There is no hypothesis shortage out on the frontier where infectious disease meets schizophrenia.
Two more studies now pave a little more of the road to that borderland, but they also show how much farther the science needs to travel.
Over the last few decades intriguing, if inconclusive, studies suggested that maternal infection with influenza, genital or reproductive pathogens, or toxoplasmosis during pregnancy may be linked to higher rates of schizophrenia among off-spring. Studies of Swedish health registry data and U.S. military personnel now provide further hints that risk may extend to infections acquired in childhood.
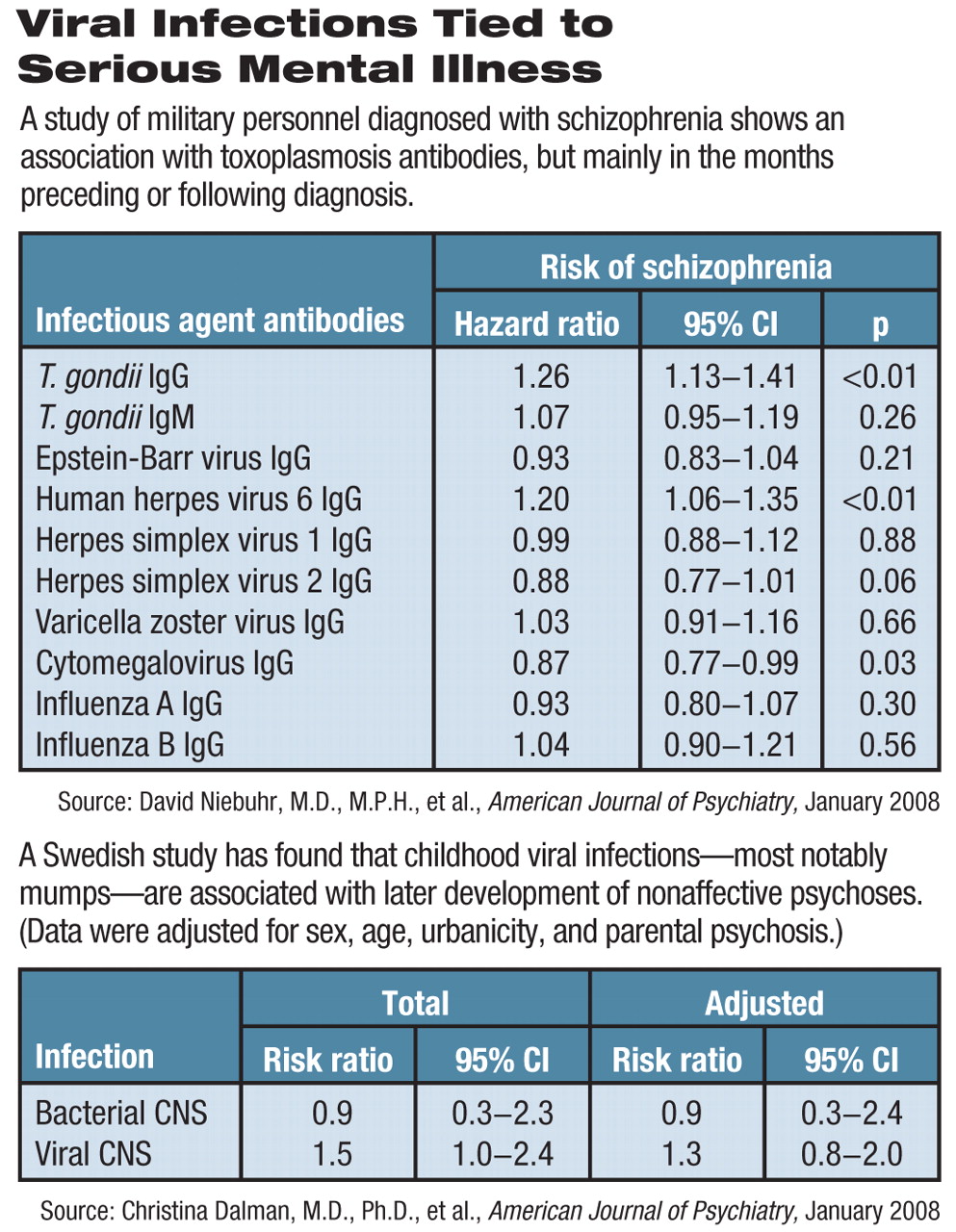
The Swedish study examined health records of children born from 1973 to 1985 to identify patients who were hospitalized for central nervous system (CNS) infections between birth and age 12 and were also admitted for nonaffective psychotic illnesses after their 14th birthday. They found 8,985 out of 1.2 million children were exposed to CNS infection, including 2,435 bacterial and 6,550 viral infections; 2,269 subjects had been hospitalized for nonaffective psychosis; and 23 subjects recorded both CNS infections and psychosis.
