Deep stimulation of the subthalamic nucleus region of the brain is a well-established surgical procedure for treating advanced Parkinson's disease. It can dramatically improve patients' motor symptoms and quality of life. However, according to a new study in the October Brain, clinicians are advised to monitor such patients carefully for suicide risk following the procedure.
The international case-control study, nested within a retrospective survey of movement disorder, included more than 5,000 subjects. All had undergone deep stimulation of the subthalamic nucleus area to alleviate Parkinson's disease symptoms. The subjects had been treated at 55 centers in North America, South America, Europe, and Asia.
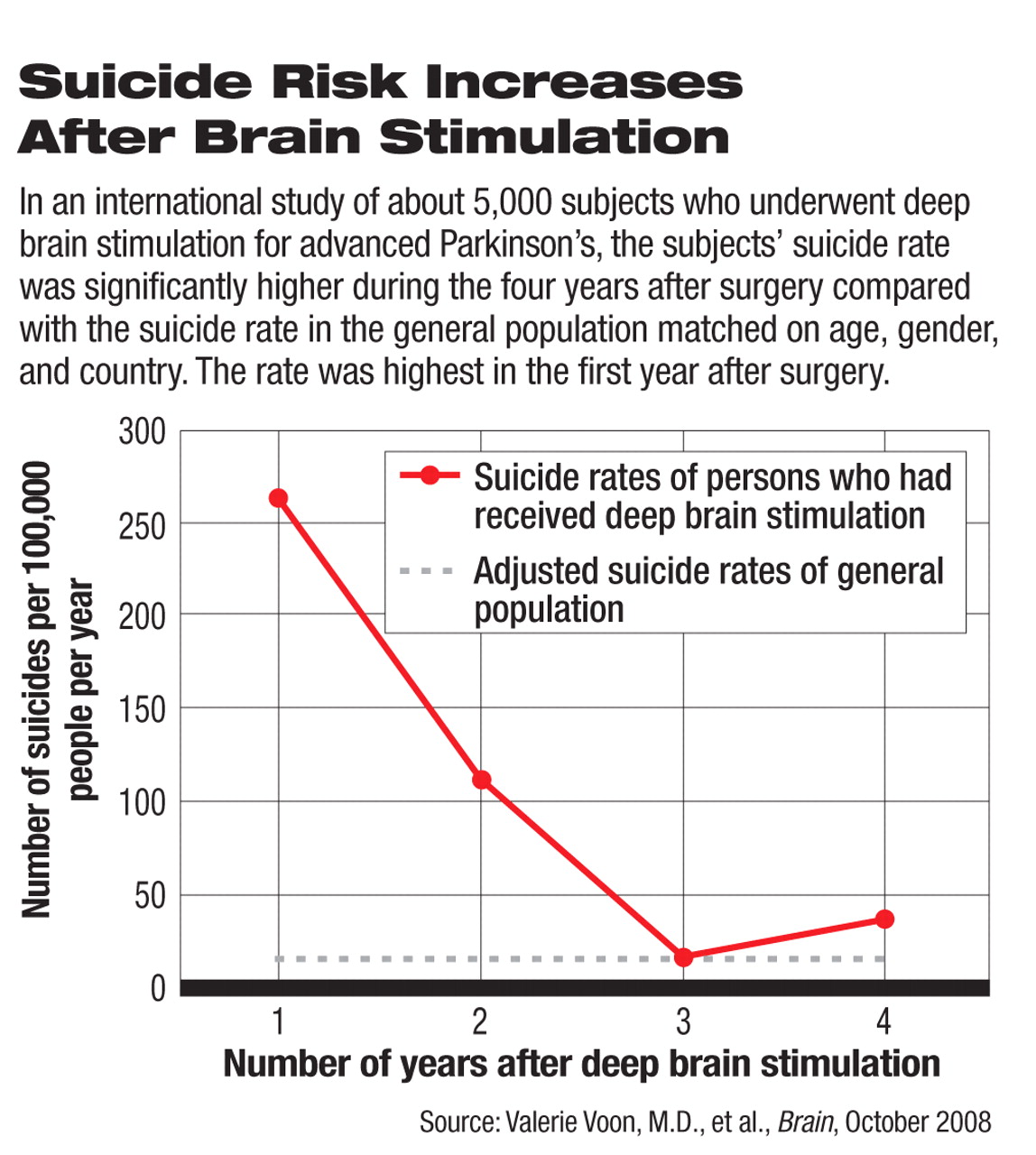
Their suicide rates after the procedure were compared with the age- and gender-adjusted suicide rates of the general population in their respective countries. (The authors cited literature showing that Parkison's disease suicide rates ranged from the same as to as much as 10 times lower than the those of the general population.)
The suicide rate of the subjects who had received deep brain stimulation for Parkinson's disease was statistically, significantly much higher during the first year after the procedure compared with the country-specific adjusted general population suicide rates. The suicide rates of the Parkinson's patients during the second, third, and fourth years after the procedure were lower than during the first year, but still significantly elevated.
These results did not surprise the study's lead investigator, Valerie Voon, M.D., a staff psychiatrist at Toronto Western Hospital in Canada when the study was conducted. She told Psychiatric News that “there were early reports of very high, postoperative suicide rates based on single centers. This study [simply] helps establish that the rate is high.”
Voon and her colleagues also tried to identify the reason or reasons for the increased risk of suicide in Parkinson's subjects who had received deep brain stimulation by comparing Parkinson's subjects who had received the procedure and had committed or attempted suicide to Parkinson's patients who had received the procedure but had not committed or attempted suicide. They found that being younger, having an earlier age at the onset of the disease, being single, having a history of impulse control disorders, and having made a previous suicide attempt seemed to be some of the reasons. However, the major reason appeared to be postoperative depression. But why?
“There is no evidence that subthalamic nucleus deep brain stimulation is associated with depression,” said Voon, who is now affiliated with the U.S. National Institute of Neurological Diseases and Stroke. “On the contrary, the majority of studies note an overall improvement in mood symptoms [after the stimulation].” Thus, it is unlikely that the postoperative depression is due to the stimulation, she said.
However, two other possibilities may explain the postoperative depression, she noted: the depression was caused by Parkinson's disease or it existed prior to the procedure. Further analysis revealed that the postoperative depressed subjects had a significantly greater frequency of preoperative antidepressant use and a trend toward more frequent preoperative suicide attempts than the postoperative nondepressed subjects. This finding supports the possibility that the depression existed prior to surgery.
In any event, the findings suggest that psychiatrists involved in the selection of patients for deep brain stimulation for Parkinson's disease, or for other conditions, should carefully screen them for suicide risk, said Voon. Such an assessment “is not necessarily a contraindication to surgery,” she explained. Furthermore, after patients receive deep brain stimulation, psychiatrists should evaluate them for depression, and if they are found to be depressed, the depression should be managed and followed.
The good news, she said, is that by treating postoperative depression,“ the risk for postoperative suicide is clearly modifiable.”