Sixty percent of military members believe that seeking help for mental health problems would have a negative impact on their careers, according to new data from a survey of military members and their families released by APA in April.
The survey also found that almost 60 percent of military members and 66 percent of their spouses acknowledge having little or no knowledge about common warning signs of or treatment options for mental health problems that may result from serving in a war zone.
“We need to do a better job of educating military personnel and their families about mental health issues,” declared then-APA President Carolyn Robinowitz, M.D., at a press conference in Washington, D.C., to announce the findings. Robinowitz noted that the vast majority of military respondents (90 percent) and their spouses (83 percent) agreed that mental illnesses can be successfully treated.
Additionally, most military members (67 percent) and military spouses (54 percent) said they rarely or never talk about their mental health with family or friends.
The survey was conducted online in March by Harris Interactive on behalf of APA and included 191 military personnel and 113 spouses of military personnel randomly chosen from a Harris Online Poll of military members and their spouses.
Military members were defined as adults aged 18 to 54 who are former or current members of the U.S. armed forces including active, Reserve, and National Guard, or who have been deployed to a war zone since 2001.
In regard to the mental health problems experienced by survey respondents, one-third of military members (33 percent) and spouses (33 percent) said they typically feel very stressed or stressed.
Reported symptoms included difficulty sleeping, anxiety, lack of interest in daily activities, and depressed feelings. In addition, 60 percent of military spouses reported facing stress due to having to handle domestic issues alone.
Military spouse and mother Monique Rizer, who spoke at the press conference, experienced such stress after her husband was deployed to Iraq. Said Rizer, “We had two small children at home, and the rest of my family was spread across the country, so I began to feel very isolated.”
Rizer experienced other problems due to stress and took advantage of free counseling sessions offered by the military, which helped her to cope effectively. She also attended support groups with other military spouses and noted that many of them had been experiencing the same emotions and other symptoms she'd been experiencing. “I would never have known that if I didn't attend the group,” Rizer said.
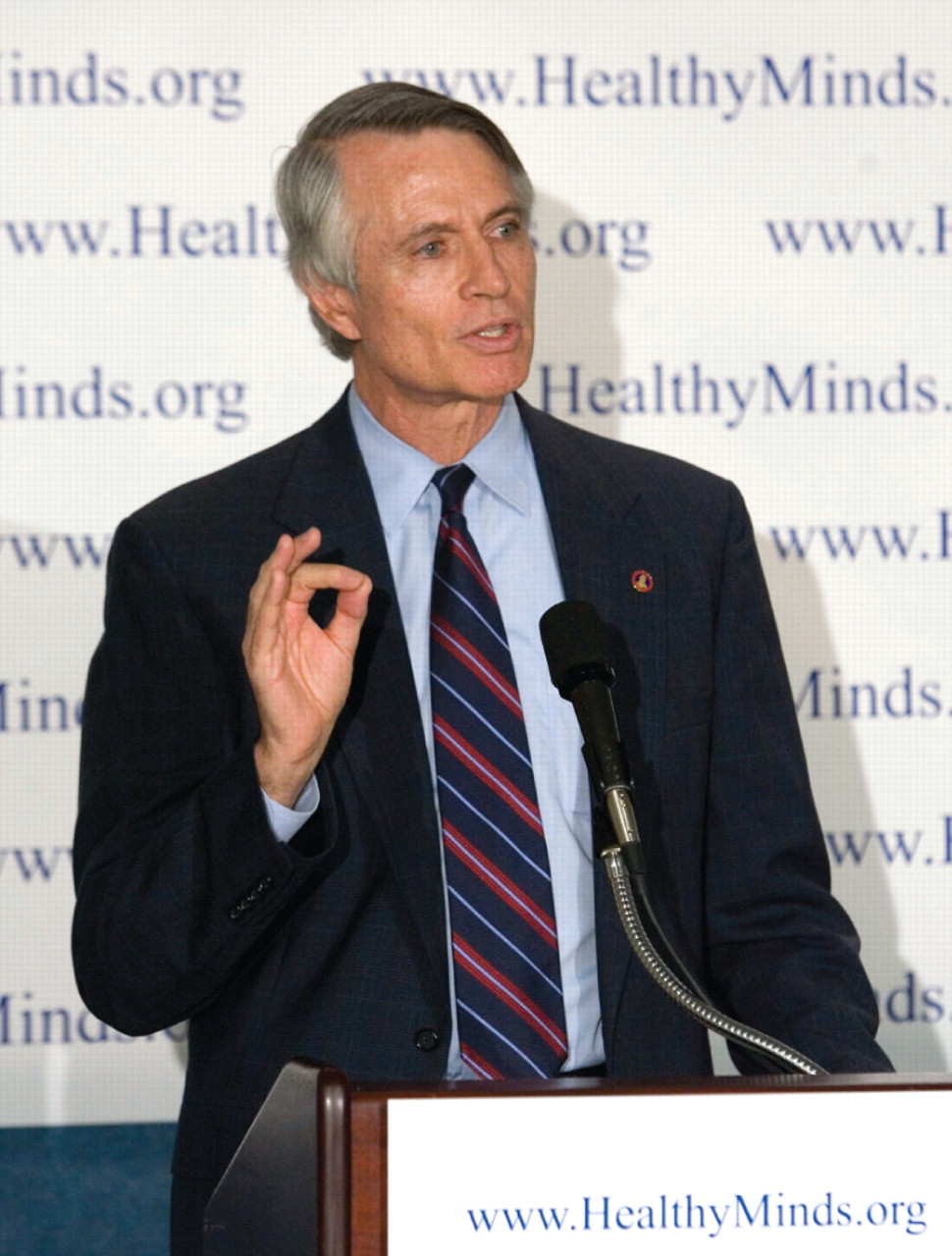
American Psychiatric Foundation President Richard Harding, M.D., noted that it is crucial to make mental health services readily available to military personnel and their families. “We must expand mental health services for military personnel and their dependents, who are dealing with longer deployments and shorter periods of respite between deployments” than many of their peers did in earlier years, he said.
Harding, a child and adolescent psychiatrist and a former Navy officer, helped treat a number of young Vietnamese refugees who came to the United States in 1975. “I saw the human consequences of war” in the child refugees, he recalled. Harding is also a past president of APA.
To respond to the mental health care needs of Iraq and Afghanistan combat veterans, many of whom have difficulty accessing care, APA has partnered with the organization Give an Hour, in which psychiatrists and mental health professionals volunteer their time to provide services to military members and their families, Harding pointed out (Psychiatric News, March 7).
Clarence Jordan, a 15-year Navy veteran with major depression, was also on hand to describe how effective psychiatric treatment has been for him.
“Consequences of my untreated mental illness ultimately led me to leave the navy and, most regrettably, my two children,” said Jordan. Jordan said that for about a decade, he bounced from city to city and job to job, until he began to seek treatment after becoming involved in the criminal-justice system. He is now a member of the Board of Directors of the National Alliance on Mental Illness (NAMI).
“Through my work with NAMI, I've seen countless people overcome mental illness and, with appropriate support and treatment, go on to lead meaningful lives,” he said.
The survey report, “Mental Health Among Military Members and Spouses,” is posted at<www.healthyminds.org>.▪