Patients with serious mental illness enrolled in the Medicare Part D prescription drug program who experienced problems accessing medications in the 12 months following initiation of the program in January 2006 were significantly more likely to visit an emergency department during that period.
Forty-four percent of patients who were dually eligible for Medicare and Medicaid experienced a problem accessing medications in the transition from Medicaid to Part D coverage. Among this group, the average predicted probability of visiting an emergency department was significantly greater than among those who did not experience an access problem.
“These findings are some of the first to look at the impact of Part D on dual-eligible patients with serious mental illnesses,” lead author Haiden Huskamp, Ph.D., told Psychiatric News. “We found that many dual eligibles had problems accessing medications after being switched from Medicaid drug coverage to a Part D plan and that individuals who did were more likely to use psychiatric ED [emergency department] care, raising concerns about negative impacts of Part D on quality of care for these individuals.
“Clinicians treating dual-eligible patients with mental illness need to be aware of the potential problems in accessing medications that may be experienced by their patients who are automatically assigned to plans that may or may not meet their medication needs,” she said.
Huskamp is an associate professor of health care policy at Harvard Medical School.
The findings were derived from a study of psychiatrists randomly selected from the AMA's master physician file and were reported in the September Psychiatric Services. The study analyzes data gathered by the American Psychiatric Institute for Research and Education (APIRE) on medication-access problems in the period January-December 2006. Darrel Regier, M.D, M.P.H., director of APIRE, and Joyce West, Ph.D., M.P.P., senior scientist with APIRE, are the coauthors.
(A previous study by APIRE on access problems based on Part D's first four months was published in the American Journal of Psychiatry in May 2007.)
In the new Psychiatric Services study, surveyed psychiatrists provided information on a final sample size of 908 dually eligible patients.
Each psychiatrist in the study was randomly assigned one of 21 start days and times to report on the next dually eligible patient treated during the psychiatrist's last typical workweek. For each patient included in the study on whom the psychiatrist reported, researchers obtained data on the patient's sociodemographic characteristics, treatment setting, diagnosis, and clinical characteristics and whether the patient experienced specific medication-access problems.
They also obtained information on emergency department visits related to the patient's psychiatric illness and psychiatric hospitalizations during the study period.
Individuals who did and did not experience medication-access problems were matched using “propensity score matching,” a statistical method of creating pairs while adjusting for confounding factors. After creating a matched sample of individuals who did and individuals who did not experience a medication-access problem, the researchers estimated two variables: the likelihood of having any emergency department visits and any hospitalization days for a psychiatric illness in the 12 months after initiation of the Part D program in January 2006, and the number of emergency department visits and hospital days.
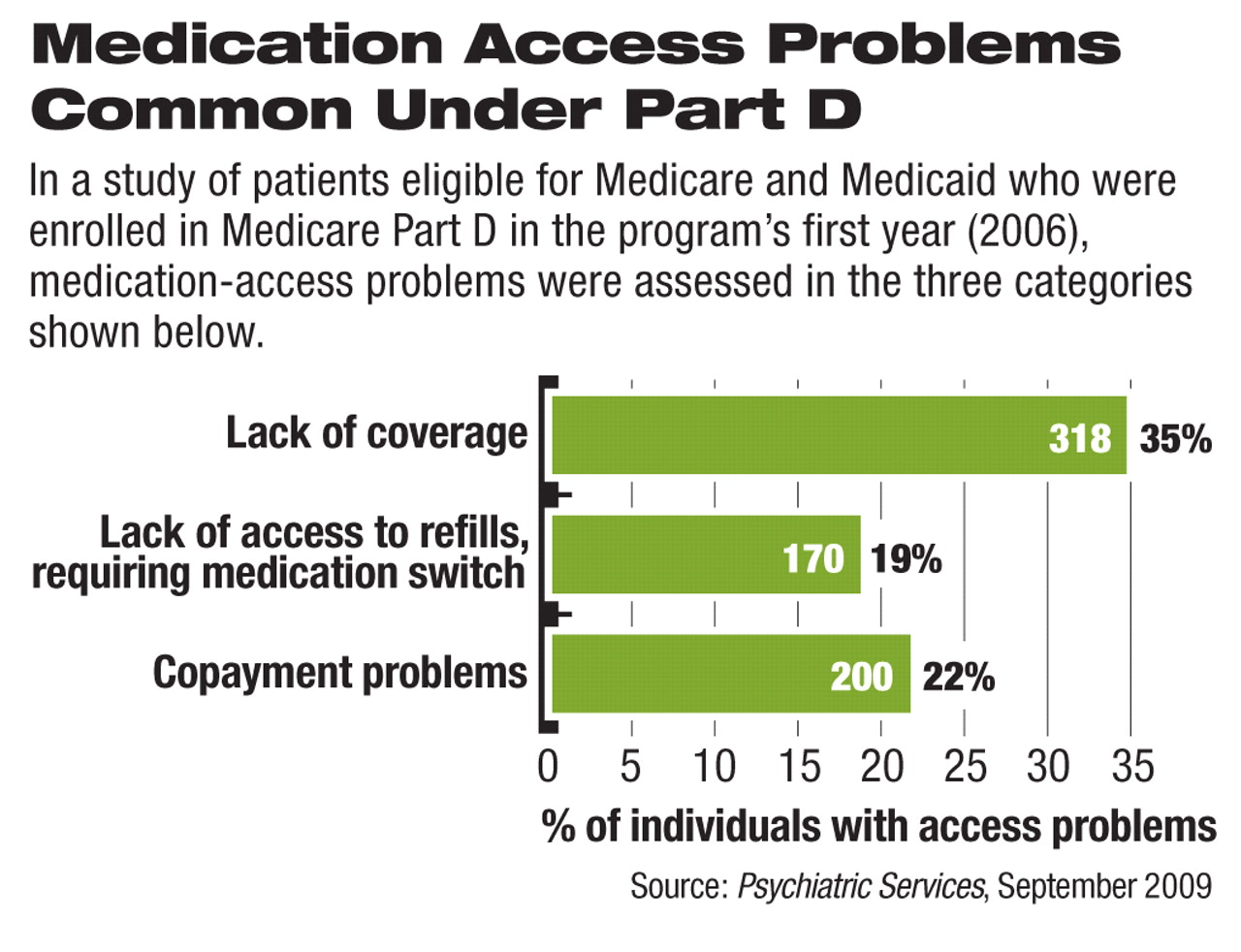
Three possible medication-access problems were assessed in the current study: being unable to access clinically indicated refills or new prescriptions because the drugs were not covered or approved, being stable on a clinically desired or indicated medication but switching to a different drug because refills were not covered or approved, and problems accessing medications because of copayments.
Huskamp and colleagues found that 400 patients, or 44 percent of the sample, had experienced one of the medication-access problems.
They also found that the mean predicted probability of visiting an emergency department was .41 for patients with an access issue and .27 for those with no access issue.
Does the study, which looked at the first 12 months after the initiation of the Part D program in 2006, suggest anything about the program today?
“One might expect access problems to be lower after the first year and the initial transitions,” Huskamp told Psychiatric News.“ However, each year since then, a large number of dual eligibles (for example, over 1 million for 2007 and over 2 million for 2008) were re-randomized to plans when the new year's premium for the plan they were enrolled in exceeded the benchmark for dual-eligible plans. Because of the re-randomization, one would expect a higher rate of medication-access problems for these individuals.
“Thus, medication-access issues due to plan switching or changes in plan coverage rules are likely to still be an issue for a large number of dual eligibles,” she said.