The public mental health system is an important safety net for persons affected by severe mental illness who have low incomes and are medically indigent. Latinos and Asians exhibit lower rates of psychiatric disorders than their non-Latino white and U.S.-born peers (
1,
2,
3,
4 ). Alegria and colleagues (
5 ) identified variations in lifetime and past-year prevalence rates of psychiatric disorders among Latino subgroups. After other factors were controlled for, Mexicans had significantly lower lifetime odds of depression and Cubans had lower odds of anxiety and substance use disorders than Puerto Ricans. In addition, both Mexicans and Cubans exhibited significantly lower lifetime and past-year odds of overall psychiatric disorders compared with Puerto Ricans.
Data from the National Latino and Asian American Survey show that lifetime and past-year prevalence of any psychological disorder did not differ by Asian subgroup (
6 ). However, multivariate analyses showed that Vietnamese women were half as likely as Chinese women to experience any depressive disorder during their lifetime, and Filipino men were more than twice as likely as Chinese men to experience any substance use disorder in their lifetime (
6 ).
Low utilization of mental health care among persons with mental illness from ethnic minority populations remains a critical public health issue (
7,
8,
9 ). Community-based surveys have shown that among persons who meet psychiatric diagnostic criteria, those from ethnic minority groups are less likely than white and U.S.-born adults to use mental health services (
8,
10 ). Lack of access to mental health services can result in adverse outcomes, including reduced quality of life, interference with social relationships, and negative impacts on labor market participation and productivity (
11 ).
Use of mental health services is shaped by diverse factors. Lack of health insurance, limited incomes, and lack of information about available services often lead to unfavorable patterns of health care use among ethnic minority populations (
12 ). Cultural factors, such as perceived origin of mental illness (
13 ), perceived helpfulness of mental health care (
14 ), or somatization and culture-bound syndromes (
15,
16 ), may also influence use of mental health services by Latinos and Asians, including immigrants from these groups. Furthermore, having limited English proficiency may reduce a person's ability to navigate mental health service systems and to establish new or maintain existing patient-provider relationships (
17,
18 ). In addition, limited English proficiency may compromise the quality of care received by foreign-born individuals, resulting in poor understanding of diagnosis or treatment, reduced adherence to treatment regimens, and poor reporting of medication side effects (
19,
20 ). However, few studies have examined the effect of limited English proficiency on use of mental health services by persons with mental illness from ethnic minority groups who are uninsured or publicly insured.
This study examined how Latino and Asian adults in San Diego County who had severe mental illness and limited English proficiency and who were indigent or publicly insured initially accessed the public mental health system and how their subsequent use of public mental health services changed over time compared with their English-proficient peers and non-Latino whites. The mental health services that were examined include outpatient, inpatient, and emergency services. We hypothesized that these Latino and Asian clients would be less likely than clients who were English proficient to access the system through outpatient mental health services and would be more likely to enter through inpatient or emergency services. We also sought to examine the effects of programs that serve large numbers of clients with limited English proficiency, because linguistically appropriate services maybe more available in such systems.
Methods
Data, sample, and independent variables
Data from the encounter-based management information system (MIS) of San Diego County Adult and Older Adult Mental Health Services (AOAMHS) were used to identify persons with severe mental illness who used public mental health services and lived in the community during fiscal years 2000–2005. Severe mental illness was defined as receiving one or more diagnoses of schizophrenia, bipolar disorder, or major depression. At admission to each service clients reported their living situation, and we classified clients by their most commonly reported living situation. We included persons living independently, those residing in assisted-living facilities (also known as board-and-care facilities), and those who were homeless. We excluded persons residing primarily in jails or long-term institutional care facilities.
Demographic information was obtained from the MIS, including age, gender, self-reported race or ethnicity, preferred service language, and Medi-Cal (California's Medicaid program) status. Additional clinical information from the MIS included diagnosis of a substance use disorder and Global Assessment of Functioning (GAF) scores (
21 ). We used a client's reported preference for service language as a proxy for limited English proficiency status. In California language preference is highly correlated with foreign-born status. Data from the California Health Interview Survey indicate that among Latino adults in San Diego in homes where Spanish is spoken, 73% were born in Mexico; among Asians in homes where Chinese or Vietnamese is spoken, 86% were born in Asia or the Pacific Islands (
22 ). The study sample is limited to Latinos with a preferred language of English or Spanish, Asians with a preferred language of English or an Asian language (for example, Chinese, Vietnamese, or Tagalog), and non-Latino whites with a preferred language of English.
San Diego County is a large, diverse county located on the U.S.-Mexico border. As a border region, it is home to large ethnic minority and foreign-born populations, particularly Latinos of Mexican origin. In addition, there is a large population of Asians in San Diego, most of whom are Filipino or Vietnamese. In 2006 San Diego County had a total population of approximately three million, 29% of whom were Latino, 10% were Asian, and 5% were African American (
23 ). The top three threshold languages (languages for which plans serving Medi-Cal beneficiaries are required to develop linguistically appropriate public health materials) are Spanish, Vietnamese, and Tagalog. The MIS database has been previously used to examine mental health service use by ethnicity and language among Latinos, as well as costs associated with nonadherence to antipsychotic medications and atypical antipsychotic polypharmacy (
24,
25,
26,
27,
28 ).
The University of California, San Diego, Institutional Review Board and the San Diego County Mental Health Services Research Committee approved the use of a limited data set for the purpose of this study in accordance with the privacy rule of the Health Insurance Portability and Accountability Act of 1996.
