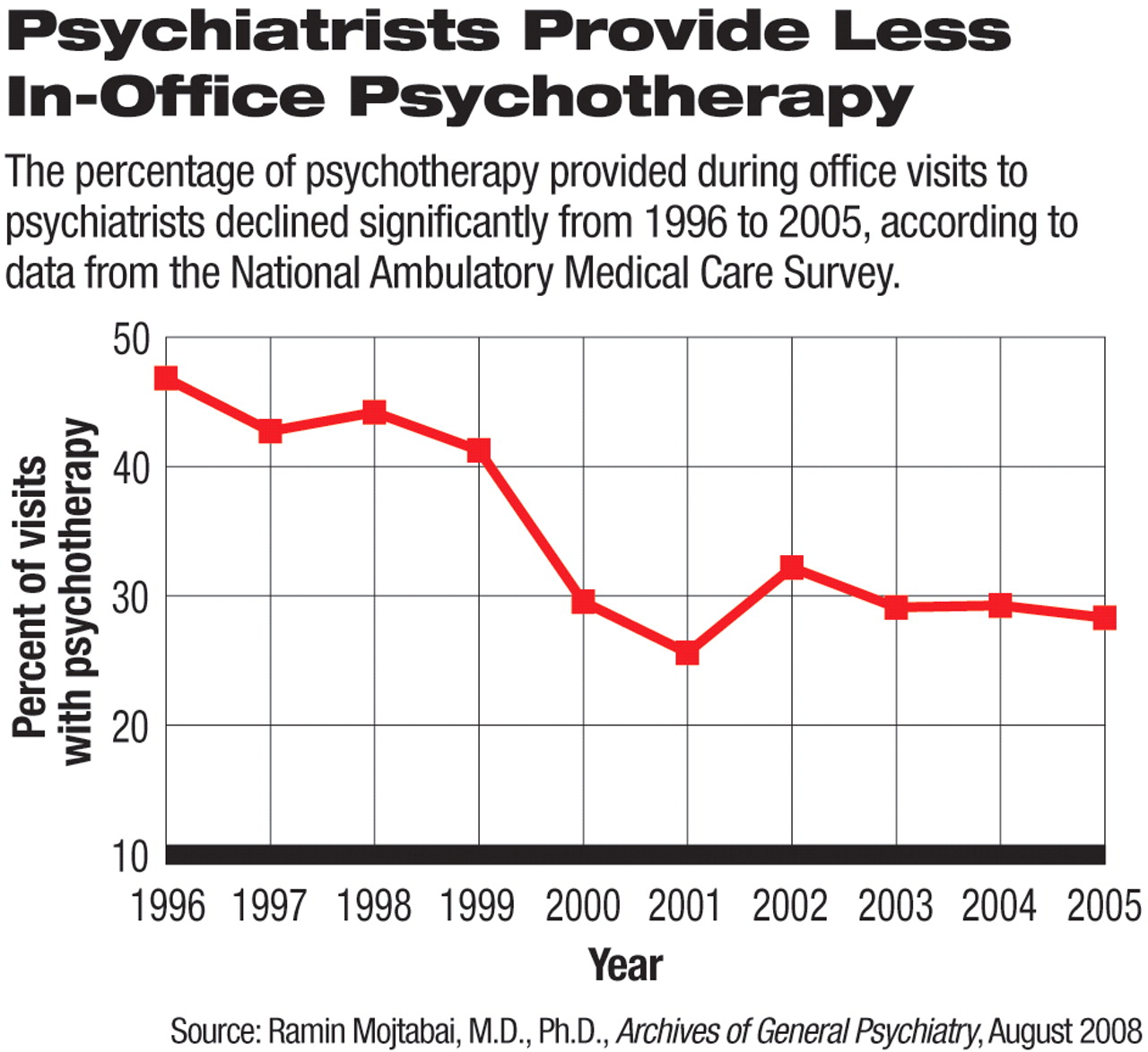
Outpatient psychiatric care in the United States saw a significant shift from psychotherapy to psychotropic medications from 1996 to 2005, according to a study published in the August Archives of General Psychiatry.
