Changes in the CPT nursing home evaluation and management (E/M) codes may make using these codes a better choice than billing under the standard psychiatry codes for care provided to patients in nursing homes.
Despite the fact that the conversion factor used to determine Medicare rates was increased by .5 percent for the first six months of 2008, many of the psychiatry CPT codes sustained a drop in payment because of a downward adjustment made to the work value of all CPT codes. This adjustment was necessary to maintain Medicare's budget neutrality (for a complete explanation of the 2008 Medicare fees, see<www.psych.org/Departments/HSF/MedicareMedicaid/2008MedicareFeeSchedule.aspx>). While the psychiatry codes fell in value, however, some of the nursing home E/M code values (RVUs) increased.
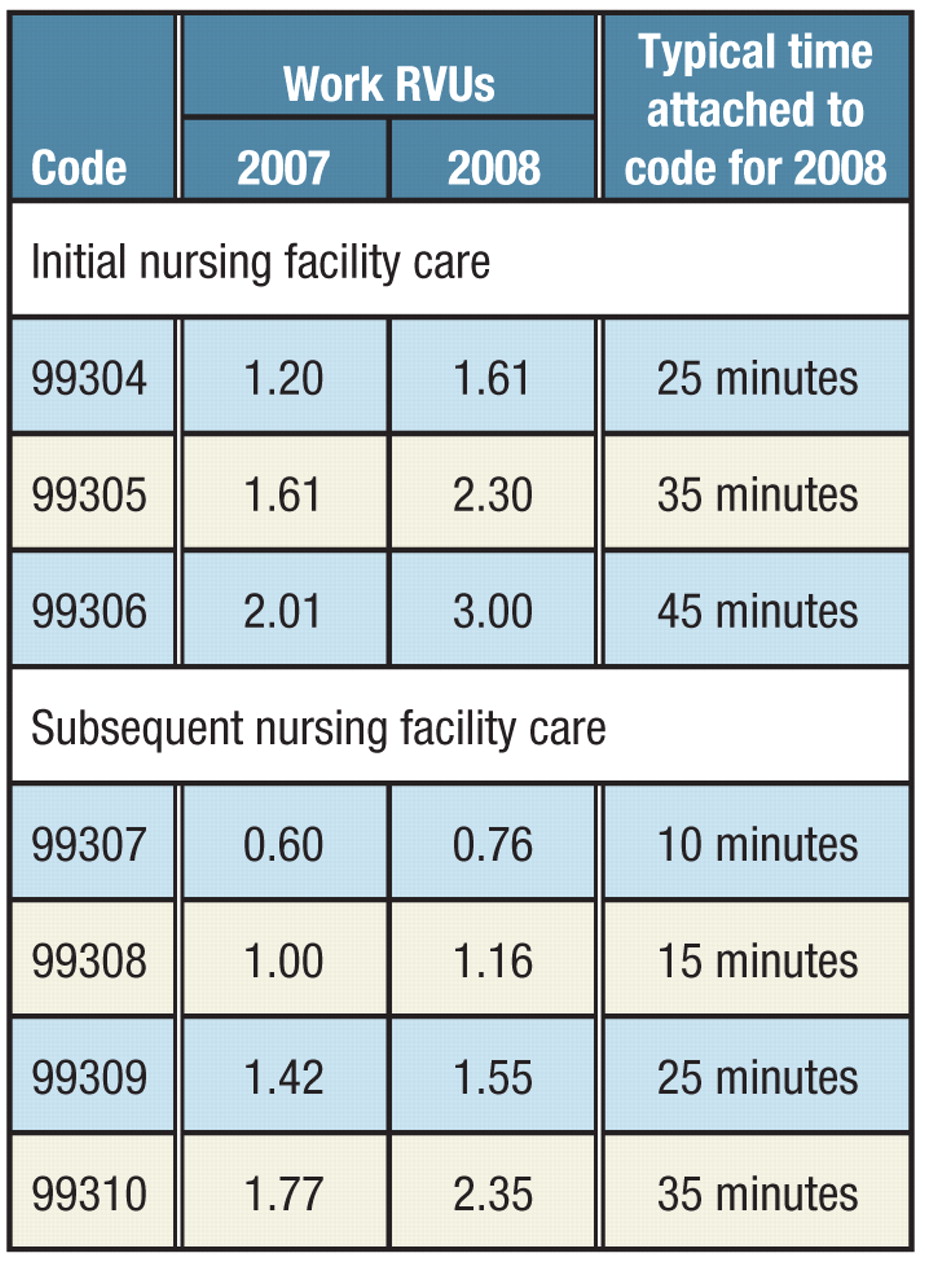
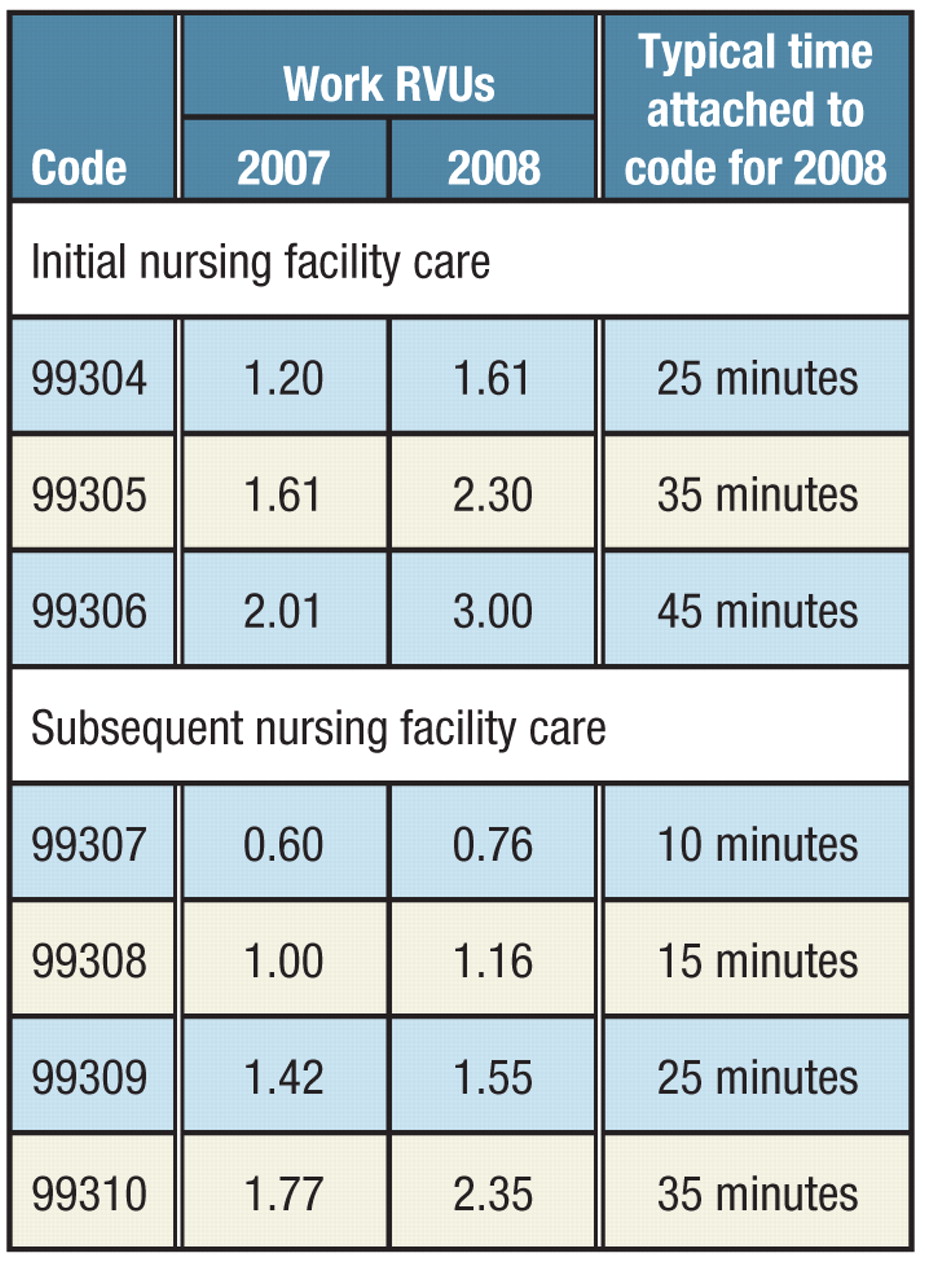
The new values attached to these codes make them more comparable to 90801 (initial psychiatric evaluation) and 90862 (pharmacologic management), codes that many psychiatrists use for their nursing home practices. (The corresponding 2008 work RVUs for 90801 and 90862 are 2.80 and 0.95.) Typical times for the nursing facility E/M codes were established and published in the 2008 CPT manual, which increases the potential utility of these codes. Because of the addition of the typical time in the code descriptor, when time spent in coordination of care and/or counseling services accounts for more than 50 percent of the total time, psychiatrists can use the appropriately timed code on the basis of time alone without having to be concerned with the standard documentation demands for E/M codes.
These changes are important for psychiatrists to understand when determining which codes are most appropriate for services provided to nursing home residents.
