Three-quarters of U.S. employers do not plan to drop insurance coverage for mental health and substance use treatment when a new federal law goes into effect next year requiring them to offer such benefits at a level equal to that of other medical benefts, a recent survey indicates.
The online survey, to which more than 140 employers responded, was conducted by the Partnership for Workplace Mental Health, a program of the American Psychiatric Foundation. The survey was designed to elicit a better understanding of the extent of currently available mental health benefits and what changes employers will make to comply with the new parity law.
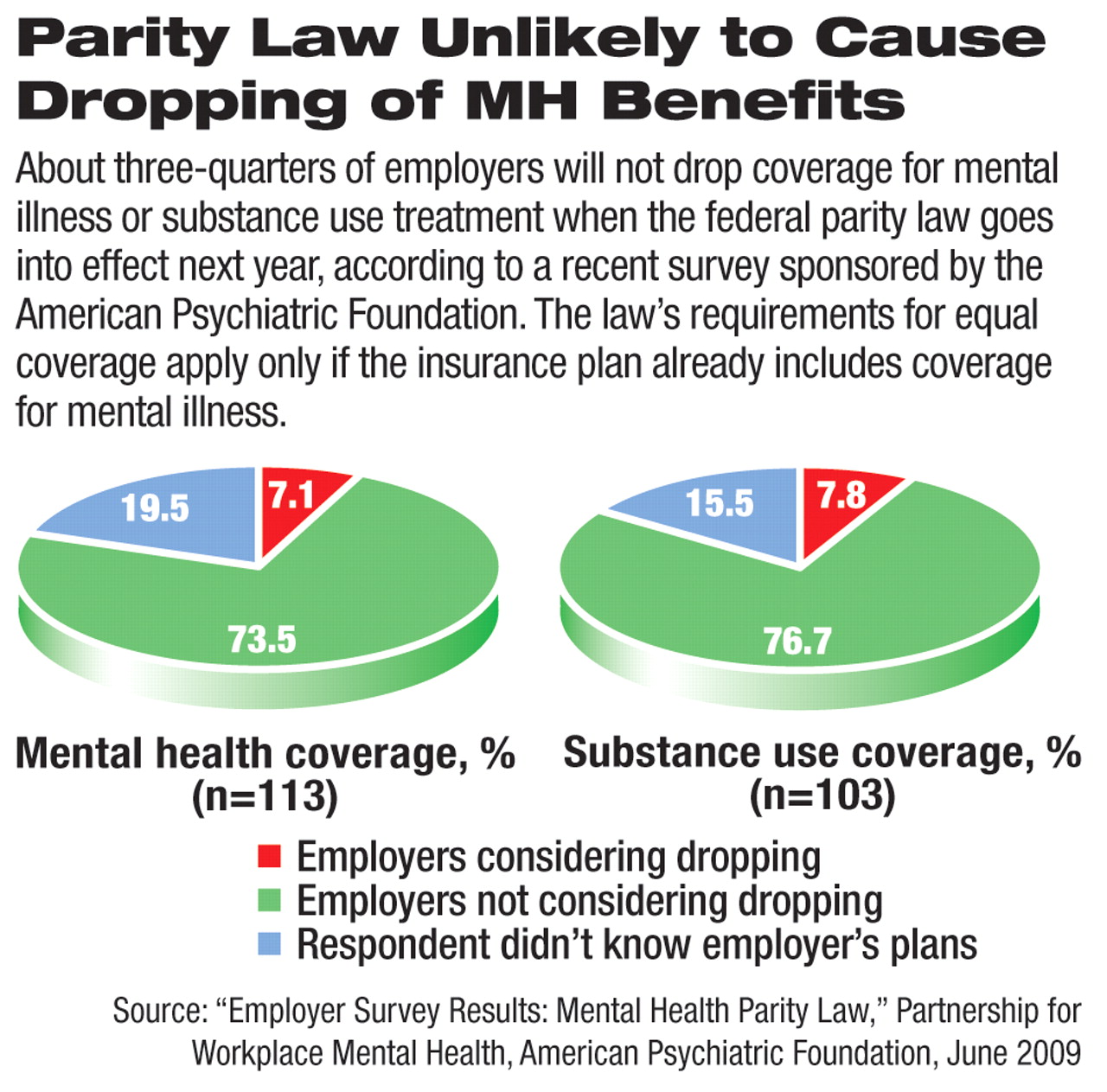
Among the chief results of the survey was a finding that 93 percent of respondents offer at least some mental health benefits, and among those, at least 74 percent were not considering dropping mental health coverage. In addition, at least 77 percent were not considering dropping substance use treatment coverage as a result of the law. The next-largest groups of respondents did not know whether dropping either coverage was under consideration. Only about 7 percent of respondents reported they were considering dropping mental health coverage, and about 8 percent were mulling the end of substance use treatment coverage.
“The [survey] results tell us that employers understand that mental health is an essential component of health,” said Alan Axelson, M.D., cochair of the partnership's Advisory Council and medical director of InterCare Psychiatric Services in Pittsburgh.
The new parity law, known as the Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act, requires health plans that offer mental health coverage to have the same benefits, copayments, and treatment limits as other types of health care. The law, which potentially could give 113 million people equal access to mental health coverage if employers retain insurance plans with behavioral health features, goes into effect on January 1, 2010, for most calendar-year plans. The law exempts employers with 50 or fewer employees from its requirements. Final regulations to implement the law are expected to be issued in October.
The survey authors sent out about 1,000 questionnaires to employers of varying sizes and received 143 completed responses.
More than three-quarters of responding companies are covered by the Employee Retirement Income Security Act (ERISA). Companies that self-insure and fall under ERISA were not subject to previous state mental health insurance parity requirements.
The survey found many employers will have to make significant changes in the health plans they offer workers to comply with the law. The law, for instance, requires employers to make several benefit design changes, including equalizing copayments and outpatient visit limits. The survey found 37 percent plan to change their copayments, 36 percent will change outpatient visit limits, and 29 percent will amend their out-of-network coverage features.
Employer responses also indicated that they plan to increase their use and promotion of wellness (35 percent) and employee-assistance (38 percent) programs.
“The current economic climate has exacerbated existing workplace mental health issues,” said William Bruning, J.D., cochair of the partnership's Advisory Council and president and CEO of the Mid-America Coalition on Health Care in Kansas City. “When employees who need mental health treatment receive it, productivity increases.”
The survey also found that mental health and substance abuse care were relatively inexpensive for employers. Only 9 percent of employers spent more than 5 percent of their health care budget on those two categories of care, and most did not expect that to change. Sixty-four percent of survey respondents said they expect parity implementation will reduce their costs, have no effect, or increase costs by less than 2 percent. Only 36 percent of respondents expected costs to increase by more than 2 percent.
“The business case for quality mental health care is there,” Bruning said.
But even small projected increases are important, experts have said, because strong federal parity legislation was stymied for decades by business leaders' long-standing concerns that parity requirements would greatly increase their health care costs. The new law allows employers to not adhere to parity requirements if their costs increase by more than 2 percent in the first year of parity and by more than 1 percent in subsequent years.
The survey results are posted at<www.workplacementalhealth.org/pdf/EmployerParitySurveyResults20090528.pdf>.▪