There is growing momentum and pressure to move evidence-based mental health interventions into real-world practice settings (
1,
2,
3,
4,
5 ). Most of these practice settings involve a relationship between a clinical or case management supervisor and practitioners who provide services. Often in community settings the clinical supervisor also supervises work activities, including conducting performance appraisals and other human resource functions. Leadership is important in these activities. Recent work has also demonstrated that mental health service providers' attitudes toward adopting evidence-based practice are associated with organizational context (for example, structure and policies) and individual provider differences (for example, education and experience) (
6,
7 ). Yet, although leadership is held to influence the adoption of innovations, such as evidence-based practices (
8 ), there has been little research on the association between leadership of the mental health supervisor and staff attitudes toward adopting evidence-based practice. However, some more general leadership studies have been conducted.
Leadership research is pervasive in the organizational literature, and studies in mental health services suggest that leadership is important for both for the organizational process and for consumer satisfaction and outcomes (
9,
10,
11 ). Glisson and Durick (
11 ) found that higher levels of positive leadership in human service organizations were associated with higher levels of organizational commitment. In a study on mental health services for youths, organizational climate mediated the association of leadership and working alliance (
12 ). Higher levels of positive leadership were associated with a more positive organizational climate, which was in turn associated with higher positive clinician ratings of working alliance. Thus there are links between leadership, organizational and clinical process, and consumer satisfaction and outcome. However, research is needed that examines the effect of leadership on attitudes toward adopting evidence-based practices in mental health service settings.
Transformational and transactional leadership are two well-studied leadership styles that have been assessed by the Multifactor Leadership Questionnaire (MLQ) (
9,
13,
14 ). Transformational and transactional leadership span both cultural and organizational boundaries (
15 ) and have been assessed and validated in numerous studies (
16,
17,
18,
19,
20,
21,
22,
23,
24,
25,
26 ). Leadership studies with the MLQ have also been conducted in mental health and other public-sector organizations (
9,
14,
27,
28,
29 ), health care settings (
30 ), and service settings. A given leader may exhibit varying degrees of both transformational and transactional leadership. The styles are not mutually exclusive, and some combination of both may enhance effective leadership.
Transformational leadership is akin to charismatic or visionary leadership (
31 ). Transformational leaders inspire and motivate followers (
32,
33 ) in ways that go beyond exchanges and rewards. Transformational leadership operates especially well in close supervisory relationships, compared with more distant relationships (
23 ), and closer supervision is often more typical in mental health settings. This close relationship may be typical of a supervisor-supervisee relationship and is also captured in the notion of "first-level leaders" (
34 ), who are thought to be important because of their functional proximity to supervisees in an organizational setting. Transformational leadership is thought to increase the follower's intrinsic motivation (
35 ) through the expression of the value and importance of the leader's goals (
31,
36 ).
In contrast, transactional leadership is based more on "exchanges" between the leader and follower, in which followers are rewarded for meeting specific goals or performance criteria (
37,
38,
39,
40 ). Rewards and positive reinforcement are provided or mediated by the leader. Thus transactional leadership is more practical in nature because of its emphasis on meeting specific targets or objectives (
41,
42,
43 ). An effective transactional leader is able to recognize and reward followers' accomplishments in a timely way. However, subordinates of transactional leaders are not necessarily expected to think innovatively and may be monitored on the basis of predetermined criteria. Poor transactional leaders may be less likely to anticipate problems and to intervene before problems come to the fore, whereas more effective transactional leaders take appropriate action in a timely manner (
39 ).
A transactional leadership style is appropriate in many settings and may support adherence to practice standards but not necessarily openness to innovation. A transformational leadership style creates a vision and inspires subordinates to strive beyond required expectations, whereas transactional leadership focuses more on extrinsic motivation for the performance of job tasks (
39,
40,
44 ). Thus it is likely that transformational leadership would influence attitudes by inspiring acceptance of innovation through the development of enthusiasm, trust, and openness, whereas transactional leadership would lead to acceptance of innovation through reinforcement and reward.
