Methods
This study was conducted in Bali between June 2001 and July 2002. Bali is one of more than 10,000 islands that make up Indonesia and is famous for its unique Hindu-based culture. In 2001 there were 3,048,317 people living in Bali, and the island is almost entirely ethnically and culturally homogeneous. Industry is now in the developing stages. The basic unit of society is a community referred to as banjar, which consists of several hundred households. Bali has 260 psychiatric beds, and hospitals provide either psychiatric medication or psychotherapy based on Western medicine.
Details about the door-to-door survey to detect individuals with schizophrenia in the community have been described elsewhere (
2 ). In brief, at the first stage, nine banjars consisting of 1,966 households with 8,546 general residents were randomly and consecutively selected. Bali has one urban center in the capital city of Denpasar, but all the communities selected for this study were located in rural areas, the predominant type of area in Bali. Then, the first author (TK), a psychiatrist who speaks Indonesian and Japanese, conducted a face-to-face interview with one family member as a key informant for each of the 1,966 households to obtain information on whether a member of the family had schizophrenia. Male heads of the household were chosen as key informants, and if they were not at home, either their wives or siblings were selected as key informants.
Family History-Research Diagnostic Criteria (
3 ) was used to detect possible cases that fulfilled the criteria of either schizophrenia or schizophreniform disorder classified in the
DSM-III-R. For suspected cases, the first author conducted a direct interview by using the nonpatient version of the Structured Clinical Interview for DSM-III-R (SCID) (
4 ) to examine whether the cases fulfilled the
DSM-III-R criteria of schizophrenia or schizophreniform disorder. We employed
DSM-III-R, which was still frequently used in Bali at the time of investigation. In total, 39 individuals with schizophrenia were detected, including three whose initial diagnosis was schizophreniform disorder but who were rediagnosed as having schizophrenia six months after their onset of illness. Of the 39 people with schizophrenia, two pairs of brothers and one uncle-niece pair in the same household were included; thus the number of households was 36. During this diagnostic procedure, the first author was blind to the individual's past history of psychiatric medical treatment. The reliability of the diagnosis of schizophrenia by the first author has been established (
5 ).
The first author then interviewed the 39 individuals with schizophrenia and their families to assess the clinical conditions of the individuals and to identify the key relatives for the purpose of examining causal beliefs about schizophrenia. Clinical symptoms were evaluated by using the Positive and Negative Syndrome Scale (PANSS) (
6 ). The validity and reliability of the Indonesian version of this scale have been established (
7 ). Eguma's Social Adjustment Scale (ESAS) (
8 ) was used for the assessment of social adjustment. The ESAS has five categories to which we assigned scores: 1, self-supportive; 2, semi-self-supportive; 3, socially adjusted to family or community; 4, maladjusted; and 5, hospitalized.
The reliability of the clinical interview carried out in Bali by the first author has been established (
5 ). One key relative who was primarily responsible for decision making regarding the help-seeking behavior of each individual with schizophrenia was identified. Although three pairs of individuals with schizophrenia in the same household were included, the key relative for each member of the pair was a different person because of the extended family system, in which many relatives who live in the same compound are involved in the individual's care. After these interviews, the first author asked each individual with schizophrenia and his or her family detailed questions regarding the individual's history of psychiatric medical treatment and corroborated the data with medical records. In this study, treatment was defined as treatment with an antipsychotic; thus treatment by native healers who use traditional herbal medicine (
9 ) was not taken into account when we categorized participants as either treated individuals or never-treated individuals.
A self-report questionnaire examining families' causal beliefs about schizophrenia was developed for this research. We listed 15 possible causes (either natural or supernatural) of schizophrenia based on the in-depth interviews with 62 relatives of patients with schizophrenia in Bali in our previous research on expressed emotion (
10 ). Natural causes consisted of 11 items that conform with the ordinary course of nature (brain disorder, fatigue, financial problems, heredity, personality problems, physical disease, family relationship stress, nonfamily relationship stress, school stress, work stress, and poor upbringing). In contrast, supernatural causes consisted of four items related to an order of existence beyond the observable universe (disturbance by spirits, god's will or fate, karma, and witchcraft).
