In a study funded by the National Institutes of Health and the Canadian Institutes of Health Research, researchers from the Columbia University Mailman School of Public Health and the University of British Columbia examined the relationship between injecting methamphetamine and suicidal behavior.
Their results, published in the December 1 Drug and Alcohol Dependence, indicate that injection drug users (IDUs) who inject methamphetamine should be monitored closely for signs of suicidal behavior.
The study was conducted in Vancouver, British Columbia, as part of an ongoing research project associated with the Urban Health Research Initiative (UHRI), a program based on a network of studies developed to help identify and understand the many factors that affect the health of urban populations, with a focus on substance use, infectious diseases, the urban environment, and homelessness.
The bulk of UHRI’s work is done in Vancouver, described as the “epicenter of a longstanding illicit drug use epidemic.” According to UHRI, Vancouver experienced in 1997 an explosive outbreak of HIV infection that remains one of the fast est spreading HIV epidemics documented in the developed world, and overdose fatalities and drug-related gun violence are highly prevalent.
Their study subjects were participants in the Vancouver Injection Drug Users Study, which began in 1996. They were recruited through word of mouth, street outreach, and referrals. At baseline and at each six-month visit thereafter, participants completed an interviewer-administered questionnaire that elicited information pertaining to sociodemographic characteristics, drug use, treatment utilization, and HIV risk behaviors.
During those visits, nurses also assessed participants for various health conditions, including suicidal behavior, and obtained blood specimens for HIV and hepatitis C serology. Participants received a small stipend for each visit.
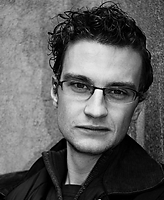
“This is one of North America’s largest cohorts of injection drug users,” Brandon Marshall, Ph.D., UHRI’s analytic coordinator, a postdoctoral fellow at the Columbia University Mailman School of Public Health and lead author of the report, told Psychiatric News. “Most of these users— about 5,000 of them—are concentrated in a very small neighborhood, making it an ‘ideal’ environment for this type of study. We were able to recruit about 1,700 of those 5,000. We have very good rapport in the community, and our study is one of the main points of access to health care for this population, so this is a very well utilized study with a high rate of follow-up.”
In a seven-year study that ended in May 2008, the researchers evaluated 1,873 participants. The median age of the sample was 31; 36.2 percent were female, and 601 (32.1 percent) were of Aboriginal ancestry. In total, 149 (8.0 percent) of the group reported a suicide attempt. The primary outcome for this part of their analysis was time to first report of suicidal behavior, and the primary exposure of interest was self-reported methamphetamine injection at least once in the prior six months.
“In this seven-year study, we found that IDUs who injected methamphetamine had an 80 percent greater risk of attempting suicide than those who did not, even after taking into account a wide range of potential confounders,” wrote Marshall and colleagues. They also investigated whether a dose-response relationship existed between the frequency of methamphetamine injection and increased likelihood of suicidal behavior, and discovered it did—compared with a period of no methamphetamine injection, infrequent methamphetamine injection was a predictor of attempting suicide, while frequent methamphetamine injection was associated with the greatest risk of attempting suicide.
“Although the etiologic pathway between injecting methamphetamine and suicidal behavior requires further investigation, it is likely that a combination of neurobiological, social, and structural mechanisms account for this association,” suggested Marshall and colleagues.
“Compared to other IDUs, it is possible that methamphetamine users have more isolated social networks and thus poorer social support systems. . . . Future studies that combine neurobiologic analyses with social epidemiologic approaches may provide greater insight into these potential mechanisms.”
The researchers said that although a variety of techniques was undertaken to ensure that the sample used was representative, caution is recommended when generalizing these findings to other settings.
An abstract of “Injection Methamphetamine Use is Associated With an Increased Risk of Attempted Suicide: A Prospective Cohort Study” is posted at <www.ncbi.nlm.nih.gov/pubmed/21676557>.