A common side effect of second-generation antipsychotic medications is weight gain. Yet up to now, there has been no way to predict which patients might be most vulnerable to weight gain induced by these drugs.
That situation may now be changing, thanks to a new finding reported online May 7 in the Archives of General Psychiatry. A gene variant located near a gene on chromosome 18 that makes the melanocortin 4 receptor seems to play a prominent role in antipsychotic-medication-induced weight gain.
The lead investigator was Anil Malhotra, M.D., a professor of psychiatry at Hofstra North Shore-LIJ School of Medicine in New York.
Malhotra and his colleagues first focused on a cohort of 139 youth aged 4 to 19 who were undergoing their first exposure to the second-generation anti-psychotic medications aripiprazole, olanzapine, quetiapine, or risperidone. The researchers tracked the youth for 12 weeks after they had started the medications to see how much weight they gained. They found that those taking aripiprazole, quetiapine, or risperidone gained comparable amounts of weight, and that those taking olanzapine gained even more.
To make their study sample more homogeneous, the researchers then genotyped the youth who had taken aripiprazole, quetiapine, or risperidone, but not olanzapine—a total of 94 subjects. Finally they looked to see whether they could link any gene variants with weight gain, while taking possible confounders, such as gender, race, initial body mass index, or type of antipsychotic used into consideration.
The researchers were able to link 20 gene variants with weight gain, and all of them were located close to a gene on chromosome 18 that makes the melanocortin 4 receptor. Mutations in this gene have been linked by other researchers to extreme obesity in the general population.
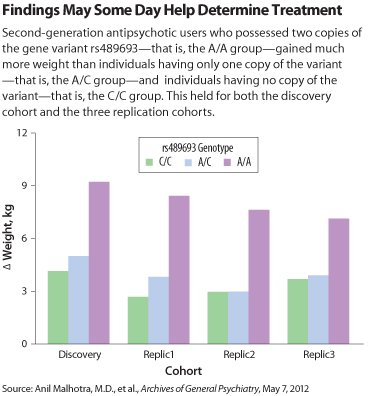
The researchers then tested a handful of these gene variants in three additional samples of subjects taking antipsychotic medications—altogether 205 subjects. The researchers found that one of the variants—called rs489693—was significantly linked to weight gain in each of the samples, even when gender, race, initial body mass index, and the particular antipsychotic used were considered.
It thus appears that this gene variant and the melanocortin 4 receptor are implicated in weight gain induced by antipsychotics, Malhotra and his team concluded.
And if so, the finding may eventually have clinical implications, Malhotra told Psychiatric News.
For example, there are currently no clinical tests for gene variants such as rs489693. But they might eventually become available. And if so, “it could be possible to identify those patients at greatest risk for severe weight gain prior to treatment initiation,” he explained. And if a patient was found to be at heightened risk for severe weight gain, then “perhaps alternative treatment strategies including nonantipsychotic drug treatment or additional psychosocial and/or behavioral interventions could be considered for these high-risk individuals.”
And if the melanocortin 4 receptor does play a critical role in mediating antipsychotic-induced weight gain, then “it seems logical that agents that directly, or perhaps indirectly, interact with the receptor might influence the weight gain associated with treatment,” he said. “Unfortunately, to date, we have not identified a compound that is safe to test in this manner.”
The study was funded by the National Institutes of Health and the Brain and Behavior Research Foundation (formerly NARSAD).