In summary, leadership is important to consider in relation to acceptance of innovations and to work attitudes, perceptions, behavior, service quality, and client outcomes. Because leadership is associated with organizational and staff performance, we propose that it is likely to influence mental health providers' attitudes toward adoption of evidence-based practices. Although leadership is prominent in our model of implementation of evidence-based practices (
7 ), few studies have examined transformational and transactional leadership and mental health providers' attitudes. Finally, no studies have examined leadership and attitudes toward adopting evidence-based practices in mental health services for youths.
In understanding organizational predictors of attitudes toward evidence-based practices, it is also important to consider and control for individual-level variables, such as providers' demographic characteristics. A recent review suggests that demographic characteristics and attitudes can be influential in the willingness to adopt and implement an innovation (
45 ). For example, receptivity to change can be an important determinant of innovation success (
46,
47 ). Rogers (
8 ) asserted that having more formal education, as well as favorable attitudes toward change and science, are associated with increased adoption of an innovation. Educational attainment is positively associated with endorsement of evidence-based treatment services, adoption of innovations, and attitudes toward adoption of evidence-based practices (
6,
48,
49,
50 ). In specialty mental health clinics, compared with professional providers, interns report having a more positive attitude toward using evidence-based assessment protocols (
51 ) and toward adopting evidence-based practices (
6 ). Because there is a link between organizational characteristics, individual differences, and attitudes toward work, these factors should be included in studies of attitudes toward evidence-based practice.
The purpose of the study presented here was to examine the association of transformational and transactional supervisor leadership with service providers' attitudes toward evidence-based practices. We hypothesized that more positive transformational leadership would be associated with more positive attitudes toward implementing evidence-based practices, as evidenced by greater openness, greater sense of appeal of evidence-based practices, and lower perceived divergence of usual practice with evidence-based practices. We also hypothesized that transactional leadership would be associated with more positive attitudes toward adopting evidence-based practice, given requirements to do so.
Methods
Participants
