All depression is not created equal—severity levels and treatment effects differ from person to person. But a new analysis of aggregate data shows that depression rates also vary widely in this country by state.
The differences, according to researchers and mental health advocates, are directly linked to the availability of mental health resources and state mental health policies.
“Depression is one of the most disabling conditions affecting people in this country,” said David Shern, Ph.D., president and CEO of Mental Health America, the organization that issued the report of the state rankings. Shern made his remarks at a press conference last November in Washington, D.C.“ The good news is that we can do something about it—we must continue with the progress we've made in providing equitable, appropriate access to depression care.”
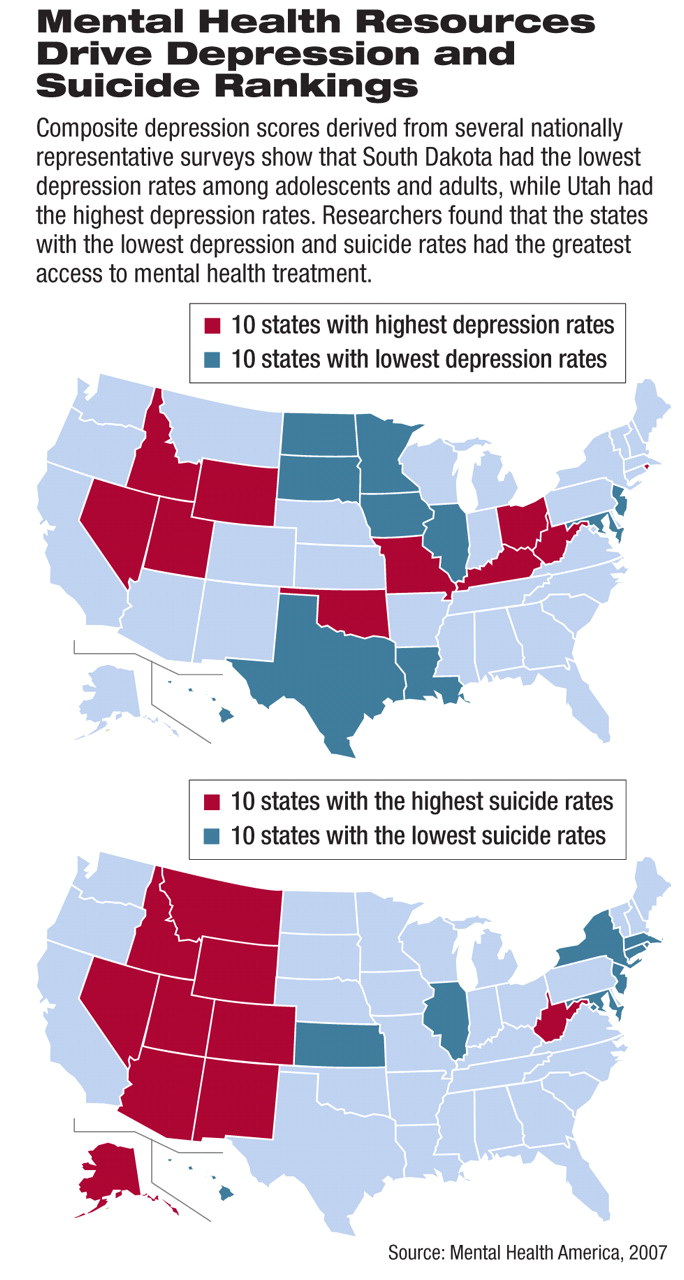
Using data from a number of nationally representative surveys between 2000 and 2006, including the Center for Disease Control and Prevention's Behavioral Risk Factor Surveillance System and the federal National Survey on Drug Use and Health Survey, researchers found that South Dakota was rated the healthiest state in terms of depression, with Utah ranking last.
They gathered data on depression using the following measures: the percentage of adults and adolescents experiencing at least one major depressive episode a year, the percentage of adults experiencing serious psychological distress (defined on the K6 scale by six questions about how frequently they experienced psychological distress during the one-month period in the past year when they were at their worst emotionally), and the average number of days in the past month in which those surveyed reported that their mental health was not good.
South Dakota showed the best results for the measures used to develop a composite depression status indicator, according to the report.
On average, residents of South Dakota experienced 2.41 poor mental health days a month. Among adults, 7.31 percent experienced a major depressive episode in the prior year, and 11.16 percent experienced serious psychological distress. Slightly more than 7 percent of adolescents experienced a major depressive episode in the prior year.
In contrast, Utah residents had the highest reported depression rates, with West Virginia and Kentucky following closely in terms of depression status.
Among adults and adolescents in Utah, 10.14 percent experienced a depressive episode in the past year, and 14.58 percent experienced serious psychological distress.
Each state also was ranked by suicide rate, using 2004 data from the National Vital Statistics System. According to the report, the District of Columbia had the lowest suicide rate, with 5.32 suicide deaths per 100,000 people. Alaska had the highest suicide rate, with 23.05 suicide deaths per 100,000 people.
To better understand differences between states in terms of depression and suicide rates, researchers also studied the association between prevalence rates and the following in each state: mental health policies, mental health treatment resources, the prevalence of barriers to mental health care, use of psychiatric treatment, and socioeconomic characteristics of residents.
Not surprisingly, researchers found that state characteristics such as availability of mental health treatment providers and the presence of mental health parity laws were linked to a state's depression and suicide rates and its subsequent ranking.
For instance, the higher the percentage of a state's population who reported unmet mental health care needs, the worse the state's depression status (p<.001). Utilization, measured as antidepressant prescriptions per capita in the state and the percentage of the adult population who received treatment in the past year, was also positively correlated with depression rates. The percentage of residents receiving mental health treatment was positively correlated with mental health status (p<.001). In addition, the more educated the state population, the higher the depression rates.
With regard to suicide, researchers found that the more mental health professionals there were in a state, the lower the suicide rate was (p<.001). Higher levels of mental health care utilization and higher educational levels were also associated with lower suicide rates.
Moreover, “Those with greater access to mental health coverage in insurance had lower suicide rates,” Shern pointed out.
Mental health advocate and consumer Cynthia Evans, who attended the press conference, added a personal dimension to the statistics. Evans, raised by a mother with schizophrenia and a father involved with drugs, was first hospitalized for depression at around the age of 13.
This was the first of many subsequent hospitalizations and suicide attempts, she told attendees at the press conference.
As an adult, Evans had difficulty getting mental health treatment due to inadequate insurance coverage. “I was almost going without groceries to try and maintain my mental health,” she noted. Evans, who is in recovery, commented that “this isn't rocket science. The more people who have access to affordable mental health care, the fewer who kill themselves.”
Shern suggested that enacting parity legislation on a broader basis, thus expanding access to affordable mental health treatment, will vastly improve depression and suicide rates in the United States.
Despite the fact that some states did better than others in terms of depression and suicide, he noted, “no state can be satisfied with its current status... .These rates can be driven lower by encouraging state policies designed to improve coverage, end discriminatory practices in insurance, and assure that qualified mental health professionals are available to serve everyone in need.”
The study was conducted on behalf of Mental Health America by researchers from Thomson Healthcare (a company that provides clients “integrated information-based solutions”), along with an unrestricted educational grant from Wyeth Pharmaceuticals.
“Ranking America's Mental Health: An Analysis of Depression Across the States” is posted online at<www.mentalhealthamerica.net/go/state-ranking>.▪