Antipsychotic medications increase patients' risk of developing diabetes, some studies have suggested. A new study now provides more evidence of such a concern. But it also suggests that the risk varies considerably depending on the antipsychotic used, the duration of use, and whether more than one antipsychotic is used.
This new study appears to be the largest and longest exploring the subject. It was headed by Lars Vedel Kessing, M.D., a professor of psychiatry at the University Hospital of Copenhagen in Denmark. Results were published in the October British Journal of Psychiatry.
In Denmark, all 5 million or so residents have a unique personal identification number that is recorded in linked registers whenever they receive medical services or purchase medications. Kessing and his coworkers used data in these registers to select their study sample—some 346,000 individuals who had purchased antipsychotics between 1996 and 2005 as well as some 1,427,000 individuals (about a third of the total Danish population) who had not. More than 50,000 people were diagnosed with diabetes in that period.
In reviewing the data, the researchers found a link between having been diagnosed with diabetes and taking an antipsychotic medication during the 10-year study period, even when some possibly confounding factors—age, gender, calendar period, and the use of lithium or anticonvulsants—were considered.
Compared with unexposed individuals, those receiving a first-generation antipsychotic medication such as zuclopenthixol, perphenazine, or haloperidol had a diabetes rate of 1.53, and those receiving a second-generation antipsychotic medication had a diabetes rate of 1.32. However, the rates of diabetes varied substantially among the second-generation antipsychotic medications.
For example, the rate was between 1.17 and 1.57 for those taking olanzapine, risperidone, or clozapine, and 2.00 or more for those taking ziprasidone or sertindole. In contrast, there was no significantly increased rate of diabetes in those taking amisulpride, quetiapine, and aripiprazole.
Finally, for individuals on either first-generation or second-generation antipsychotic medications, the rate of diabetes increased with duration of treatment and the number of antipsychotics the patients took.
For instance, the rate of diabetes was 0.98 in subjects who had purchased one or two second-generation antipsychotic prescriptions, 1.30 in subjects who had purchased 20 to 24 of them, and 1.81 in subjects who had purchased 40 or more. Along similar lines, the rate of diabetes was 1.48 in subjects using one antipsychotic medication, 2.38 in subjects using four, and 3.41 in subjects using five or more.
The study had no outside funding.
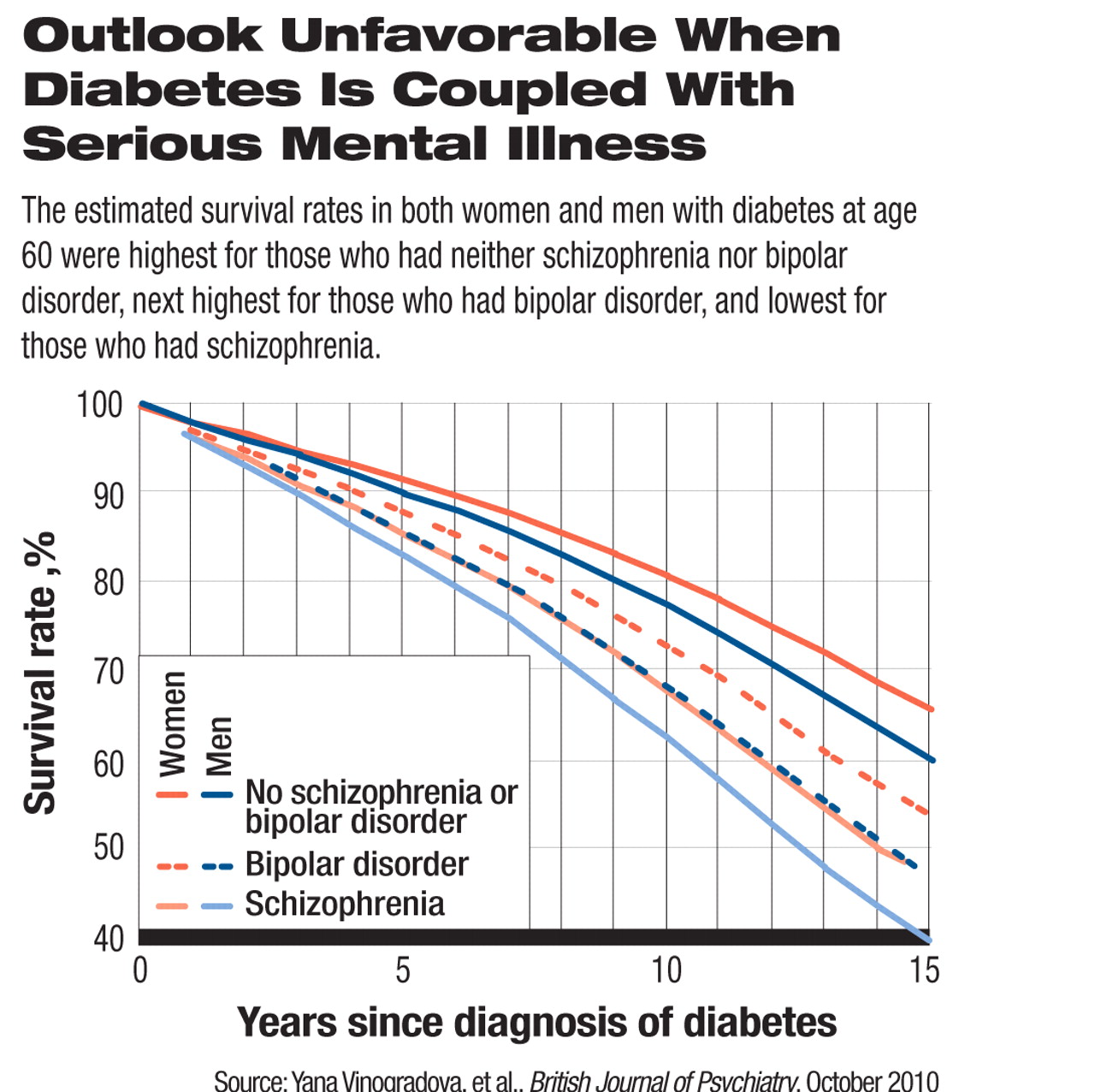
In a related study also published in the October British Journal of Psychiatry, British researchers reported that individuals who have both schizophrenia and diabetes or both bipolar disorder and diabetes have a significantly increased risk of death compared with individuals with diabetes alone.
The cohort included some 44,000 people with diabetes. Out of these subjects, 257 also had schizophrenia, 159 also had bipolar disorder, and 14 had been diagnosed with both schizophrenia and bipolar disorder. Their survival rates between 2000 and 2005 were the focus of the study.
There are several possible explanations for the results, the researchers believe.
One is that in people with schizophrenia and diabetes or in people with bipolar disorder and diabetes, diabetes may be more poorly controlled than in people with diabetes alone. However, a study by other researchers does not support this explanation, they pointed out. It found that diabetes care in the United Kingdom is as good for people with schizophrenia or bipolar disorder as for those without it.
Another explanation is that people who have schizophrenia or bipolar disorder and diabetes have more comorbid physical illnesses than people with diabetes alone.
The researchers did not address the possibility that people with schizophrenia and diabetes or with bipolar disorder and diabetes are at increased risk of death because they do not take good care of themselves in ways other than diabetic control or because of suicide.
This study was headed by Yana Vinogradova, M.Sc., of the University of Nottingham and funded by that university and the U.K. Disability Rights Commission.