Many Americans seem to have become enamored with complementary or alternative medicine (CAM). The evidence? They spent $14 billion for CAM in 1990, according to a study reported in the January 28, 1993, New England Journal of Medicine. In 2007, the figure was a whopping $34 billion, according to figures released by the National Center for Complementary and Alternative Medicine in July 2009.
And some of this money is going for mental-health-related issues.
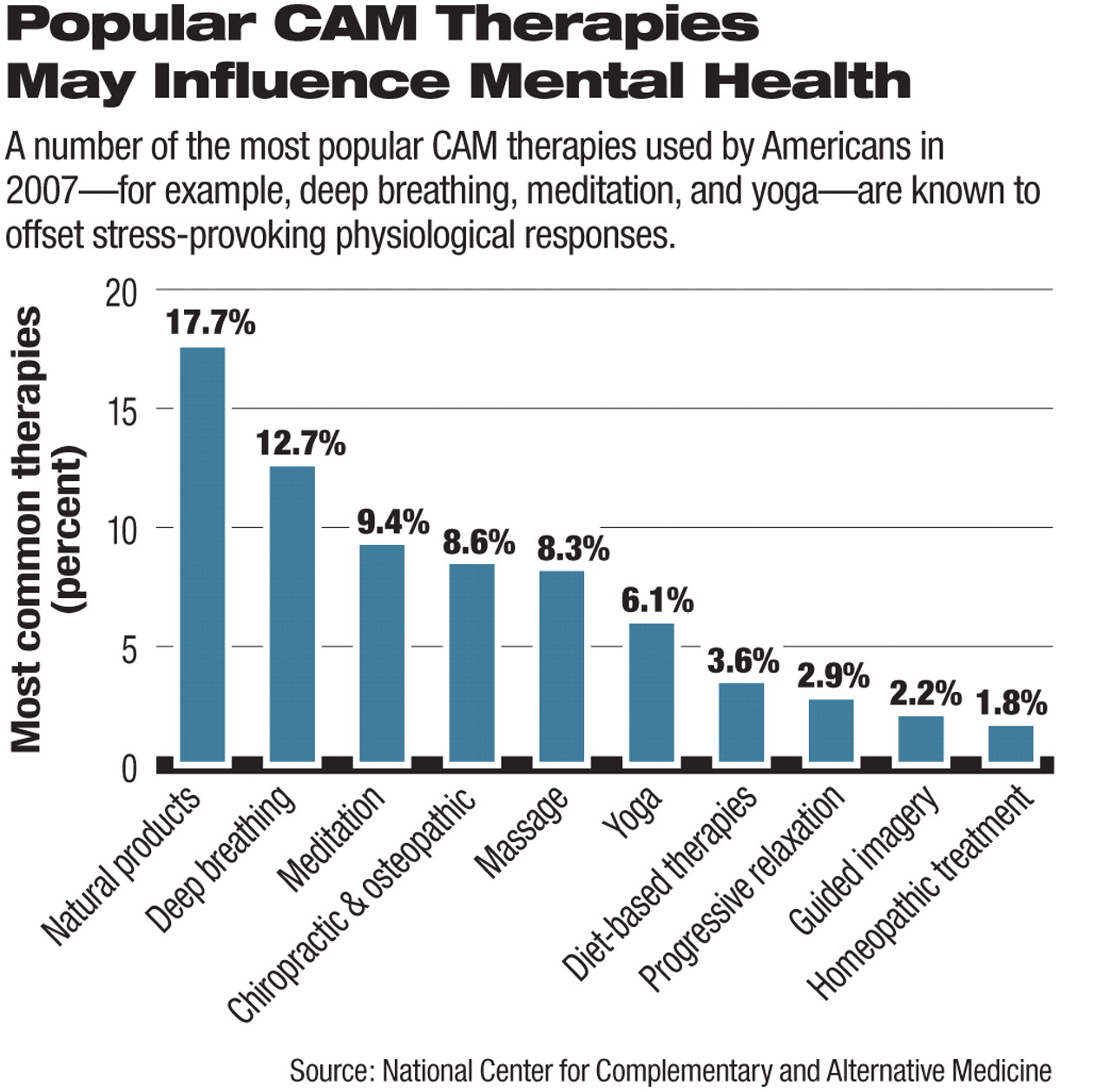
For example, three of the most popular CAM therapies used by Americans in 2007 were deep breathing, meditation, and yoga, and two of the most poplar natural products used by them in 2007 were fish oils/omega-3 fatty acids and ginkgo biloba. Anxiety was one of the top five reasons why Americans used CAM in 2007.
