Research conducted in the past few years shows that ketamine leads to a rapid antidepressant effect within hours of administration. A recent study has demonstrated how this mood change translates into a tangible protection against suicidal ideation in treatment-resistant patients with depression (see
Ketamine Leaves BDNF Unchanged for more on ketamine treatment).
Ketamine is an anesthetic given intravenously that is often used in surgery and in veterinary medicine. It is known to cause psychosis and has raised abuse concerns.
In a paper published in the September 1 Biological Psychiatry, researchers at Mount Sinai School of Medicine, Rutgers University, and Harvard University conducted two clinical studies in which they assessed suicidal ideation in patients with treatment-resistant depression. The study was funded by the National Institutes of Health.
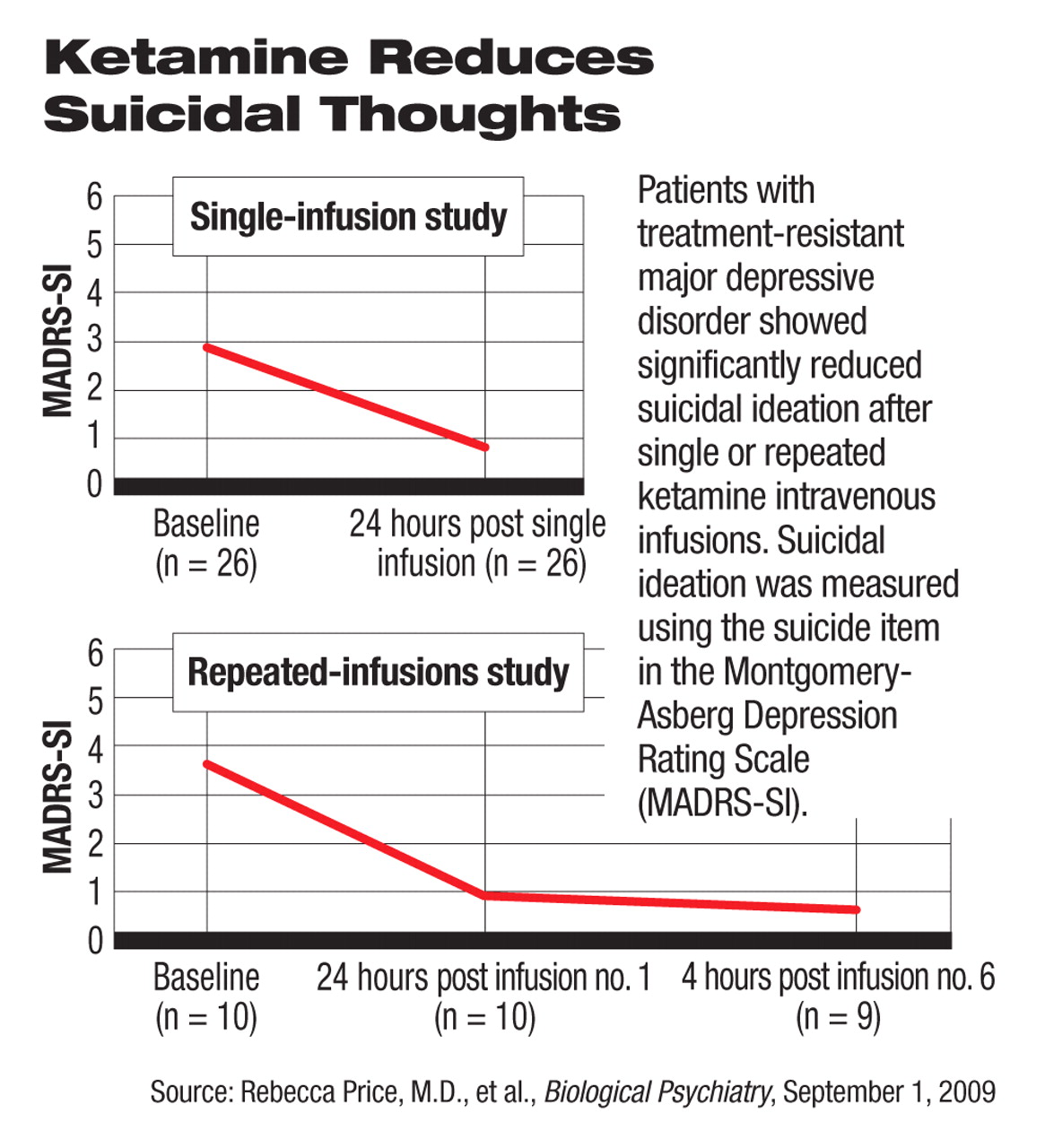
Twenty-six patients participated in the first study, in which each received a single infusion of ketamine at a dose of 0.5 mg/kg and was then kept in the hospital for 28 hours. Outcomes were measured 24 hours after the infusion using the single suicide-related item in the Montgomery-Asberg Depression Rating Scale (MADRS-SI). Scores ranged from 0 to 6, with a score of 6 indicating “explicit plans for suicide when there is an opportunity” or “active preparations for suicide.”
