Screening for psychiatric illness in adults and children nationwide is expected to increase as coverage mandates in the new health care law for both private and public insurance programs go into effect over the next few years. And that increase could help cut the rates of untreated mental illness, said mental health advocates.
Supporters of increased access to mental health care gathered for a Capitol Hill briefing in November to hail the expected benefits of the health care reform law. Those benefits came via provisions that include a requirement that all health insurance plans participating in the new state health insurance exchanges—planned for launch by 2014—cover services recommended by the U.S. Preventive Services Task Force (USPSTF), the Advisory Committee of Immunization Practices at the Centers for Disease Control and Prevention, and the Health Resources and Services Administration.
Among the recommendations are an annual depression screening for all youth aged 12 to 18 and depression screenings for adults “when staff-assisted depression care supports are in place to ensure accurate diagnosis, effective treatment, and follow-up,” according to the USPSTF.
Importantly, the law mandates that all insurance plans that were issued after September cover 100 percent of the cost of preventive care, including mental health screenings, when they are offered by innetwork providers.
These coverage requirements serve only as a floor, and thus more-generous screening coverage requirements established in some states could remain in place.
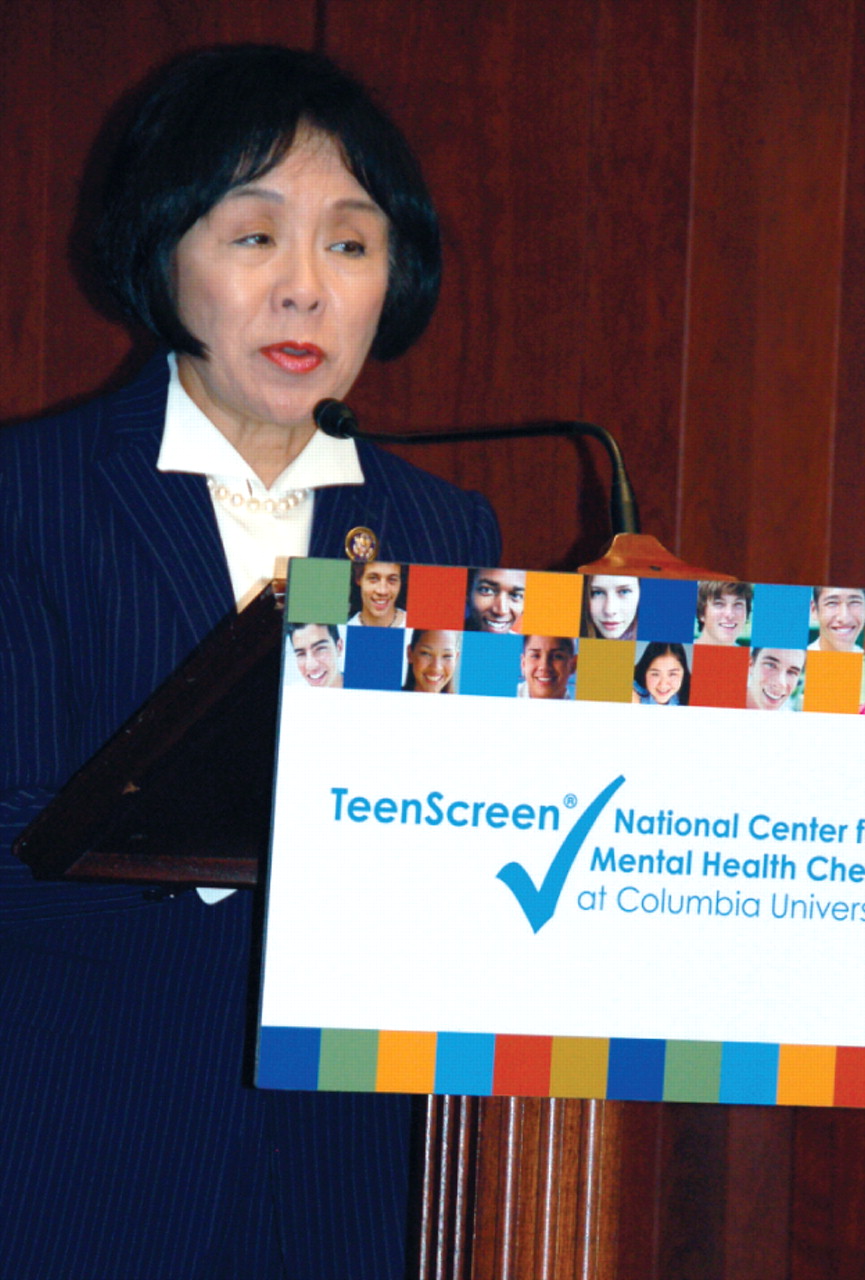
“There are too many people who do not receive the care they need,” said Rep. Doris Matsui (D-Calif.) at the November briefing, which was sponsored by the TeenScreen National Center for Mental Health Checkups at Columbia University. “This law will help address that.”
As a member of one of the committees that wrote the House version of the health care legislation, Matsui advocated for the inclusion of preventive care and “wellness provisions.”
Also included in the law was an expansion of the federal Medicaid Early and Periodic Screening, Diagnostic, and Treatment benefit, which includes a mental health assessment as part of its covered well-child visits. Many Medicaid plans are required to offer such assessments to comply with the requirements of the federal insurance parity law enacted in 2008. The parity law requires most private insurers to offer the same level of coverage for screening, diagnosis, and treatment of psychiatric disorders as they do for other types of medical conditions.
Researchers and public-health policymakers have long touted the benefits of mental health screening, including that for substance use disorders, in primary care, which is the only medical point of contact for the vast majority of the population. They maintain that routine screening for mental illness is the most effective way to lower the rate of untreated mental illness, which in 2009 stood at 62 percent of people with symptoms of such illness, according to a Substance Abuse and Mental Health Services Administration (SAMHSA) report released in November. Additionally, 40 percent of people with symptoms of serious mental illness were found to have gone without treatment, according to the SAMHSA report.
The economic cost of such widespread lack of needed treatment—which shows up in disability, unemployment, substance abuse, homelessness, inappropriate incarceration, suicide, and “wasted lives”—is more than $100 billion annually, according to the National Alliance on Mental Illness.
“If care providers consistently screen and intervene with early-stage substance abuse, the health care system can avert enormous human and economic costs,” said A. Thomas McLellan, Ph.D., deputy director of the Office of National Drug Control Policy, in testimony before a House of Representatives subcommittee in June.
The need for increased mental illness prevention and early-detection efforts also has been stressed as critical by suicide-prevention advocates, who note that the vast majority of suicide victims had untreated mental illness.
Kelly Kelleher, M.D., director of the Center for Innovation in Pediatric Practice, praised the ability of screening tools to help detect psychiatric conditions, especially in children.
“Early detection is key,” said Kelleher, during the November Capitol Hill briefing. “The earlier we can identify these conditions, the better the chance we have to treat and reverse their effects.”
As a member of the American Academy of Pediatrics Task Force on Mental Health, Kelleher helped develop a mental health toolkit for pediatricians that incorporates mental health screening in patient visits.
A key federal official, Richard Frank, Ph.D., deputy assistant secretary for planning and evaluation at the Department of Health and Human Services, also hailed the promise of screening tools to help detect illness early when it is most amenable to treatment and to get psychiatric treatment to people who might not otherwise seek it out. The health law's provisions are expected to spur wider use of these screening tools, which physicians have not widely adopted in the past due in part to a lack of insurance reimbursement for them.
“This area is ripe for movement now,” Frank said, about the expanded screening coverage requirements in the health care law.