Participants were providers of mental health clinical and case management services who took part in a larger study of organizational issues affecting the provision of mental health services to children, adolescents, and their families in San Diego County, California (
6 ). Organizational and individual participation rates were high (94 and 96 percent, respectively). Data were collected between November 21, 2000, and September 19, 2001. Of the 322 providers in the larger study, 19 participants (5.9 percent) were missing data on at least one of the variables in the set of analyses used in this study, resulting in a final sample of 303 providers working in 49 publicly funded mental health programs for youths.
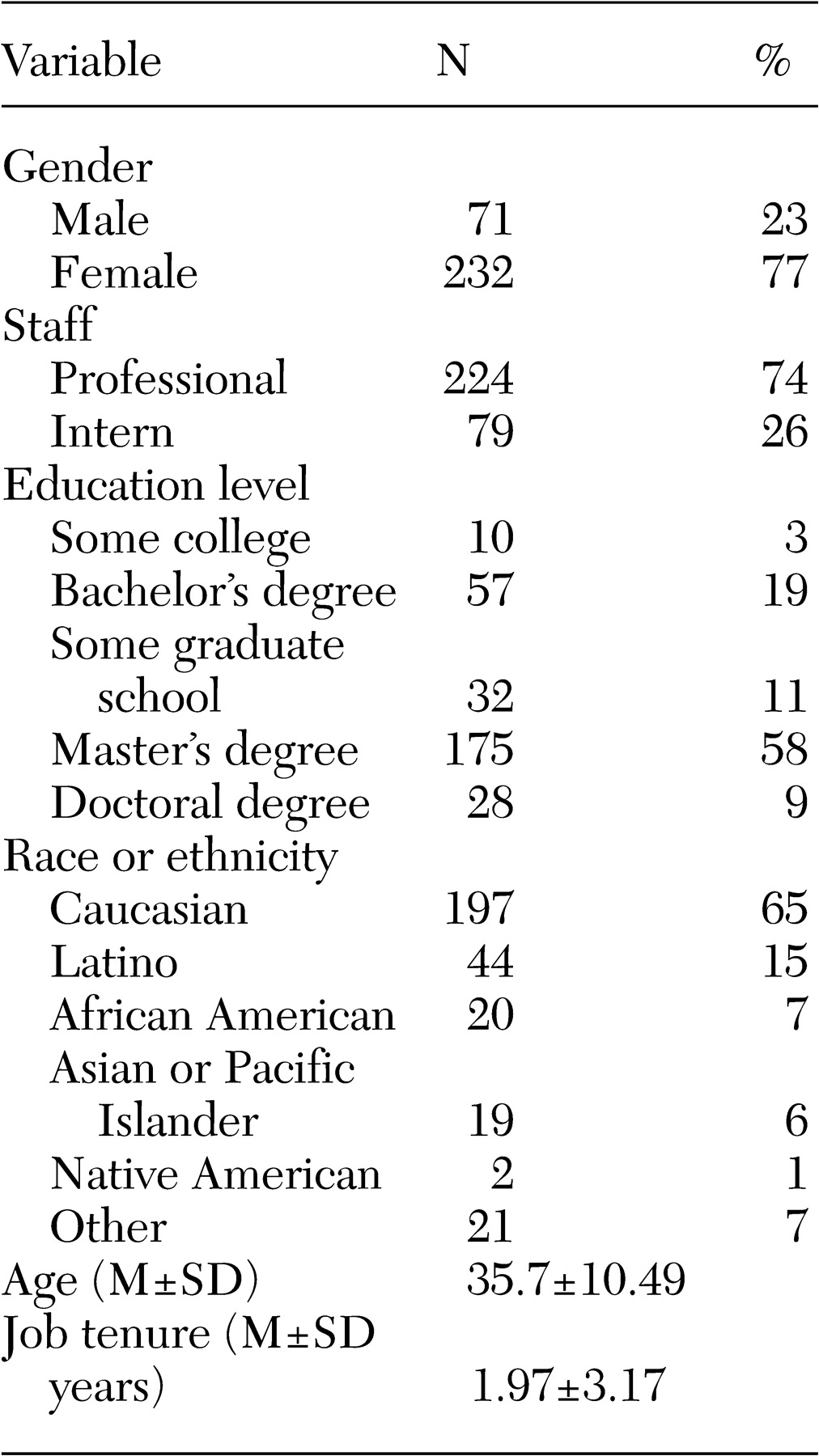
Table 1 shows demographic characteristics for individual-level nominal and continuous variables in the study. A total of 245 respondents (81 percent) were full-time employees. Primary disciplines included marriage and family therapy (103 participants, or 34 percent), social work (99 participants, or 33 percent), psychology (65 participants, or 21 percent), psychiatry (five participants, or 2 percent), and "other" (for example, criminology, drug rehabilitation, education, or public health; 31 participants, or 10 percent). There were fewer interns than professional staff in the service system (26 percent compared with 74 percent). The mean±SD age of respondents was 35.7±10.5 years. Seventy-six percent were female. Sixty-five percent were Caucasian, 15 percent were Hispanic, 7 percent were African American, 6 percent were Asian or Pacific Islander, 1 percent were Native American, and 7 percent were another race or ethnicity. (Percentages total more than 100 percent because of rounding.)
Measures
Provider survey. The provider survey incorporated questions about providers' demographic characteristics, including age, sex, education level, professional status (intern or professional), and job tenure (time working in the present employment setting) (
6 ). Providers' education level was assessed with ordered categories from low to high: attainment of some college, college graduate, some graduate work, master's degree, and doctoral degree (Ph.D., M.D., or equivalent). Intern status indicated whether the respondent was an intern or an employed professional. Professional status was coded as 0 for staff and as 1 for interns.
Attitudes toward evidence-based practice. The Evidence-Based Practice Attitude Scale (EBPAS) (
6 ) was used to assess mental health providers' attitudes toward evidence-based practice. The EBPAS is a brief, 15-item measure with four subscales assessing attitudes toward adoption of evidence-based practices. The four EBPAS subscales represent four theoretically derived dimensions of attitudes toward adoption of evidence-based practices: appeal, requirements, openness, and divergence. Total scores on the EBPAS were also calculated.