After discussing the causes of the illness in an open-ended manner to focus their ideas, the key relatives were asked to what extent each of these 15 items relates to the development of the illness. Each item was rated by using a 3-point scale (1, cause; 2, undecided as a cause; and 3, not a cause). Key relatives were also asked, which item was the most important cause of illness among the items they chose. These questions were designed to assess the causal attribution of the respondents at the time of the investigation. Moreover, additional questions were asked of the key relatives whose family members received psychiatric medical treatment at some point after their onset of illness. They were asked to indicate when they began thinking it was the most important cause—that is, whether it was perceived as being the most important cause before the patient's initiation of medical treatment or after.
This self-report questionnaire was constructed on the basis of the Causal Models Questionnaire of Schizophrenia in China (
1 ) and the 5-point Likert scales for examining relatives' beliefs about the causes of schizophrenia in Germany (
11 ); however, details such as the listed causes and the method of rating were originally developed in line with Balinese culture. Before the study presented here began, a pilot study was conducted for 62 relatives in our previous research on expressed emotion (
10 ) to examine the test-retest reliability of this questionnaire. The relatives were asked to respond to the questionnaire twice within a seven-day period. The Cohen's kappa coefficient was between .71 and .92, with a mean value of .82 for 15 items and .90 for the most important cause, indicating that the test-retest reliability was satisfactory.
We evaluated the relationship between the most important cause identified by the key relatives and the treatment status of the individuals with schizophrenia, sociodemographic data and clinical condition of the individuals with schizophrenia, and sociodemographic data of the key relatives.
The study was approved by the Indonesian Institute of Science, and all participants gave written informed consent to participate in the study.
Results
Of the 39 individuals with schizophrenia, 25 were males and 14 were females. They had a mean age of 38.7±14.46 years, a mean age at onset of 24.1±7.49 years, a mean total score on the PANSS of 78.87±25.43, and a mean ESAS score of 2.51± 1.21. (Possible PANSS scores range from 30 to 210, with higher scores indicating more severe psychiatric symptoms. Possible ESAS scores range from 1 to 5, with higher scores indicating worse social adjustment.) Nineteen (49 percent) had received psychiatric medical treatment at some point after their onset of illness, whereas 20 (51 percent) had not undergone any psychiatric treatment. Among the 19 treated individuals, two (11 percent) had been on medication regularly, whereas the remaining 17 (89 percent) had been on medication irregularly or briefly over the course of their illness. However, all individuals with schizophrenia had undergone traditional healing. All 19 individuals who received psychiatric medical treatment received traditional healing at least once before the initiation of psychiatric medical treatment.
Of 39 key relatives, 32 were male and seven were female. They had a mean age of 45.6±14.7 years and a mean of 4.7±4.3 years of education. The key relatives included 12 fathers, five elder brothers, five younger brothers, three wives, three sons, and 11 other family members.