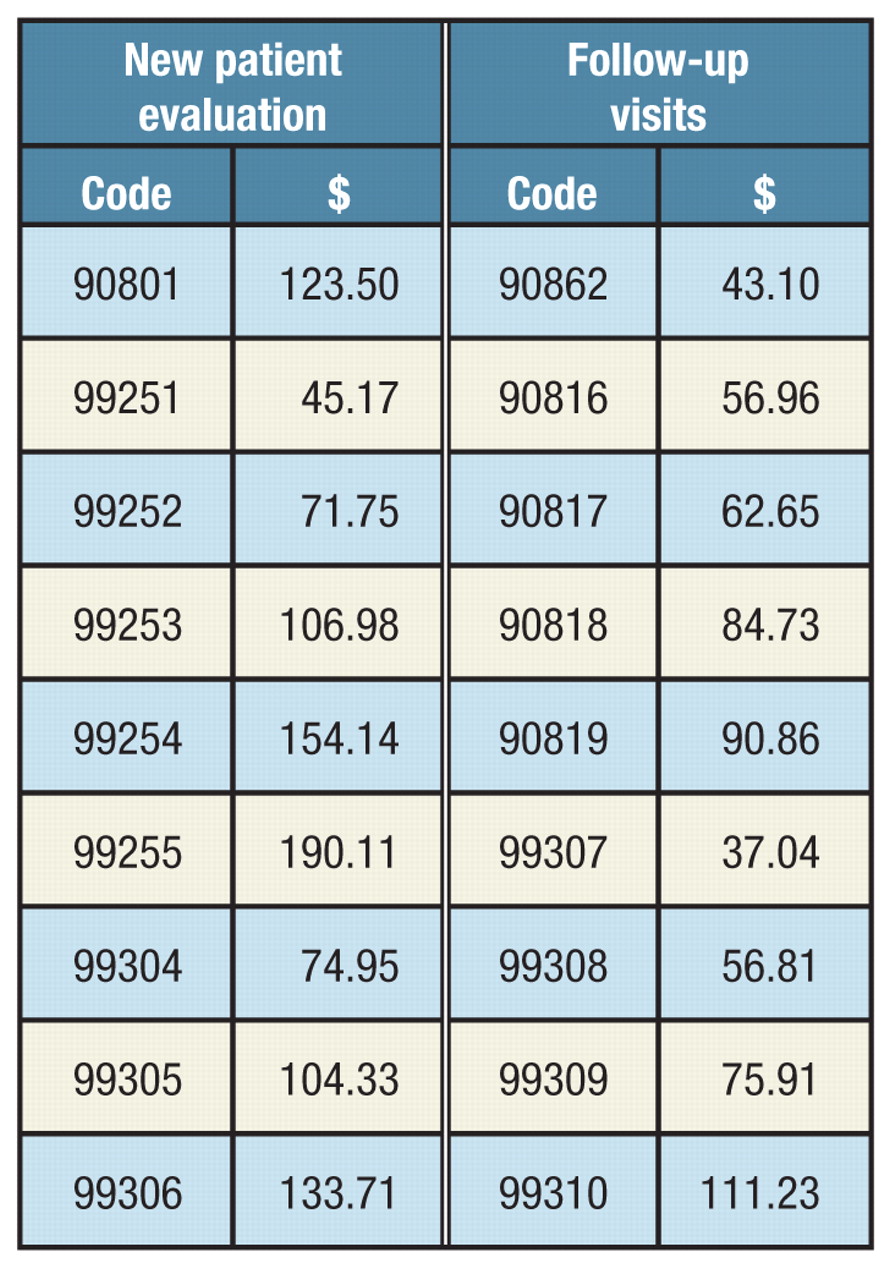
The table on the left compares the dollar amounts paid for various codes. (These dollar amounts represent payments for treatment provided in a facility by participating physicians and are taken from the Ohio Medicare carrier. Actual fees vary from state to state and locale to locale, although the ratios generally stay the same.)
The codes 90816-90819 are time-delineated inpatient and nursing home psychotherapy codes without (even numbered) or with (odd numbered) evaluation and management services (90816 and 90817, 20 to 30 minutes; 90818 and 90819, 45 to 50 minutes).
The even-numbered codes can be used by other mental health practitioners—psychologists, for example. The odd-numbered codes can be used only by a psychiatrist or other clinician licensed to prescribe medication.
Please note that psychotherapy should not be confused with counseling and coordination of care. As defined by the CPT manual, psychotherapy is the treatment for mental illness and behavioral disturbances in which the clinician establishes a professional contract with the patient and, through definitive therapeutic communication, attempts to alleviate the emotional disturbances, reverse or change maladaptive patterns of behavior, and encourages personality growth and development. Counseling is defined as a discussion with the patient and/or family or other caregiver concerning one or more of the following: diagnostic results, prognosis, risks and benefits of treatment, instructions for management, compliance issues, risk-factor reduction, and patient and family education.
The key point in devising a billing plan for nursing home work is to document according to CPT guidelines and base CPT code choice on the code that is the most appropriate for the service you provide, whether it is psychotherapy or evaluation and management. ▪