About 1 in 5 U.S. adults suffered from a mental illness, not including a substance use disorder, in 2009, according to a report from the Substance Abuse and Mental Health Services Administration (SAMHSA). However, substance abuse and dependence frequently coexisted in people with other mental illnesses, the report pointed out.
Every two years, SAMHSA compiles the latest available national mental health statistics from various data sources, including national surveys, into one report. The latest edition, “Mental Health, United States, 2010,” was released April 25 and includes epidemiological as well as health care service data on mental illness.
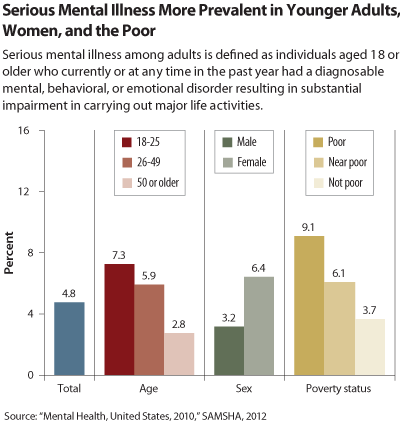
About 1 in 20 American adults aged 18 or older (4.8 percent) had a mental illness severe enough to impair major life activities in 2009. Among these people, about 40 percent received no treatment for their mental illness. The prevalence of serious mental illness in adults decreased with age, was twice as high in women as in men, and was clearly associated with poverty (see graph).
For purposes of the SAMHSA study, the prevalence of serious mental illness was considered a subset of any mental illness, which was defined as having a diagnosable mental, behavioral, or emotional disorder with mild to serious functional impairment. Substance use disorders frequently coexisted with other types of psychiatric disorders. In adults with serious mental illness in 2009, 1 in 4 met criteria for co-occurring substance dependence or abuse. This rate (25.7 percent) was four times the rate (6.5 percent) of substance dependence or abuse in the population with no mental illness (excluding substance use disorders).
Alcohol dependence or abuse was present in 1 of 5 adults with serious mental illness and was more common than illicit drug dependence or abuse. These data suggest that it is imperative to screen for and treat addiction in patients with other psychiatric disorders.
SAMHSA’s report examined mental illness statistics in certain special populations. For example, 2008 data showed that over 10 percent of active-duty military personnel reported posttraumatic stress disorder (PTSD) symptoms in the previous 30 days serious enough that they were deemed to need further evaluation. In addition, 21 percent of military personnel reported that in the seven days prior to being surveyed, they had depression symptoms serious enough that reviewers said they warranted follow-up evaluations. The data were derived from self-administered questionnaires given to military personnel. The percentages refer to personnel who self-reported enough symptoms (PTSD or depressive) that the military deemed them to be in need of further evaluation.
The report also highlighted the high prevalence of mental illness among the incarcerated population identified in surveys conducted at local jails in 2002 and state and federal prisons in 2004. With use of a modified Structured Clinical Interview for DSM-IV, symptoms of mental health problems or recent history of mental illness diagnoses were present in 64 percent of local jail inmates, 56 percent of state prison inmates, and 45 percent of federal prison inmates.
SAMHSA’s “Mental Health, United States, 2010” survey is the only national-level compilation of mental health data from both the private and public sectors, H. Westley Clark, M.D., J.D., M.P.H., director of SAMHSA’s Center for Substance Abuse Treatment, told
Psychiatric News. “It is an important reference for academics, policymakers, and students,” Clark said. The report goes beyond epidemiology, he noted, to summarize overall mental health services and costs in the United States. The effort is born out of SAMHSA’s recognition of the overlap between substance abuse issues and other areas of mental health as well as of mental health as a key component of overall health.