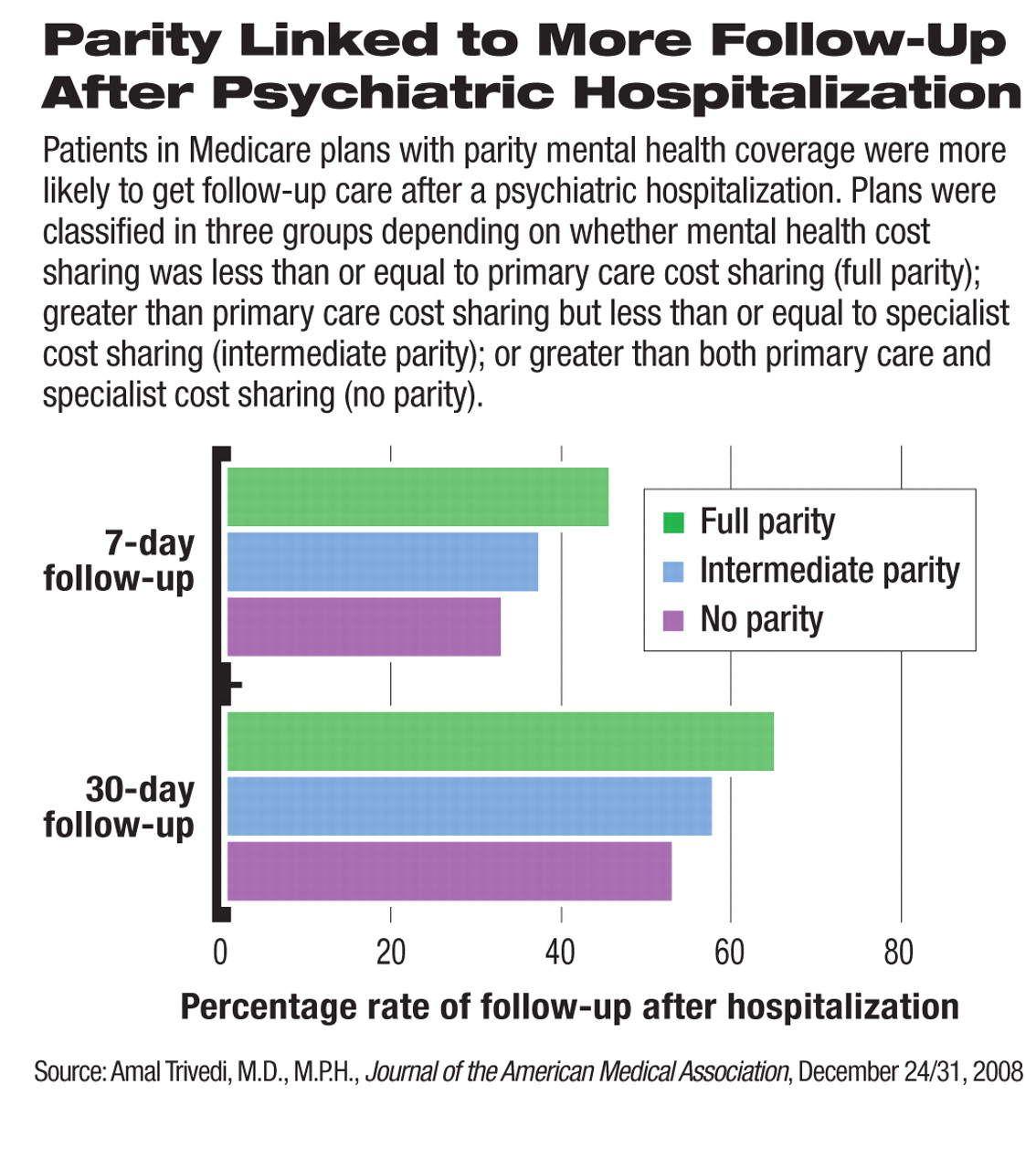
Individuals in Medicare plans with insurance parity for mental health appear to have markedly higher use of clinically appropriate mental health services following a psychiatric hospitalization than do people in plans without parity.
A review of cost-sharing requirements in Medicare health plans and follow-up services after hospital discharge for enrollees in those plans showed that individuals in full-parity plans were more likely to visit a mental health practitioner within seven to 30 days after a hospitalization compared with enrollees in Medicare plans with intermediate or no parity.