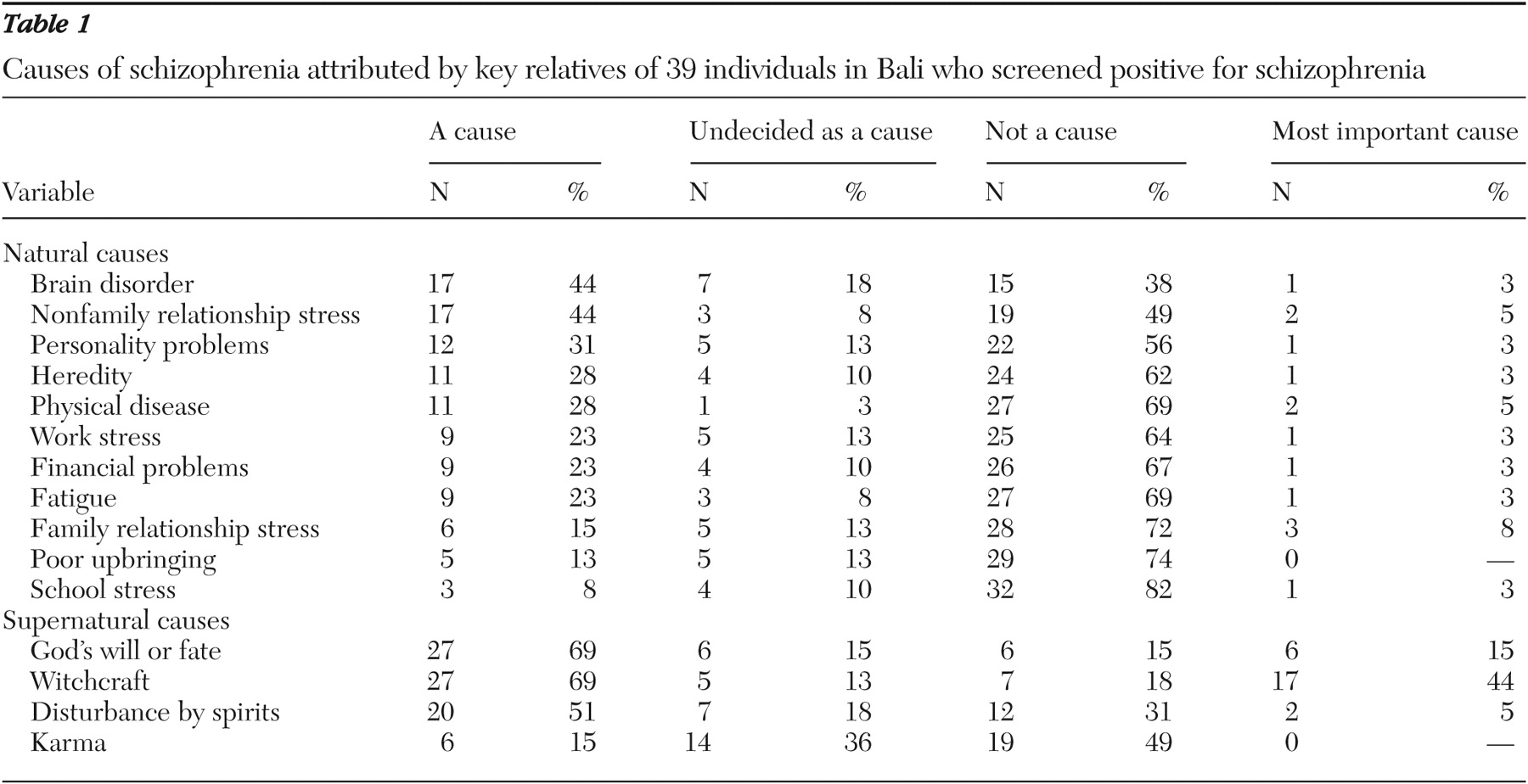
Key relatives identified a mean of 4.9 possible causes (range of two through nine). As shown in
Table 1, the most frequently cited causes were god's will or fate (69 percent) and witchcraft (69 percent), followed by disturbance by spirits (51 percent). Thus the three most commonly identified causes were supernatural. More than half the relatives identified these factors as a cause of the illness. Among natural causes, brain disorder (44 percent) and nonfamily relationship stress (44 percent) were most frequently cited.
Causes identified as being most important were witchcraft (44 percent), followed by god's will or fate (15 percent) and family relationship stress (8 percent). Again, the two causes most commonly identified as most important were supernatural. In total, 25 relatives (64 percent) identified a supernatural cause as being the most important in the development of schizophrenia, whereas 14 relatives (36 percent) thought a natural cause was the most important.
All 19 of the key relatives who had family members who received psychiatric medical treatment reported that, of the causes they selected as being most important at the time of the interview, they had recognized these as being the most important since before the patient's medical treatment was initiated.
