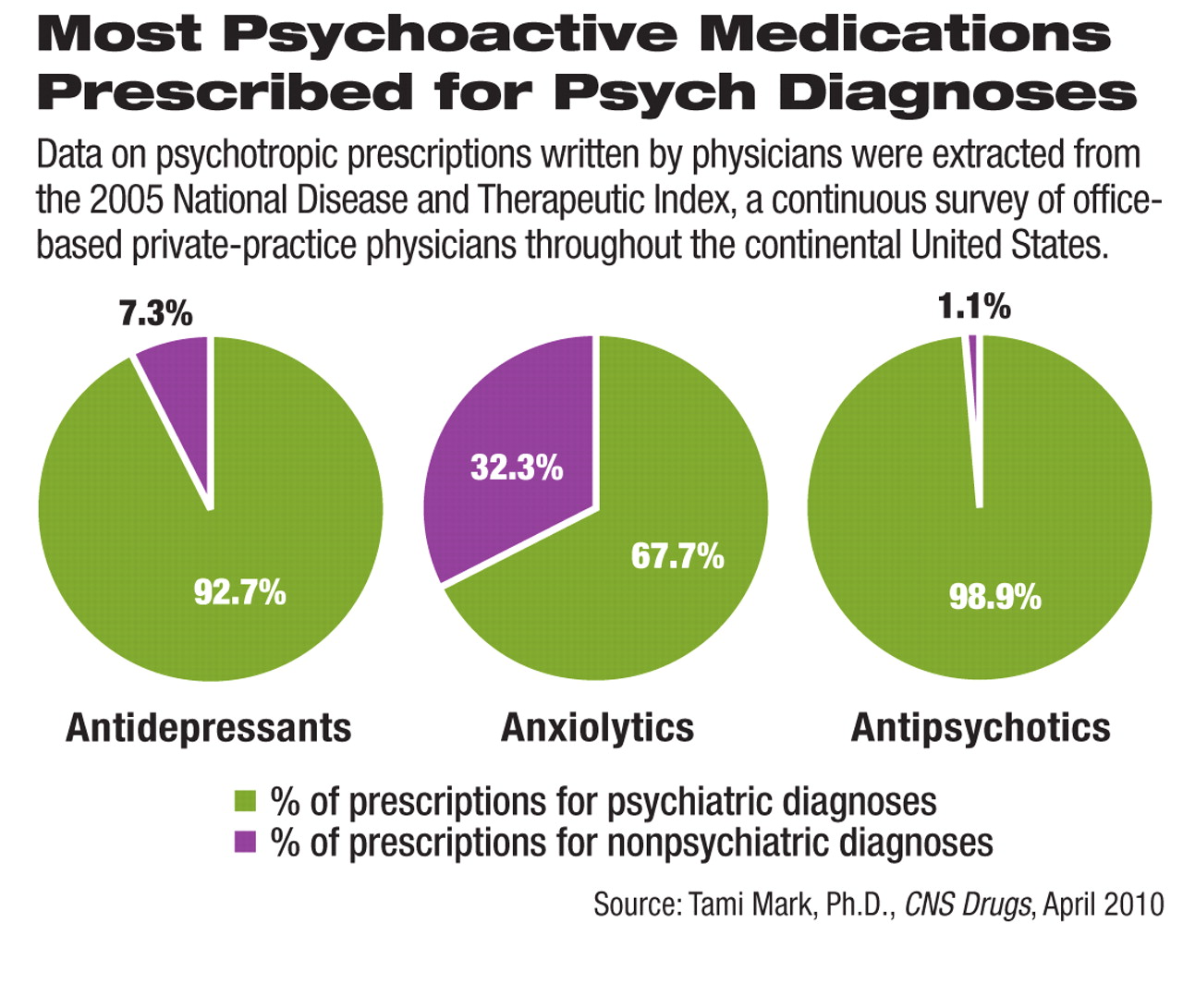
A very small minority of antidepressant and antipsychotic prescriptions and about one-third of antianxiety prescriptions are written for nonpsychiatric diagnoses, according to a recent analysis of national physician survey data.
The use of psychoactive drugs has risen rapidly since the 1990s, and expenditures for this category have grown faster than the total prescription drug market. This trend has raised concerns that psychoactive drugs are being prescribed excessively and too frequently for unapproved uses. Research and debate about off-label prescribing of psychiatric drugs have focused on unapproved uses within the realm of psychiatric disorders, and very little is known about whether these drugs are used for nonpsychiatric diagnoses such as pain.
The study, by Tami Mark, Ph.D., director of analytic strategies at Thomson Reuters, examined physician-reported data in the National Disease and Therapeutic Index, a continuous survey of physicians conducted by IMS Health, a private market-research company. The survey randomly selects a representative sample of 4,000 physicians every quarter from office-based physicians in private practice within the continental United States. Each participating physician is surveyed by telephone on two consecutive days per month and asked about the diagnoses and associated treatment in every patient visit during these two days. Multiple diagnoses and prescriptions may be reported for each visit.
The study analyzed data from 2005 and included three major types of psychoactive medications: antidepressants, antianxiety drugs, and antipsychotics.
Of the antidepressants prescribed in 2005, 92.7 percent were associated with psychiatric diagnoses. About two-thirds (65.3 percent) were prescribed for mood disorders, and 16.4 percent for anxiety disorders (see chart). The nonpsychiatric diagnoses associated with antidepressant prescriptions included headaches, connective tissue diseases such as fibromyalgia, nervous-system disorders other than the psychiatric diagnoses defined in ICD-9-CM codes 290-314, and female disorders such as premenstrual tension.
Antipsychotics were prescribed almost exclusively (98.9 percent) for psychiatric diagnoses. The most common indications were mood disorders (39.0 percent) and schizophrenia and other psychotic disorders (34.5 percent).
Certain uses of antipsychotics are controversial, and the study did not directly analyze whether these psychoactive drugs were used for unapproved psychiatric indications. The data showed that 7.4 percent of the antipsychotics were prescribed for delirium, dementia, amnestic disorders, or other cognitive disorders commonly diagnosed in the elderly. A mandatory boxed warning in all antipsychotic drug labels states that this type of use is associated with increased risk of death. About 1 in 20 (5.7 percent) antipsychotic prescriptions was written for attention-deficit/hyperactivity disorder, conduct disorder, or disruptive behavior disorders, and 2.3 percent of the antipsychotics were prescribed for other psychiatric disorders usually diagnosed in infancy, childhood, and adolescence, such as autism. This use is also controversial. However, the study did not include the age of patients in the analysis.
Although the antianxiety class was associated with the lowest proportion of psychiatric diagnoses, two-thirds (67.7 percent) of the prescriptions were written for psychiatric disorders. The diagnosis of an anxiety disorder was linked to 39.6 percent of the prescriptions, and mood disorders accounted for 18.9 percent.
Among the uses not associated with a psychiatric diagnosis, preparation for medical examination or procedures was the reason for 6.0 percent of the antianxiety-drug prescriptions. In addition, allergic reactions were cited in 4.1 percent of these prescriptions. Indications related to back pain accounted for 2.5 percent of the prescriptions.
The study was sponsored by the Substance Abuse and Mental Health Services Administration and published in the April CNS Drugs.