Moreover, the association of parity with follow-up care was even stronger for enrollees from areas of low income and with less education.
The report appears in the December 24/31, 2008, Journal of the American Medical Association, (JAMA).
“In this study of mental health insurance parity, copayments that were $14 greater in plans without parity compared with full-parity plans were associated with an 11 percentage point–lower rate of follow-up after a psychiatric hospitalization,” wrote lead author Amal Trivedi, M.D., M.P.H., and colleagues. “The association of parity with follow-up visit rates was increased by a factor of 1.4 for enrollees in the lowest quartiles of ZIP code–level income and 1.7 for enrollees in the lowest quartile of ZIP code–level education.”
Trivedi, a professor in the Department of Community Health at Brown University's Warren Alpert Medical School, noted that the study is broadly consistent with results from the RAND Health Insurance Experiment. That study found that mental health services are more sensitive to cost sharing than other medical services and that the effect of cost sharing is increased in vulnerable subgroups.
Although follow-up care after hospitalization is associated with improved outcomes, Trivedi acknowledged that he and colleagues “were unable to determine whether the higher proportion of follow-up visits in full-parity plans was associated with lower rates of rehospitalization.”
Mental health services researcher Howard Goldman, M.D., who reviewed the study for Psychiatric News, said that seven- and 30-day follow-up after hospitalization is a standard measure of quality used by the Healthcare Effectiveness Data and Information Set (HEDIS). This tool is used by most commercial health plans to measure performance on important dimensions of care and service.
“When you are dealing with administrative data, it's true that you can't directly measure quality, but follow-up after hospitalization is an accepted measure in mental health services research,” Goldman said.
He added that rehospitalization is no better a measure of quality since access to rehospitalization may be vital and that higher rates—rather than lower rates—could be indicative of better quality care.
Goldman is editor of the APA journal Psychiatric Services and lead author of a landmark 2006 study on the effect of parity on cost and out-of-pocket spending in the Federal Employees Health Benefits Program (FEHBP).
In their study, Trivedi and colleagues reviewed cost-sharing requirements for outpatient mental health and general medical services for 302 Medicare health plans from 2001 to 2006. Among 43,892 people who were enrolled in 173 health plans and who were hospitalized for a mental illness, the researchers determined the relation between parity in cost sharing and receipt of timely outpatient mental healthcare after discharge using cross-sectional analyses of data from the Medicare plans.
They classified plans into three groups depending on whether the health plan's mental health cost sharing was less than or equal to primary care costsharing (full parity), greater than primary care cost sharing but less than or equal to specialist cost sharing (intermediate parity), or greater than both primary care and specialist cost sharing (no parity).
The researchers also performed longitudinal analyses comparing 10 plans that discontinued parity between December 2002 and January 2006 with 10 matched-control plans that maintained parity. Each plan was randomly matched to one control plan, stratifying by U.S. Census region and tax status.
Across all years of the study, 47 percent of the enrollee observations (16,224,431) were from Medicare plans with no parity, 32 percent were from plans with intermediate parity (11,058,364), and 21 percent were from plans with full parity (7,195,442).
Adjusting for individual and health plan characteristics, the investigators found that rates of follow-up within seven and within 30 days after a psychiatric hospitalization were greater in plans with equivalent cost sharing for mental health and primary care versus plans with mental health cost sharing greater than cost sharing for primary and specialty care.
For individuals in the lowest quartile of area-level education, the 30-day follow-up rate was 18.3 percentage points lower in plans with no parity versus plans with full parity.
In the 10 plans that discontinued parity, rates of outpatient follow-up decreased, while the rates increased in the 10 control plans that maintained parity. In eight of those plans with two years of data before discontinuing parity, rates of follow-up within seven days were 47.0 percent in the year prior to discontinuation and 37.9 percent in the year following. Researchers observed similar trends for rates of 30-day follow-up.
Goldman said the JAMA study refined the understanding of parity by focusing on quality of care.
“This study represents a significant advance over the work we did on the FEHBP in that it is able to make a more direct comparison between plans with higher cost sharing and plans with lower cost sharing and showed that lower cost sharing is associated with higher quality care on the measure of follow-up after inpatient care,” Goldman said.
“We don't know anything about what the cost impact was, but it does move the field further and provides another reason to expand parity because it promotes quality care.”