“We found a weak association between viral CNS infections in childhood and later development of nonaffective psychotic disorders,” wrote Christina Dalman, M.D., Ph.D., of the Department of Psychiatric Epidemiology at Stockholm's EPI/Karolinska Institutet, and nine colleagues in the January American Journal of Psychiatry (AJP).
Bacterial infections occurred in only four subjects with psychosis and accounted for no increased risk. However, the 19 subjects with viral CNS infections had a greater risk for developing psychosis (risk ratio [RR] = 1.5, confidence interval = 1.0-2.4). Adjustment for sex, age, urbanicity, or parental psychosis reduced the risk slightly but brought the results below the level of statistical significance (see chart).
Enterovirus infection (RR=1.0) was not associated with later development of psychosis, but mumps (RR=2.7) and cyto-megalovirus (RR=16.6) were. The authors cited prior research indicating that mumps virus can invade the brain, infecting ependymal cells, persisting in neurons, and perturbing development of or causing problems with memory, learning, or sensory and motor abilities. A mumps vaccine was introduced in Sweden in 1982, before which mumps was the most common cause of aseptic meningitis or mild encephalitis, according to Dalman.
The number of cases may be small, but the fact that the study focuses on CNS infection that caused delirium, headache, or meningitis worthy of hospitalization is a key point, said Alan Brown, M.D., an associate professor of clinical epidemiology at the Mailman School of Public Health and an associate professor of clinical psychiatry at New York State Psychiatric Institute at Columbia University. Brown has studied the connection between prenatal infections and schizophrenia, and wrote an editorial accompanying the two articles.
“If anything, the study might have missed milder cases, since some viral infections would not warrant hospitalization,” he told Psychiatric News. “Plus, some patients may have had such serious neurological effects from their infections that psychiatric disorders might be masked.”
The CNS infections were spread across the entire 12-year age span studied, which might make it hard to tie infection to specific neurodevelopmental timing or mechanisms, said Brown. Perhaps infection causes some brain inflammatory process, especially among glial cells, leading to fibrosis in brain tissue, he speculated.
The second report, also in the January AJP, is a pilot study that compared antibodies for nine common infectious agents from 180 members of the U.S. Army, Navy, and Air Force discharged from military service between 1992 and 2001 after a diagnosis of schizophrenia. The armed forces routinely take serum samples when a person enlists and about every two years afterward. The 180 patients were matched with 532 healthy military service members with no mental disorder.
Researchers led by Col. David Niebuhr, M.C., a physician and chief of the Department of Epidemiology at Walter Reed Army Institute of Research, measured immunoglobulin G (IgG) levels of antibodies to Toxoplasma gondii and to several common viruses. T. gondii IgG was associated with a significantly higher hazard ratio (HR=1.24, p<0.01) for schizophrenia. Human herpes virus 6 also had a significant positive association (HR=1.20).
However, while 58 percent of serum samples were taken at least six months before diagnosis, the only significant associations between T. gondii IgG and schizophrenia occur within six months prior to diagnosis or after that point.
“That means the cause-and-effect mechanism could work either way,” said Brown. “T. gondii might cause schizophrenia, but a lifestyle associated with schizophrenia might just as well increase the risk of contracting toxoplasmosis.”
Niebuhr's team found little evidence of seroconversion, indicating that infection generally occurred before the first specimen had been drawn, he told Psychiatric News. Given that, he said, “... from our data, we cannot address the issue of prodromal behaviors resulting in T. gondii infection.”
The report had a few other issues that Brown hoped will be addressed when Niebuhr and colleagues expand their research to cover all 1,200 subjects they have identified so far. Serial data on antibody levels are not reported by individual subjects, so it's hard to tell when they became seropositive, said Brown.
“Most of the serum specimens were negative for both cases and controls, but we found that cases were more likely to have higher antibody levels than controls,” explained Niebuhr. “Therefore, the sera for all groups contain both positive and negative specimens, and both positive and negative specimens were included in the analyses.”
The expanded study will include more cases and more specimens per case, which might help tease out the temporal relationship of infection and onset of schizophrenia, said Niebuhr. But if new infection occurs not long before or after schizophrenia, a clear answer may not be possible without further investigation, he said.
Although independent replications are warranted, both studies are“ promising,” said Brown, and support an infectious etiology for schizophrenia once thought implausible.
The size of the effects observed was small, compared with the 20 percent of the U.S. population exposed to T. gondii, for example, he said. If elevated antibodies were shown prospectively to be a risk factor for schizophrenia, studies like these would imply the potential for prevention.
“Given that some infections linked to risk of schizophrenia may be treatable or prevented by vaccines, we may already be preventing cases of schizophrenia by administering mumps vaccine during childhood,” he said.“ An excellent test of the toxoplasma hypothesis would be to see if giving antitoxoplasmosis antibiotics to people seropositive for T. gondii decreased antibodies and improved symptoms of schizophrenia.”
Whatever the outcome, such a trial might be another step toward ruling in or out a postnatal role for the infection in the origins of schizophrenia.