The score on the appeal subscale represents the extent to which the provider would adopt an evidence-based practice if it were intuitively appealing, could be used correctly, or was being used by colleagues who were happy with it. The score on the requirements subscale assesses the extent to which the provider would adopt an evidence-based practice if it was required by an agency, supervisor, or state. The score on the openness subscale assesses the extent to which the provider is generally open to trying new interventions and would be willing to try or use evidence-based practices. The score on the divergence subscale assesses the extent to which the provider perceives evidence-based practices as not clinically useful and less important than clinical experience. The total score on the EBPAS represents one's global attitude toward adoption of evidence-based practices. The overall Cronbach's alpha reliability for the EBPAS was good (
α =.77), and subscale alphas ranged from .90 to .59. The EBPAS validity is supported by associations of EBPAS scales with both individual provider-level attributes and organizational characteristics (
6,
48 ). All responses for the EBPAS were scored on a 5-point scale, ranging from 0, not at all, to 4, to a very great extent.
Leadership. The MLQ 45-item Form 5X was used to assess the providers' perceptions of supervisors' transformational and transactional leadership behaviors (
52 ). Transformational leadership was assessed with four subscales of idealized influence (eight items,
α =.87), inspirational motivation (four items,
α =.91), intellectual stimulation (four items,
α = .90), and individual consideration (four items,
α =.90). Transactional leadership was assessed with four subscales detailing leadership styles, including contingent reward (four items,
α =.87), laissez-faire (four items,
α =.83), active management by exception (four items,
α =.74), and passive management by exception (four items,
α =.82). Providers were asked to judge the extent to which their immediate supervisor engaged in specific behaviors measured by the MLQ. Each behavior was rated on a 5-point scale ranging from 0, not at all, to 4, to a very great extent.
Survey procedure
A program manager was contacted at each program, and the study was described to him or her in detail. Permission was sought to survey service providers who worked directly with youths and families. For participating programs, providers' survey sessions were scheduled at the program site at a time designated by the program manager. Surveys were administered to groups of providers. The project coordinator or a trained research assistant administered providers' surveys and was available during the survey session to answer any questions that arose. A few surveys were left for completion for providers who did not attend the survey sessions. Such surveys were either mailed back in a prepaid envelope or picked up by a research assistant. Participants received a verbal and written description of the study, and informed consent was obtained before the survey. Participation in the study was voluntary, and all participant responses were confidential. This study was approved by the appropriate institutional review boards.
Analyses
Pearson product-moment correlation analyses were first conducted to examine associations of transformational and transactional leadership and individual-level covariates with the dependent variables—that is, EBPAS scores representing attitudes toward evidence-based practices. Next, regression analyses were conducted in order to examine the associations of leadership with scores on each of the four EBPAS subscales and total scores on the scale while the analyses controlled for the effects of individual provider characteristics. Because providers were nested within mental health programs, resulting in potential dependency of responses within program, multilevel analyses were conducted to control for the effects of the nested data structure (
53,
54,
55 ). All regression analyses were conducted by using the Mplus analytic software, which accounted for the nested data structure (
56 ). Because hypotheses were directional, one-tailed significance tests were used.
Results
As shown in
Table 2, correlation analyses showed a pattern of results supporting the hypothesis that ratings of higher levels of positive leadership would be associated with more positive attitudes toward evidence-based practice. Specifically, transformational leadership was significantly positively associated with scores on the EBPAS subscales of appeal, openness, and requirements and EBPAS total scores. Transactional leadership was significantly positively associated with scores on the EBPAS subscales of openness and requirements and EBPAS total scores. Next, a regression analysis was performed for each EBPAS subscale and one for the overall scale.
