Since the dawn of hunting and gathering, some people have always gathered more than others and just couldn't bear to part with it.
When such behavior crosses the line from the eccentric into the DSM-IV realm, it becomes a symptom—hoarding—the compulsion to acquire objects coupled with an unwillingness to discard them.
Hoarding may occur in connection with a number of psychiatric disorders, but it is most commonly associated with obsessive-compulsive disorder (OCD). Perhaps 30 percent to 40 percent of people with OCD have hoarding symptoms. Specialists argue over the relationship between OCD and hoarding. Is the latter merely a symptom of the former, or should the two be considered separate syndromes?
“There's a real discussion in the field about where hoarding goes,” said Jack Samuels, Ph.D., a psychiatric epidemiologist and an assistant professor of psychiatry at Johns Hopkins, in an interview with Psychiatric News. “People with OCD and hoarding have more severe symptoms, show more symmetry or ordering obsessions, and respond less well to treatment than those who hoard but do not have OCD.”
Recent studies have sought answers from several directions.
In the March 2007 American Journal of Psychiatry, Samuels and colleagues from five other sites published a genetic study of 219 families with OCD-affected sibling pairs and their first- and second-degree relatives. They found a significant linkage on chromosome 14 to compulsive hoarding behavior when they compared families with at least two hoarding relatives with families with only one or no hoarders. Other researchers have found linkages on chromosome 9 and chromosome 3.
Neuroimaging shows varying results too. “Obsessive-compulsive hoarding may be a neurobiologically distinct subgroup or variant of OCD whose symptoms and poor response to antiobsessional treatment are mediated by lower activity in the cingulate cortex,” wrote Sanjaya Saxena, M.D., and colleagues in the June 2004 American Journal of Psychiatry.
A more recent study, in the January 8 Molecular Psychiatry, by David Mataix-Cols, M.D., and colleagues found that when challenged, OCD patients with prominent hoarding symptoms showed greater activation in the bilateral anterior ventromedial prefrontal cortex than did patients without hoarding symptoms and healthy controls.
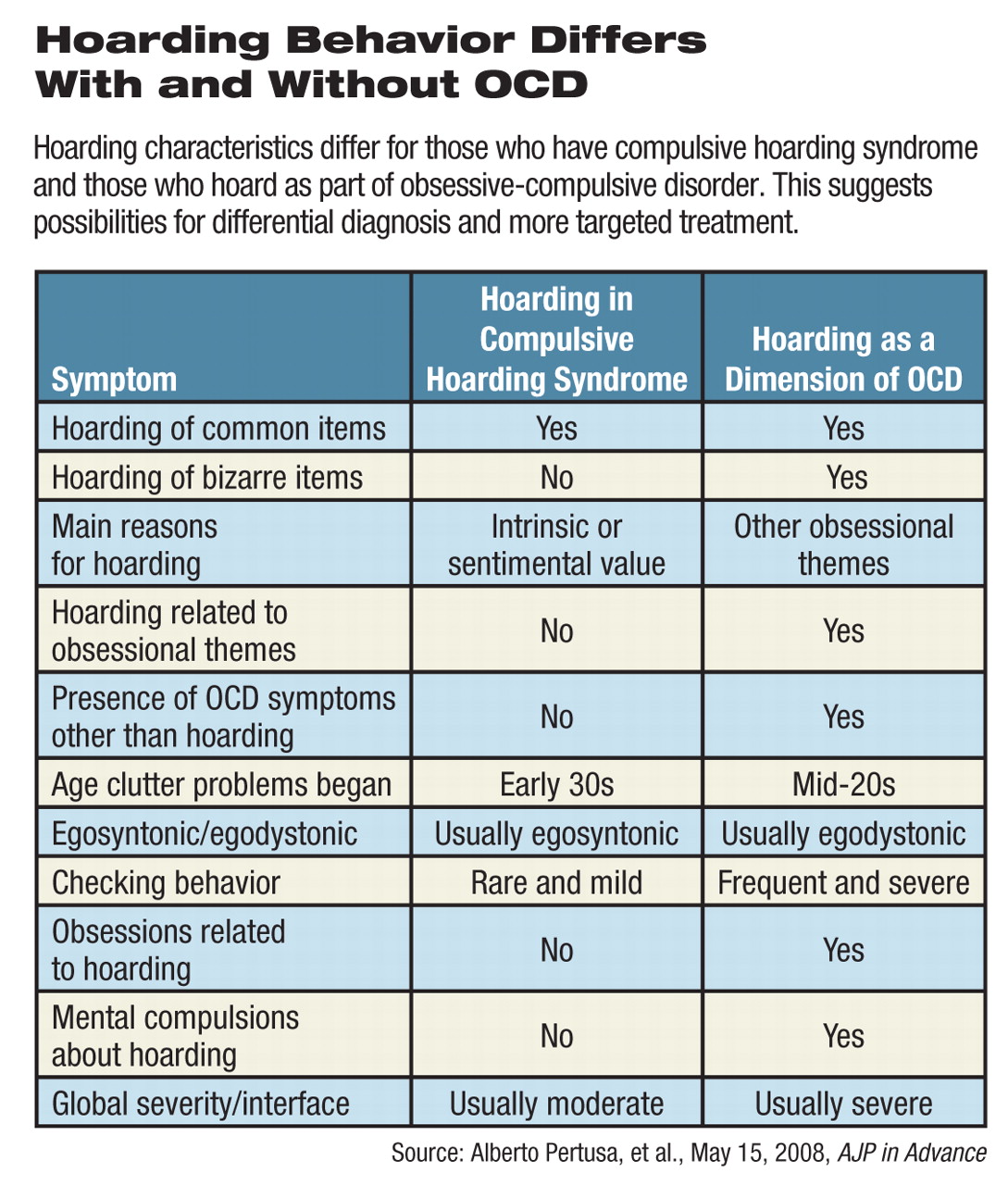
Now a group of researchers from Spain and the United Kingdom reports on a study of 163 individuals who exhibited hoarding behavior with and without OCD, OCD without hoarding, plus control subjects with anxiety but without either hoarding or OCD and healthy controls. An initial group of severe hoarders was divided into two groups, those with and those without OCD.