Based on the National Ambulatory Medical Care Survey (NAMCS), 28.9 percent of office-based visits to psychiatrists involved psychotherapy in 2004-2005, a significant decrease from 44.4 percent of office-based psychiatric visits in 1996-1997.
Only 10.8 percent of the psychiatrists in the sample provided psychotherapy to all of their patients in 2004-2005, about half the rate in 1996-1997 (19.1 percent).
On average, more than a quarter (28.4 percent) of the sampled psychiatric practices provided no psychotherapy during a typical week in 2004-2005.
A total of 5,597 visits to office-based psychiatrists in the overall NAMCS database were included in the analyses. The NAMCS is an annual survey of outpatient visits to physicians throughout the country. It collects information on these visits from a random sample of physicians or their staff during a randomly selected one-week period. The survey is conducted by the National Center for Health Statistics, a division of the Centers for Disease Control and Prevention.
The study was conducted by Ramin Mojtabai, M.D., Ph.D., an associate professor of mental health at Johns Hopkins University School of Public Health, and Mark Olfson, M.D., M.P.H., a professor of psychiatry at Columbia University College of Physicians and Surgeons and a researcher at the New York State Psychiatric Institute. The study was supported in part by a grant from the federal Agency for Healthcare Research and Quality.
Psychiatrists who saw more self-pay patients and conducted fewer visits covered by managed care provided more psychotherapy. In addition, the number of medications prescribed at a practice was inversely related to the amount of psychotherapy provided.
The reason for decreased use of psychotherapy, the authors believed, lies primarily in the financial incentives in favor of medication treatment over psychotherapy in recent years. They cited data from a previous study showing third-party reimbursement for one 45-minute outpatient psychotherapy session to be substantially less than three 15-minute medication-management visits. The increasing number of new psychotropic medications on the market also contributed to the trend, said the researchers.
“The trend [of decreasing psychotherapy by psychiatrists] is not at all a surprise, but the study is useful for giving us actual numbers,” Eric Plakun, M.D., director of admissions and professional relations at the Austen Riggs Center in Stockbridge, Mass., told Psychiatric News.
Plakun agreed with the study authors that financial disincentives for providing psychotherapy are among the main reasons for its declining use, but suggested that the shift in the training of psychiatrists is also a significant factor. “The field of psychiatry has moved toward more pharmacological treatment and other approaches like [electroconvulsive therapy]. It reflects changes in who the teachers are and who is selected into psychiatric residencies,” he explained. Preceptors and mentors specializing in psychotherapy are rare in many programs.
As chair of APA's Committee on Psychotherapy by Psychiatrists, Plakun noted that the committee has been addressing the decline in psychotherapy use and training for more than a decade and helped establish the Accreditation Council for Graduate Medical Education's requirements for psychotherapy training in psychiatry residency programs.
If psychiatry is walking away from psychotherapy, this direction has“ implications for the identity of psychiatry as a profession,” the authors wrote. Although some strongly believe psychotherapy is an important and integral part of a psychiatrist's arsenal, they noted, “a growing group of psychiatrists ... appear to shun delivery of formal psychotherapy all together.”
The study does not show whether patients were getting less psychotherapy overall or simply getting it from other mental health clinicians. However, Plakun noted that psychiatrists are in the best position to integrate both psychotherapy and medication management, especially for patients who are more severely ill. He pointed out that a substantial proportion of patients have disappointing or no response to multiple courses of medications, and many have comorbid conditions that require a full arsenal of treatments from psychiatrists who are skilled in delivering all of them.
Large clinical trials on mental illnesses such as depression and bipolar disorder have demonstrated the superior efficacy of combining psychotherapy and medications over either treatment alone (Psychiatric News, November 2 and May 4, 2007). The higher cost of providing both treatments, however, often makes the combination treatment difficult for patients to access.
“We need to ask ourselves what the future role of psychiatrists is,” said Plakun. He believes that psychiatrists will become the ultimate specialists to diagnose and treat the more severely ill and difficult-to-treat patients. To treat these patients effectively,“ psychiatrists need the competency to integrate medications and psychotherapy,” he said.
An abstract of “National Trends in Psychotherapy by Office-Based Psychiatrists” is posted at<archpsyc.ama-assn.org/cgi/content/abstract/65/8/962>.▪