As shown in
Table 2, compared with the 14 relatives who chose a natural cause as being the most important, the 25 relatives who chose a supernatural cause as being the most important had a significantly higher mean age (p<.01, two-tailed t test) and less education (p<.001, two-tailed t test). Of the 25 relatives who chose a supernatural cause as being the most important, 17 had family members who had never received psychiatric medical treatment and eight had family members who received such treatment. However, of the 14 relatives who chose a natural cause as most important, three had family members who had never received psychiatric medical treatment and 11 had family members who received such treatment. Thus, compared with relatives who chose a natural cause as the most important, relatives who chose a supernatural cause as the most important were more likely to have family members who had never received psychiatric medical treatment (17 of 25 relatives, or 68 percent, compared with three of 14 relatives, or 21 percent) (
χ 2 =7.79, df=1, p<.01). No significant difference was observed in other clinical data for the individuals with schizophrenia (age at onset, duration of illness, PANSS scores, ESAS scores) between the two family groups.
Discussion
Families' causal attributions regarding schizophrenia may be strongly influenced either by their cultural and social backgrounds or by the state of mental health care in their community. According to the Balinese traditional belief system, mental disorders are considered "nonmedical diseases" that are caused by an invisible and abstract element (
9 ). Although trance and possession disorders are usually recognized as a direct result of possession by spirits or gods, psychotic disorders such as schizophrenia are often described with vague wording, such as "disorders caused by outside supernatural factors." In the study presented here, families of individuals with schizophrenia tended to attribute the cause of the illness more to supernatural factors than to natural factors. Thus this study indicates that, even now, Balinese still have a firm traditional belief that mental disorders are "nonmedical diseases," especially Balinese who are older and have less education.
This study demonstrated that the families' supernatural causal attributions regarding schizophrenia were strongly associated with nonreceipt of psychiatric medical treatment by individuals with schizophrenia. To our knowledge, this is the first community-based study investigating the relationship between families' causal beliefs and the psychiatric treatment status of individuals with schizophrenia. The clinical condition of the individuals with schizophrenia in this study who never received psychiatric medical treatment was poor; thus therapeutic intervention for these individuals is needed (
2 ). Providing knowledge about schizophrenia to family members is one of the key factors of an intervention strategy aimed at reducing the number of individuals with schizophrenia in Bali who have never received psychiatric medical treatment. As Jorm (
12 ) noted, although the benefits of public knowledge of physical diseases are widely accepted, knowledge about mental disorders (mental health literacy) has been comparatively neglected. If the public's mental health literacy is not improved, public acceptance of evidence-based mental health care may be hindered (
12 ).
In addition to the negative impact a lack of mental health literacy has on the treatment of individuals with schizophrenia, we should also note several positive aspects regarding supernatural causal attributions in Bali. The most frequently cited causes by the relatives in this study were god's will or fate and witchcraft. Furthermore, relatives rated witchcraft as the most important cause, followed by god's will or fate. These causal attributions are not personal and go beyond the patients' sphere of responsibility. Researchers have shown that relatives with high levels of expressed emotion, which is a significant and robust predictor of relapse in schizophrenia, were found to view the illness and associated symptoms as residing more within the patient's control as compared with relatives with low levels of expressed emotion (
13 ). Thus a supernatural causal belief about schizophrenia among Balinese might contribute to the low prevalence of relatives in Bali who have high levels of expressed emotion (
10 ). Moreover, a supernatural causal attribution, which does not assign responsibility for the disorder to the family, may decrease the families' psychological burden.
This study has several limitations. First, the small number of participants made it difficult to interpret the results. Second, participants for the purpose of examining causal beliefs about schizophrenia were limited to the families of persons with schizophrenia, and either the general residents or persons with schizophrenia themselves were not included. Future studies should overcome these limitations and should identify comprehensive Balinese causal beliefs about schizophrenia.