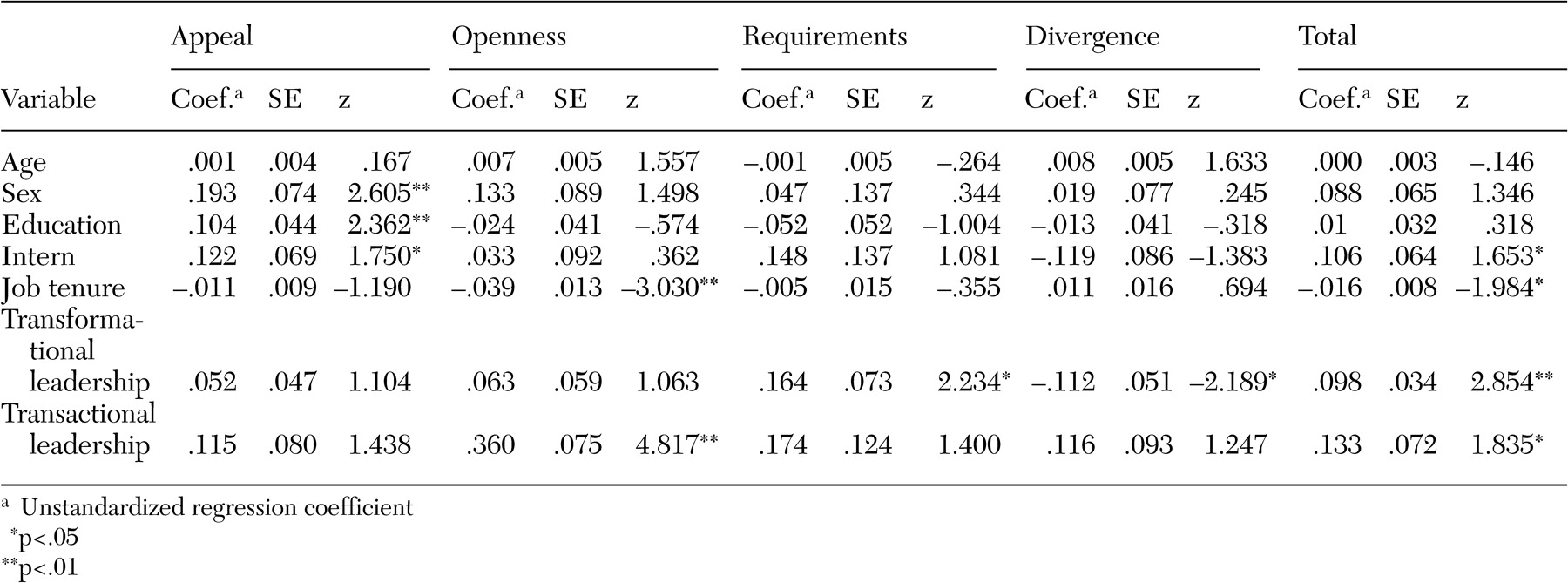
All regression analysis results are shown in
Table 3 . Neither a transformational nor a transactional leadership style was significantly associated with scores on the EBPAS appeal subscale. In regard to provider characteristics, higher scores on the appeal subscale were associated with being female, having a higher educational attainment, and being an intern. Predictors accounted for 7.4 percent of the variance in scores on the appeal subscale.
Transactional leadership was significantly positively associated with scores on the EBPAS openness subscale. This indicates that providers who reported that immediate supervisors exhibited more transactional leadership behaviors endorsed greater general openness toward adoption of evidence-based practices. Job tenure was significantly negatively associated with scores on the openness subscale, indicating that providers who worked at their program for longer periods scored lower on the openness subscale. Predictors accounted for 14.0 percent of the variance in scores on the openness subscale.
Transformational leadership was significantly positively associated with scores on the requirements subscale. This finding indicates that providers who worked with supervisors who they rated higher on transformational leadership were more willing to adopt evidence-based practices if required to do so. There was also a marginal effect (p=.081) suggesting that transactional leadership was associated higher scores on the requirements subscale. Predictors accounted for 7.7 percent of the variance in EBPAS total scores.
As hypothesized, transformational leadership was negatively associated with the scores on the EBPAS divergence subscale. This finding indicates that providers who worked with supervisors who exhibited more transformational leadership behaviors were less likely to perceive a gap between their current practices and evidence-based practices. Predictors accounted for 5.1 percent of the variance in scores on the divergence subscale.
Finally, both transformational and transactional leadership were positively associated with total scores on the EBPAS. This finding supports the proposed hypothesis and indicates that providers who rated their supervisor higher on transformational and transactional leadership were more open to adopting evidence-based practices. In regard to demographic variables, being an intern was positively associated and job tenure was negatively associated with more positive attitudes toward evidence-based practices. Predictors accounted for 13.4 percent of the variance in total scores on the EBPAS.