So does any of the CAM applied to mental health actually help?
Results from the nascent CAM—mental health research field show promise in some cases, but history also shows that promising therapies have later proved to be of no benefit.
For example, there is now ample evidence that meditation, yoga, and other relaxation responses can offset stress-provoked physiological responses. There is even reason to speculate that such techniques may help extend life, a study reported in the December 1989 Journal of Personality and Social Psychology suggested. Seventy-three elderly nursing home residents were randomly assigned to meditation, mindfulness, or no treatment daily (thus serving as a control group). All were followed for a three-year period. At the end of that time, all of the meditation group and 88 percent of the mindfulness group were alive; only 40 percent of the control group was.
Evidence has been mounting that the omega-3 fatty acids can be of value in preventing and treating depression and bipolar disorder and may even help combat borderline personality disorder (Psychiatric News, August 3, 2001; January 17, 2003; January 16, 2004). Ginkgo biloba has been shown to improve the attention, memory, and cognitive speed of some cognitively healthy subjects (Psychiatric News, January 2, 2009).
Exercise seems capable of helping prevent depression in men and women, a recent large study found (Psychiatric News, January 2, 2009). This study especially impressed Trisha Suppes, M.D., Ph.D., she said during a recent interview. Suppes, a professor of psychiatry at Stanford University, has conducted some CAM—mental health research.
“There is some indication that acupuncture may be helpful for depression during pregnancy and as an adjunct to antidepressants,” Rosa Schnyer, DAOM, L.Ac., told Psychiatric News. Schnyer is a clinical assistant professor of pharmacy at the University of Texas, Austin, and a CAM—mental health investigator.
Lesser-Known Remedies Promising
Some lesser-known CAM—mental health remedies also may be beneficial.
N-acetylcysteine, an amino acid available from health-food stores, can help counter trichotillomania, according to a randomized, double-blind, placebo-controlled study of 50 subjects with the disorder. The senior investigator was Suck Won Kim, M.D., an associate professor of psychiatry at the University of Minnesota. Results were published in the July 2009 Archives of General Psychiatry.
Chamomile has mild antianxiety activity in persons with generalized anxiety disorder, a randomized, double-blind, placebo-controlled trial of 57 subjects with the disorder found. The study was conducted by Jay Amsterdam, M.D., a professor of psychiatry, Jun Mao, M.D., an assistant professor of family medicine and community health, and colleagues at the University of Pennsylvania. Results appeared in the August 2009 Journal of Clinical Psychopharmacology.
In another study, 56 healthy men and women were exposed to the aroma of lavender, the aroma of lemons, or to a no-odor substance (water) during three visits. Self-reports and unobtrusive mood measures provided significant evidence that lemon oil enhanced positive mood compared with lavender or water. The study, which was headed by Janice Kiecolt-Glaser, Ph.D., a professor of psychiatry at Ohio State University, was published in the April 2008 Psychoneuroendocrinology.
Body therapy, which consists of training patients to become aware of their inner-body experiences while being massaged, significantly reduced dissociation in subjects who had been sexually abused as children. A reduction in dissociation is considered important to recovery from sexual abuse. The study was headed by Cynthia Price, Ph.D., a research assistant professor at the University of Washington. Results appeared in the May 2007 Complementary Therapies in Clinical Practice.
And when vitamin D and a chemical in the herb turmeric, called curcumin, are combined, they may be able to fight Alzheimer's, an in vitro experiment suggested. Immune cells from Alzheimer's patients were incubated with beta-amyloid plaques, a biological hallmark of Alzheimer's; vitamin D; and curcumin. Curcumin helped the immune cells bind to the plaques; vitamin D then helped the immune cells destroy the plaques. Results appeared in the July 2009 Journal of Alzheimer's Disease.
