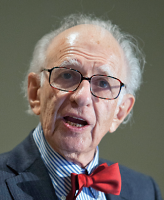
Molecular biology has made enormous strides in neurology but only modest ones in psychiatry, Nobel Prize–winner Eric Kandel, M.D., said at APA’s annual meeting in Philadelphia in May (For more on Kandel see Psychiatry, Neurology Need Closer Relationship).
Molecular research has been limited by lack of knowledge about the neuroanatomical basis of most psychiatric illnesses and the specific genes involved in those disorders, he said. Furthermore, mental illnesses are quite complex and involve many genes.
“Every gene works in the context of all other genes,” said Kandel, a professor at Columbia University, director of the Kavli Institute for Brain Science, and a senior investigator at the Howard Hughes Medical Institute. “Those genes may exert some compensatory effects and explain why some people with a predisposition for, say, schizophrenia do or do not become ill.”
However, recent advances have led to the development of sophisticated mouse models to study schizophrenia, he noted. “We can now do studies in mice comparable to those in people and studies in people comparable to those in mice,” he said.
Positive symptoms (such as disorganized thought, hallucinations, or delusions) are still difficult to recreate in mice. However negative symptoms (such as social withdrawal, blunted affect, or decreased motivation) and cognitive deficits can be studied in rodents.
“We know that antipsychotic drugs antagonize D2 receptors and that there is excessive dopaminergic transmission in the striatum in patients with schizophrenia, as a result of either increased dopamine synthesis, release, or receptor expression,” he said.
So Eleanor Simpson and Christoph Kellendonk in his lab developed a mouse that overexpressed the D2 receptor only in the striatum and also expressed a regulatory gene that could be used to turn the receptor gene on or off.
For one cognitive test, Kandel’s colleagues sent the animals down a T-maze. When they reached the head of the T, they had to turn in the opposite direction from the one in which they previously found food. Normal mice could make the right decision. Mice with lesions in their pre-frontal cortices had trouble doing so, as did mice with the D2 gene turned off. When the D2 gene was turned on, however, the animals continued to have cognitive defects. This is because compensatory changes carrying the behavioral abnormality forward took place in the brain.
“The defect is present at birth, and the striatal D2 receptor overexpression during prenatal development is enough to cause persistent cognitive deficits in adulthood,” explained Kandel. “This demonstrates why blocking D2 receptor expression later in life has no effect on cognitive symptoms. It also shows that schizophrenia is a developmental disorder and that the striatum has a more important role in cognition than previously thought.”
In collaboration with Peter Balsam, Ryan Ward, and Simpson, Kandel next modeled negative symptoms in mice, including a test of motivation, which is often deficient in patients with schizophrenia.
“These characteristics are similar in people and in mice, so it’s important to do parallel experiments in both,” he said.
In one test of motivation, the animals had to press a lever an increasing number of times to get food—once, twice, four times, eight times, etc. Eventually, like people, they give up, Kandel noted.
Mice overexpressing the D2 receptor are less willing to work for food, mimicking behavior in humans with schizophrenia.
Finally, in humans with schizophrenia, a third component of motivation—the pleasurable qualities of an outcome—remains normal. Such was also the case with the mice that were over-expressing D2. Their hedonic reactions remained intact.
Kandel and his colleagues then went on to use gene-chip analysis to study 23,000 transcripts from the striatum to see which genes were turned on when D2 receptors were overexpressed and turned off when expression was restricted. They found that increased D2 receptor expression produced increased 5-HT2C receptor expression. Blocking that receptor rescued motivation.
In mice, at least, both cognitive and negative symptoms seem induced by excess striatal D2 receptor activation, suggesting a “common molecular etiology,” he explained.
Transgenic mouse models may be just one impetus pushing psychiatry toward a needed paradigm shift, one that integrates psychiatry, neurobiology, and cognitive psychology, said Kandel.
“Few significant advances have been made in several decades,” he pointed out. “We need to encourage this kind of interaction between studies in mice and studies in patients to make headway in understanding the components of schizophrenia for which we do not have treatments.”

Psychiatry, Neurology Need Closer Relationship
Eric Kandel, M.D., headed toward psychiatry because of an early fascination with psychoanalysis. But in his senior year of medical school, he decided that a psychoanalyst should know something about the brain, so for a six-month elective period, he joined a neuroscience laboratory.
It was a fateful decision. Kandel subsequently spent most of his long career studying the molecular basis of memory using the sea snail Aplysia as his model. He won the Nobel Prize for that work in 2000, and in recent years returned to his original interest in mental illness.
Kandel wasn’t the only one who in his youth was impressed by Freud.
“Psychoanalysis caught the imagination of many people in my generation in the 1950s and 1960s, but that faith was diluted by the advent of psychotropic medications,” he said. “The intellectual value of psychoanalysis was challenged, and that carried with it a downplaying of psychotherapy as well.”
That was a loss, he said.
“Until recently, up to DSM-III or –IV, psychiatrists still distinguished between organic and functional mental illnesses,” he said. “Functional illnesses were those without evidence of brain damage. Now we realize that the mind is a set of functions carried out by the brain, that every [psychiatric] disorder is a brain disorder, and that psychotherapy is a brain treatment.”
What is needed, however, are more rigorous trials evaluating the specific value of different forms of psychotherapies and illuminating how they work.
Kandel also argued for greater interaction between neurology and psychiatry, the two medical specialties concerned with the brain.
“Our field has evolved in sophistication with regard to biology,” he said. “Psychiatry calls for a different sort of character than neurology, but we still need a hands-on, anatomical sense that neurology could provide. We should begin with a joint residency of neurology and psychiatry together by having the two fields share the same experiences for a year or two.”