Subjects' mean score on the MADRS-SI scale decreased from 2.85 before the ketamine infusion to 0.77 at 24 hours after the infusion, which was statistically significant. Before the infusion, 13 patients had a score of 4 or above on the scale. Twenty-four hours after the infusion, eight of the 13 patients had a score of 0 or 1 and three had a score of 2 or 3; two remained at or above a score of 4.
Ten of the 26 patients also completed the Implicit Association Test, a behavioral-assessment instrument the researchers used to measure the implicit suicidal intention before and after the infusion. The implicit and explicit suicidal association scores also decreased significantly after the ketamine infusion.
Ten of the patients who had been deemed responders in the first study participated in the second study and received repeated ketamine infusions three times a week in a period of 12 days for up to six infusions. Their average MADRS-SI score was 3.0 at baseline. Nine patients scored 0 on the MADRS-SI scale after every repeated infusion. One patient had a score of 2 after the first infusion (baseline score 4). The patient was dropped from further infusion because of lack of response in overall depressive symptoms, defined as at least 50 percent reduction in MADRS total score.
The effect of ketamine on suicidal ideation was likely an indirect result of the antidepressant effect of the drug, the authors concluded after they analyzed the correlation between the total score of the nonsuicide-related items in the MADRS and the suicide-related item score. The 26 patients in the single-dose study had an average preinfusion MADRS total score of 37 (scale range 0-60), which decreased to 15 at 24 hours after the infusion. Seventeen of these patients had a 50 percent reduction in MADRS total score.
All study participants had moderate to severe depression as indicated by an Inventory of Depression Symptomatology score of 32 or above at baseline and had failed at least two adequate antidepressant trials in the current depressive episode. They had been suffering from major depressive disorder for a mean of 29 years. All had been in the current depressive episode for at least two years and failed an average of six antidepressants in the current episode. Five of the 26 participants had a history of suicide attempts.
No patient experienced hallucinations during the studies, Rebecca Price, M.S., a Ph.D. candidate in psychology at Rutgers University and the lead author of the article, told Psychiatric News. The psychotomimetic side effects observed in the studies were “minimal” at this low dose of ketamine, she said, and additional results and analyses are pending publication.
The rapid antidepressant effect of ketamine infusion has previously been reported in small clinical trials conducted by researchers at the Mood and Anxiety Disorders Program at the National Institute of Mental Health (NIMH). The NIMH researchers also demonstrated that ketamine's mechanism of action may lie in its antagonism of the NMDA (N-methyl d-aspartate) receptors and subsequent activation of the AMPA (amino-3-hydroxy-5 methylisoxazole-4-propionic acid) receptors; both are biologically activated by the neurotransmitter glutamate (Psychiatric News, September 7, 2007).
An abstract of “Effects of Intravenous Ketamine on Explicit and Implicit Measures of Suicidality in Treatment-Resistant Depression” is posted at<www.journals.elsevierhealth.com/periodicals/bps/article/S0006-3223(09)00519-8/abstract>.▪