Other Studies Disappoint Advocates
However, some of the CAM—mental health therapies that looked especially promising have turned out to be disappointing. A notable one is St. John's wort for major depression, according to a study by Jonathan Davidson, M.D., a professor of psychiatry at Duke University. He and his colleagues concluded that there was no evidence from their study to “support the efficacy” of the herb in moderately severe major depression. Results were published in the April 10, 2002, Journal of the American Medical Association (JAMA) (Psychiatric News, May 17, 2002).
Additionally, ginko biloba was not found to be effective in preventing Alzheimer's. The trial, headed by Steven DeKosky, M.D., of the University of Virginia and a leading Alzheimer's scientist, was conducted at five academic medical centers throughout the United States. It included more than 3,000 community volunteers aged 75 or older and used a randomized, placebo-controlled, double-blind design (Psychiatric News, January 2, 2009).
Some lesser-known attempts to deploy CAM for psychiatric illness have disappointed as well. For example, St. John's wort was found to be no better than a placebo in countering obsessive-compulsive disorder, according to a study headed by Kenneth Kobak, Ph.D., of the Dean Foundation for Health Research and Education and published in the November 2005 International Clinical Psychopharmacology. And St. John's wort fared no better than a placebo in countering attention-deficit/hyperactivity disorder in children and adolescents. The lead investigator was Wendy Weber, Ph.D., then with Bastyr University School of Naturopathic Medicine and now with the National Center for Complementary and Alternative Medicine. Findings appeared in the June 11, 2008, JAMA.
As the CAM—mental health field picks up momentum, undoubtedly more will be learned about which remedy may work for which indication. For instance, Suppes and her colleagues want to learn whether Veterans Administration patients are using CAM remedies for various psychiatric disorders and, if so, whether they are receiving any benefits from them.
Some Questions Demand Answers
But some questions are especially urgent, researchers in the field believe.
“Many alternative medicines are used for depression, dementia, decreased libido, and alcoholism,” Kim noted. “We need more information in these areas.”
“People sometimes take vitamins or combinations of vitamins in lieu of treating their bipolar disorder,” said Suppes. “In terms of risks and benefits, it would be important to examine that scientifically.”
“For CAM practices that have a long record of safety (i.e., acupuncture, meditation, imagery, yoga, etc.), effectiveness and outcome studies should come first,” Schnyer asserted.
But should psychiatrists ever recommend to their patients they use CAM for mental health—and if so, for which conditions? CAM—mental health authorities hold different opinions.
“I recommend the omega-3 fatty acids routinely for a number of health benefits,” Kim reported.
“I tend to be very evidence-oriented,” said Suppes. “So I would not recommend CAM that has not been studied. But what I do endorse and recommend to patients is a healthy lifestyle, which includes eating fresh foods, exercising every day, and sleeping regularly. Yes, I'm positive about CAM, but I also believe in the need to study it.”
“Omega-3 fatty acids, St. John's wort, and some other biologically based CAM therapies can be extremely helpful, but care should be taken when combining them with pharmaceutical drugs,” Schnyer cautioned. “It's a good idea to consult with CAM practitioners before recommending these types of CAM therapies to patients.”
“Yoga and tai chi can promote self-efficacy, which is often lacking in mentally ill people,” Mao observed. “So encouraging them to use such modalities could be beneficial. But with many CAM treatments, you should take a number of factors into consideration before recommending them. For instance, how safe is the therapy? How effective? What are the alternatives? And how much does it cost? Cost is particularly important for patients since a lot of CAM is not reimbursed by health insurance companies.”
“Ultimately, the most valuable contribution that CAM can make to mental health,” Schnyer predicted, “is not a series of modalities that may be helpful, but a change in how we view illness and the process of getting well.”
More information about CAM for mental health indications is posted at <www.nccam.nih.gov> and can be found in the book Complementary and Alternative Treatments in Mental Health Care, edited by James H. Lake, M.D., and David Spiegel, M.D., published by American Psychiatric Publishing Inc.