At least part of the reason why patients with alcohol dependence respond differently to naltrexone treatment appears to lie in a particular variation in the opioid receptor gene known as OPRM1, according to a study in the February 4 Archives of General Psychiatry.
Researchers at the Medical University of South Carolina found a significant link between a genetic polymorphism and the likelihood of good clinical response to naltrexone treatment based on genetic and outcome data collected in the multicenter, Combined Pharmacotherapies and Behavioral interventions for alcohol Dependence (COMBINE) study.
The COMBINE study was funded by the National Institute on Alcohol Abuse and Alcoholism and conducted from 2001 through 2004. Patients with diagnosed alcoholism were treated with 100 mg of naltrexone or placebo for 16 weeks. The authors analyzed the genetic data prospectively collected from 1,013 participants.
According to previous research, most people carry the Asn40 polymorphism type of the OPRM1 gene on both of their chromosomes, which means that the amino acid asparagine resides at position 40 in the receptor protein. Because of a single nucleotide mutation, however, this amino acid may be substituted with aspartate (Asp40). Previous research estimated that 15 percent to 25 percent of the human population carry at least one copy of the Asp40 allele, and this slight change in the μ-opioid receptor protein may affect the carrier's response to alcohol and pharmacologic treatment for alcoholism.
Naltrexone is an antagonist for several opioid receptors and binds preferentially to the μ-opioid receptors. It is approved for the treatment of alcoholism and has been shown to reduce alcohol-induced highs and alcohol cravings. The drug's effect size over placebo is “in the small to moderate range,” the authors noted.
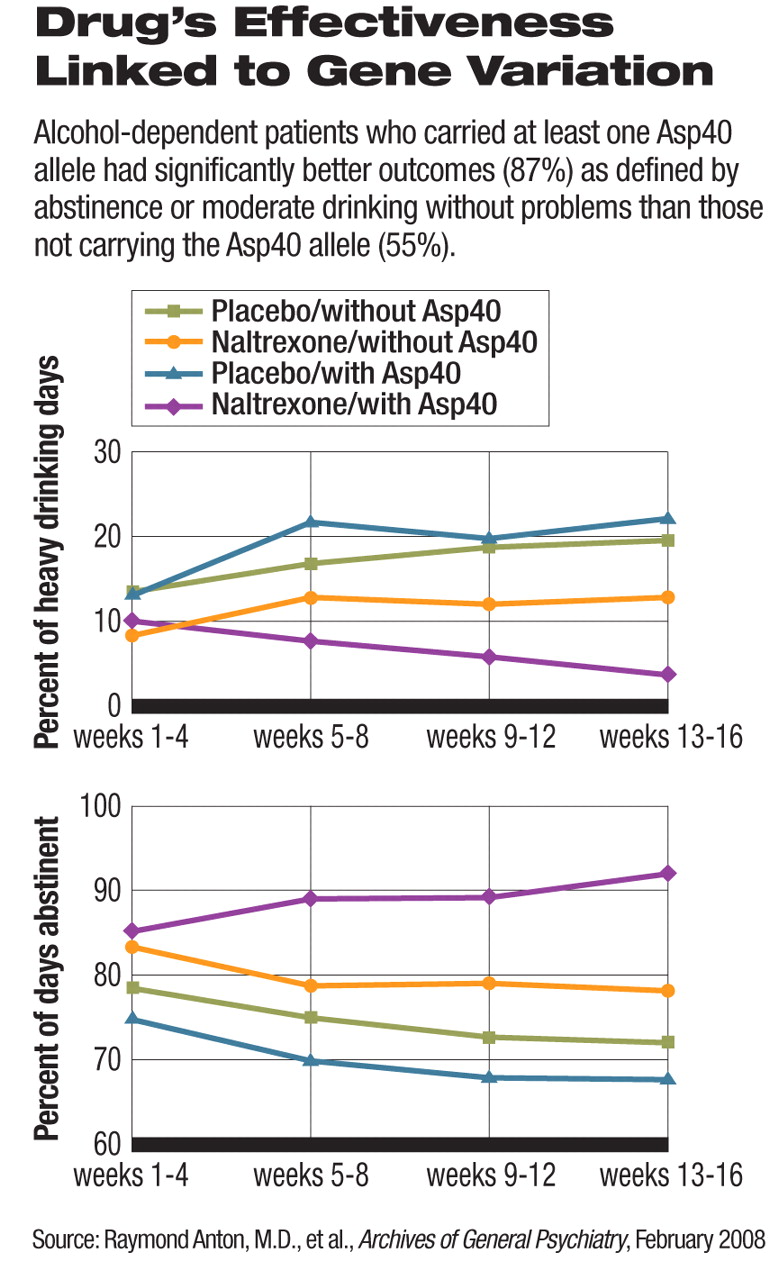
In the COMBINE study, naltrexone increased the percentage of days abstinent and decreased the percentage of heavy-drinking days, compared with placebo, among patients who carried at least one copy of the Asp40 allele. In those who carried two copies of it, however, naltrexone was not significantly different from placebo in these drinking-related outcomes. These differences were statistically significant in participants who underwent brief medical-management sessions, but not in those who received the more intense and specific combined behavioral intervention (CBI). The behavioral interventions may have obscured the interaction between genetics and naltexone, the authors suggested.
Among the participants who carried at least one Asp40 allele, 87 percent of those who took naltrexone had a good clinical outcome, defined as abstinence or moderate drinking without problems, during the last eight weeks of the treatment. In contrast, about 55 percent of those with two Asn40 alleles had similar response to naltrexone. The difference was statistically significant. The two genotypes responded to treatment without naltrexone in similar rates around 50 percent.
The effect of genetic variations on the efficacy of naltrexone revealed in this study “could have immense clinical importance,” lead author Raymond Anton, M.D., and colleagues said. For example, the development of anyμ -opioid antagonist should also consider potential interaction with the OPRM1 genetic variance. “We can't say for sure that all μ-opioid antagonists will have this type of interaction, and perhaps they have slightly different binding sites, kinetics, etc., but there is a high probability that they will,” Anton, a professor of psychiatry and director of the Center for Drug and Alcohol Programs at the Medical University of South Carolina, commented to Psychiatric News.
He cautioned that prospectively randomized studies based on genetic variations are needed to confirm the interaction between this genetic variation and naltrexone. In addition, “this finding is largely limited to Caucasians; we could not explore African Americans, Hispanics, or Asians independently [in the COMBINE study],” he said. At this point, he recommended that clinicians and patients “weigh the evidence and decide for themselves whether a genetic test should be performed prior to the decision to use or not use naltrexone for alcohol treatment.”
Genetic research has been quietly making its way into pharmacotherapy of various diseases. Scientists have found specific gene variations that predict who is more likely to experience certain effects from drugs, such as emerging suicidal thoughts from selective serotonin reuptake inhibitors, excessive bleeding with normal warfarin dosage, and severe skin reactions to carbamazepine (Psychiatric News, January 18). The link between the OPRM1 gene and naltrexone efficacy is another example of how genetic variations explain why a drug helps some patients but not others.