlled Trial of Fluoxetine and Cognitive-Behavioral Therapy in Adolescents With Major Depression, Behavioral Problems, and Substance Use Disorders” is posted at<archpedi.ama-assn.org/cgi/content/abstract/161/11/1026>. An abstract of “Prevalence of Positive Substance Abuse Screen Results Among Adolescent Primary Care Patients” is posted at<archpedi.ama-assn.org/cgi/content/abstract/161/11/1035>.▪