Patients who had “OCD plus hoarding,” “hoarding minus OCD,” or “OCD minus hoarding” were more likely to have relatives with OCD than were the anxiety and healthy control groups, wrote Alberto Pertusa, M.D., of the Division of Psychological Medicine at King's College London, Institute of Psychiatry, and colleagues (including Mataix-Cols) in the May 15 AJP in Advance. It is scheduled to appear in the print edition of the American Journal of Psychiatry in September.
Hoarding seemed to run in families, wrote Pertusa. “More than half of the participants in each of the two hoarding groups reported having at least one relative with significant hoarding behavior.”
Hoarders with OCD were more likely to collect “bizarre” items, like feces, urine, hair, or rotten food than were hoarders without OCD.
Between 70 percent and 74 percent of both groups reported that clutter filled most living spaces in their homes. The two groups said they started hoarding at about age 20, often after some traumatic event.
Hoarders without OCD said they collected items because they were valuable, might come in handy later, or had sentimental value. However, 28 percent of hoarders with OCD said they feared that something catastrophic would happen to them if they discarded an item.
Social phobia was more common in the two hoarding groups than in the“ OCD minus hoarding” group, and the two OCD groups had more generalized anxiety disorder than did hoarders without OCD.
“In most cases, compulsive hoarding appears to be a separate syndrome from OCD, which is associated with substantial levels of disability and social isolation,” concluded Pertusa. “[Our findings] support the idea of compulsive hoarding being a distinct clinical syndrome, which is highly comorbid with OCD as well as with other forms of psychopathology, like social phobia.”
As preparations get under way for DSM-V, due to be published by APA in 2012, researchers in the field hope to define the boundaries between OCD and hoarding to better diagnose patients with either or both sets of symptoms.
“Now is the time to revisit diagnoses that are uncertain,” said Samuels. “These studies all have implications not only for clarifying diagnosis but eventually for treatment as well.”
“Compulsive Hoarding: A Symptom of OCD, a Distinct Clinical Syndrome, or Both?” can be accessed at AJP in Advance at<http://ajp.psychiatryonline.org/pap.dtl>.“ To Discard or Not to Discard: The Neural Basis of Hoarding Symptoms in Obsessive-Compulsive Disorder” is posted at<www.nature.com/mp/journal/vaop/ncurrent/abs/4002129a.html>.▪