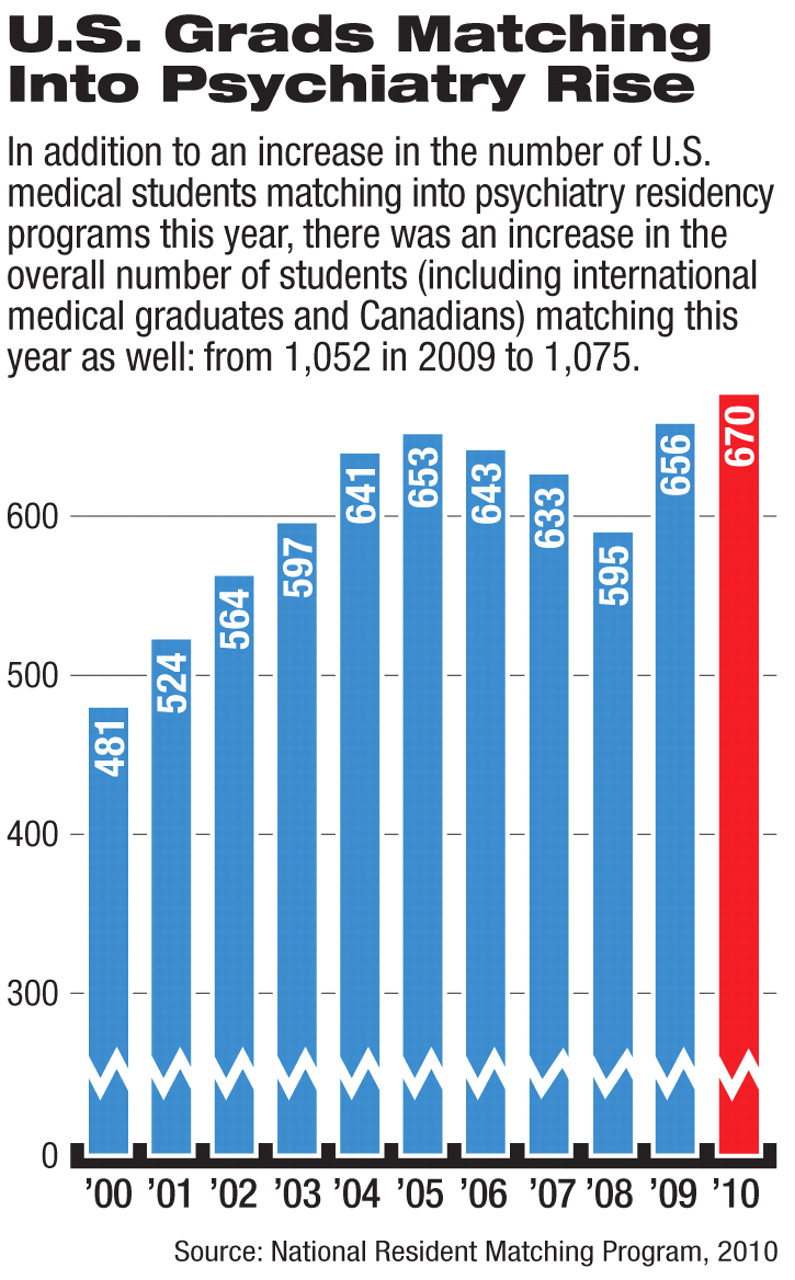
A total of 670 U.S. medical school graduates matched into psychiatry residency positions in this year's National Resident Matching Program (NRMP), exceeding last year's total of 656.
The percentage of matching graduates in psychiatry was the same as last year—4.5 percent. That percentage has remained relatively stable since 2006.
In all, 1,075 psychiatry residency slots were filled. As in the past, the positions not filled by U.S. medical graduates were filled by international medical graduates (U.S. and non-U.S. citizens), Canadian students, and students who graduated from medical school in previous years.
The match—in which the choices of graduating medical students are “matched” with those of residency programs—is typically watched as an indicator of workforce size and makeup in the various medical specialties for the coming years.
One notable feature of this year's match was its size: 30,543 applicants participated, the largest number in history, according to the NRMP.
But perhaps most notable was the increase in the number of students matching into primary care specialties. There was a 9 percent increase over 2009 in the number of U.S. medical school seniors who matched with residency positions in family medicine. And there was a 3 percent increase for internal medicine and a 2 percent increase for pediatrics.
“The AAMC is extremely encouraged that more graduating U.S. medical students this year chose primary care for their residency training,” AAMC President Darrell Kirch, M.D., said in a statement. “The increases for family medicine, internal medicine, and pediatrics in this year's match are welcome steps in the right direction for improving our health care system and our nation's health.
“Many factors go into a new doctor's choice for residency training. An AAMC survey last fall indicated that nearly 50 percent of U.S. medical schools had instituted or were considering programs or policies to encourage interest in primary care. We believe the results of this year's match demonstrate that the nation's medical schools are making progress in their efforts to encourage more new doctors to pursue careers in primary care. A strong primary care system is an essential part of good medicine.”
Other notable trends of the match this year include the following:
•.
Neurological surgery, orthopedic surgery, dermatology, and otolaryngology were the most competitive fields for applicants. At least 90 percent of those positions were filled with U.S. medical school seniors.
•.
All but five positions were filled of the 1,187 available in obstetrics-gynecology, and 915 positions were filled by U.S. seniors, a number that has increased for the sixth consecutive year.
•.
The number of U.S. medical school seniors going into emergency medicine increased for the fifth consecutive year. That field filled 1,182 of the 1,556 first-year positions.
For psychiatry, this year's numbers reflect stability—though the specialty is one of the less competitive residencies, it continues to attract a small percentage of medical students interested in the brain, mind, and behavior.
Sidney Weissman, M.D., a former APA trustee and past president of the American Association of Directors of Psychiatric Residency Training who has maintained a long-time interest in workforce trends, believes that the evidence that both psychological and somatic therapies affect the brain, mind, and behavior is a feature that can make psychiatry attractive to tomorrow's physicians.
“Psychiatry has a unique opportunity in the next three years to impact recruitment,” he said in an analysis of match results he sends to interested parties each year. “The publication of DSM-5 in 2013 means that psychiatry as a discipline will be in the spotlight. We must use it effectively to showcase our field.
“I believe we must alter some of our language. We speak of pharmacotherapy and psychotherapy. The former impacts on the brain, but people are left to wonder where psychotherapy works. I would propose, since all therapy impacts on the brain and all therapy alters psychological functioning, we might describe psychotherapy as has having two functions—somatic and psychological. The publication of the new DSM gives us an opportunity to address our use of language.”