Discussion
The main finding of this study is that more positive leadership ratings were associated with more positive attitudes toward adopting evidence-based practice. This is congruent with the notion that leadership is important in the adoption of innovations across a range of organizational contexts and technologies (
8,
57,
58 ). However, across all EBPAS subscales and the total scale on the EBPAS, predictors accounted for about 5 to 14 percent of variance in subscale and total scores. This suggests that although leadership is associated with providers' attitudes toward evidence-based practices, additional factors should be considered. In the study presented here both transformational and transactional leadership were associated with attitudes toward adoption of evidence-based practices.
Transformational leadership was positively associated with scores on the requirement subscale and total scores on the EBPAS scale and negatively associated with scores on the divergence subscale. It is likely that supervisors who exhibit more positive transformational leadership behaviors engender attitudes in subordinates that would lead subordinates to greater openness to adopting new technologies or practices. This finding is clearly in keeping with the definition of transformational leadership as inspiring commitment to and enthusiasm for the leader and willingness to follow the leader's vision. Consistent with this definition is the finding that transformational leadership was associated with the total EBPAS score, indicating that inspirational and motivational leadership may engender open attitudes.
Also of interest is the finding that higher transformational leadership was associated with lower perceived divergence of evidence-based practices and usual practices. It is likely that this finding indicates a general distrust of change and practices that are perceived as different from usual care where leadership is suboptimal. These findings suggest that having a positively perceived local opinion leader to introduce and guide change in practice may facilitate receptivity to change in providers' behavior (
59 ). Consistent with the above findings, transactional leadership was positively associated with scores on both the openness subscale and the total EBPAS scale. This suggests that leadership styles that appropriately reinforce positive work behaviors may lead to a greater sense of trust in the supervisor-supervisee relationship and lead to greater openness toward adopting evidence-based practices.
Some limitations of this work should be noted. First, this study assessed providers' attitudes rather than actual uptake of evidence-based practices. There are a number of factors likely to influence not only attitudes toward evidence-based practices but also actual implementation. Indeed, a leader's attitude toward evidence-based practice may influence staff attitudes, and leaders' attitudes were not assessed in this study—instead, providers rated their perception of their supervisors' leadership behaviors. Second, this is a cohort study, and although it is intuitively appealing to suggest that supervisor leadership precedes staff attitudes, such an inference is not warranted on the basis of the correlational nature of this study.
Third, this study involved public-sector mental health providers, and results may not generalize to other contexts or provider groups. However, this concern is somewhat mitigated to the extent that the findings presented here are consistent with the literature on leadership and organizational change. Fourth, five regression models were estimated, and thus inflation of type I error rates could be a factor in this set of analyses. Fifth, providers' ratings of their supervisors' leadership was assessed in the study presented here. However, other organizational variables may also be related to providers' attitudes toward evidence-based practices (
48 ). Finally, the focus of leadership was not assessed. That is, it is unknown in the study presented here the degree to which supervisors promoted the use of evidence-based practices. This leaves us with findings regarding general, rather than specific, effects of transformational leadership.
Further studies are needed to examine the extent to which supervisors' transformational and transactional leadership that was focused specifically on improving attitudes and implementation of evidence-based practices would lead to greater, lesser, or different associations with providers' attitudes and ultimately, with evidence-based practice implementation fidelity and client outcomes.
One of the strengths of the study presented here is that it focused on real-world mental health service providers working in community-based, publicly funded mental health programs. In that respect, this work differs from studies of manualized interventions focusing on more traditional psychotherapy practices with doctoral-level clinicians (
60,
61 ). In the public behavioral health care system, a majority of providers in the workforce in community settings across the United States do not have doctoral-level educations, and these essential providers will likely be agents of widespread delivery of evidence-based interventions. Thus, although this study took place in one large county, the results are likely to generalize to other similar settings. Additional research is needed in order to determine if these findings can be replicated.
This study also adds to the evidence base for the construct validity of the EBPAS. Previous work provided preliminary validation of the EBPAS; our findings support the notion that attitudes may be affected not only by the context within which providers deliver mental health services but also by the leader-staff interactions and exchanges in the workplace that can affect job performance and organizational citizenship (
62,
63,
64 ). This suggests that leadership development targeted at improving the organizational change process could be considered before or concurrent with evidence-based practice implementation.
Providers in the study presented here were predominantly female, and a majority of public-sector providers of youth mental health services are female. Leadership and subordinate perceptions and relationships may be affected by the sex of the leader or follower. For example, gender affects leadership style, and effective leadership involves a balance of positive feminine and masculine characteristics (
65 ). Female leaders may also be rated higher on interpersonal aspects of transformational leadership (
66 ). It appears that in understanding leadership effects, gender of the leader and follower should be considered, but the extent to which these factors are at play in mental health services and evidence-based practice implementation requires further study.
As with providers in other types of services, those who provide youth and family services are often highly committed to their work and clients. Leadership is important in work interactions and in shaping organizational culture to support change and innovation (
67 ). Attitudes toward adopting evidence-based practice may be influenced to the extent that leaders are effective in communicating and getting support for a vision that includes the adoption and use of evidence-based practices. Transactional leadership may also help in rewarding and reinforcing behaviors that support the vision.
Working in the public sector brings special challenges for organizations implementing evidence-based practices. For example, the need for obtaining or renewing contracts and securing funding is an ongoing concern. At the local level, implementing evidence-based practices within an existing contract may mean renegotiating statements of work and defining what services can be reimbursed. National reimbursement policies may not be aligned with the provision of some evidence-based practices. These and other related concerns can lead to challenges for leaders in communicating how a vision of improved or changed services fits, or does not fit, with the day-to-day roles, duties, and tasks fulfilled by providers. Stronger leadership should help to mitigate some of the stresses of day-to-day operation of services and improve managers' ability to lead change.
Particular attention should be paid to the perceptions and attitudes of public-sector providers and their supervisors. There have been recent calls for renewed attention to workforce development (
68,
69 ). More effective leadership is one mechanism by which first-level leaders (
34 ), such as program managers, can work with their staff to improve the workplace and the ability of programs to respond to the need for change in perspective and process that accompanies implementation of evidence-based practices. It is these first-level leaders who generally have the responsibility for managing and monitoring change. Attention to the relationships between the managers and their staff in public-sector mental health programs will be necessary to address the challenges of workforce development and evidence-based practice implementation.
Conclusions
Although leadership functions may vary by organizational level or discipline (
70,
71 ), the study presented here suggests that the supervisor-supervisee dyad is a potentially important point of influence in affecting attitudes toward adopting evidence-based practice. However, in order to change attitudes and practice, leaders must persevere in the change process, and multiple hurdles to change should be expected and allowed for (
72,
73,
74,
75,
76 ).
Behavioral health services organizations often deal with change as a function of internal initiatives or in response to external demands. Leaders at different organizational levels often spearhead or manage such changes. Although this study deals with attitudes toward evidence-based practice, it also relates to organizational change in general. Organizational context, individual provider differences, and type and complexity of the evidence-based practice to be implemented must all be considered (
77 ). Leadership at the supervisor-supervisee level is important in management of change, as this is a frequent point of contact, influence, and shared meaning in organizations. Because of the complexity of organizations, providers, and clients, there is no single factor or correct approach for implementation of evidence-based practices in behavioral health service organizations. However, the study presented here provides some guidance in improving our understanding of how leadership may influence providers' attitudes. The link between attitudes and actual implementation of evidence-based practices has yet to be confirmed, however.
This study adds to the evidence that leadership is one factor that can affect the implementation of evidence-based practices in behavioral health services. This study provides additional evidence that multiple factors in the service context are important in understanding attitudes toward evidence-based practice (
4,
6,
7,
75,
78 ). Leadership geared toward promoting adoption of innovation and change is critical to the success of implementing evidence-based practices. Further work is needed to identify who will benefit from improved leadership skills, how best to train and apply leadership skills, and when in the process of evidence-based practice implementation to provide training and development for effective leadership.
Acknowledgments
This work was supported by grant MH-001695 from the National Institute of Mental Health. The author thanks the program managers, supervisors, clinicians, and case managers who participated in this study.