Dependent variables
In fiscal year 2005–2006 AOAMHS provided services to 38,581 adult and older adult clients, with a budget of $163 million, of which $94 million was allocated to nonprofit providers across 132 direct-service programs. The MIS provides detailed information about specialty mental health care encounters and service utilization. We examined use of three types of services: outpatient visits, including case management, individual or group therapy, and medication management; admissions to acute psychiatric inpatient and crisis residential facilities (the latter are a community-based alternative to psychiatric hospitalization); and admissions to emergency services, including admissions to the psychiatric emergency unit and engagement by the psychiatric emergency response team, a group of specially trained officers and mental health providers.
We identified clients at their initial point of contact with the mental health system, defined as the first use of service after a 12-month period without service use. Using six fiscal years of data, we excluded clients who used services in the first fiscal year (July 1, 1999, through June 30, 2000) and then identified each client's first service across the next five fiscal years (July 1, 2000, through June 30, 2005). We classified the location of this service (inpatient, emergency, or outpatient) as the point of first contact. We then identified three six-month windows after the initiation of service use and computed the use of inpatient, emergency, and outpatient services during each of these periods. Thus three observations per patient were constructed to capture service use in three six-month periods corresponding to zero to six months, seven to 12 months, and 13 to 18 months after initial contact. We expected that three six-month periods would allow us to examine clinically relevant changes in service utilization over time. We excluded persons without a full 18-month exposure period (that is, those who initiated services after January 2004). We also excluded subsequent service use periods if, for example, clients received additional services after another 12-month period of nonutilization.
We identified three outpatient programs where clients with limited English proficiency received a majority of their outpatient services. Asians in San Diego County are less numerous and relatively localized residentially compared with Latinos, who are more numerous and more geographically dispersed. Among Asian clients with limited English proficiency who used outpatient services, 82% received a majority of their services from an outpatient program administered by an organization that specializes in providing services in numerous languages to the Pan-Asian community in San Diego. Only 15% of English-proficient Asian clients received a majority of their services at this clinic. Among Latino clients with limited English proficiency who used outpatient services, 32% received a majority of their services from one of two outpatient programs in the South Bay region of San Diego, which has a high proportion of Latino residents. Only 17% of English-proficient Latino clients received a majority of their services at these clinics. We created dummy variables to indicate the receipt of a majority of outpatient services at each of these three programs. We also created an interaction variable for clients with limited English proficiency who received a majority of their services from clinics that were focused on providing services to clients with limited English proficiency. We included these variables in the analysis of outpatient service use intensity described below.
Statistical analyses
We first compared clients on demographic and clinical characteristics at the initial use of service. The group with limited English proficiency and the English-proficient group were initially compared on demographic and clinical characteristics. These data were analyzed at the person level by using t tests and chi square tests, as appropriate, to test for the significance of pairwise comparisons. Data on non-Latino whites provided a reference group.
Second, we analyzed point of first contact using multinomial logistic regression, adjusting for age, gender, diagnosis, Medi-Cal coverage (versus being uninsured), and GAF score. Predicted probabilities were calculated for each group and set of first contact points. These probabilities were standardized to the underlying population characteristics by calculating, for example, the predicted probability of initial inpatient use among Spanish-speaking Latinos as the mean predicted probability of inpatient use among all persons as if all were Spanish-speaking Latinos. Standard errors of these estimates were calculated by using the nonparametric bootstrap, and p values for pairwise comparisons were computed from these empirical distributions (
29 ).
Third, we analyzed mental health service use over time. Probability of service use by type of mental health service and six-month period was compared among the ethnic and language groups by using multivariate logistic regressions, which adjusted for the differences in demographic and clinical characteristics noted above. These data were analyzed as person-periods with three observations per person, one corresponding to each six-month period. We included interactions between ethnicity and language and time period to capture change in service use over time. Because there were substantial changes in service use across time periods (especially from the first to the second six-month period), we did not attempt to model within-client correlation. Instead, we adjusted the estimated covariance matrices to account for nonindependence of observations at the client level (
30 ). As described above, predicted probabilities, standardized to the underlying population characteristics, were calculated for each group and type of service. Standard errors were calculated by using the nonparametric bootstrap with the sampling procedure adjusted for nonindependence; p values were computed from the empirical distributions (
29 ).
Fourth, we analyzed intensity of outpatient service utilization by using a two-part model (
31 ). The two-part model is commonly used to estimate health care utilization and costs when the dependent variable is nonnegative and when its distribution is noticeably skewed and kurtotic (with a heavy right-hand tail). In this application, logistic regression was used to estimate the probability of use, and a generalized linear regression (specified as having a gamma distribution with a log link function) was used to estimate the number of outpatient services among clients receiving at least one service (
32,
33 ). We employed a gamma model rather than a count model (for example, a negative binomial model) because the distribution of outpatient services was nearly continuous. These data were analyzed as person-periods, with the analysis adjusting for demographic and clinical characteristics as well as six indicator variables for three clinics with large numbers of clients with limited English proficiency and interactions for clients with limited English proficiency who were receiving a majority of their services at these clinics.
Covariance matrices were adjusted to account for nonindependence of observations at the client level (
30 ). Standardized estimates of mean outpatient visits were calculated for each ethnicity-language group and six-month period over both parts of the model (probability of use and conditional use). Standardized estimates were also calculated for clients with limited English proficiency and English-proficient clients over the entire period for each of the three clinics that had large numbers of clients with limited English proficiency. Standard errors and p values were computed as described above. [These models are described in more detail in a technical appendix that is available as an online supplement to this article at ps.psychiatryonline.org.]
Results
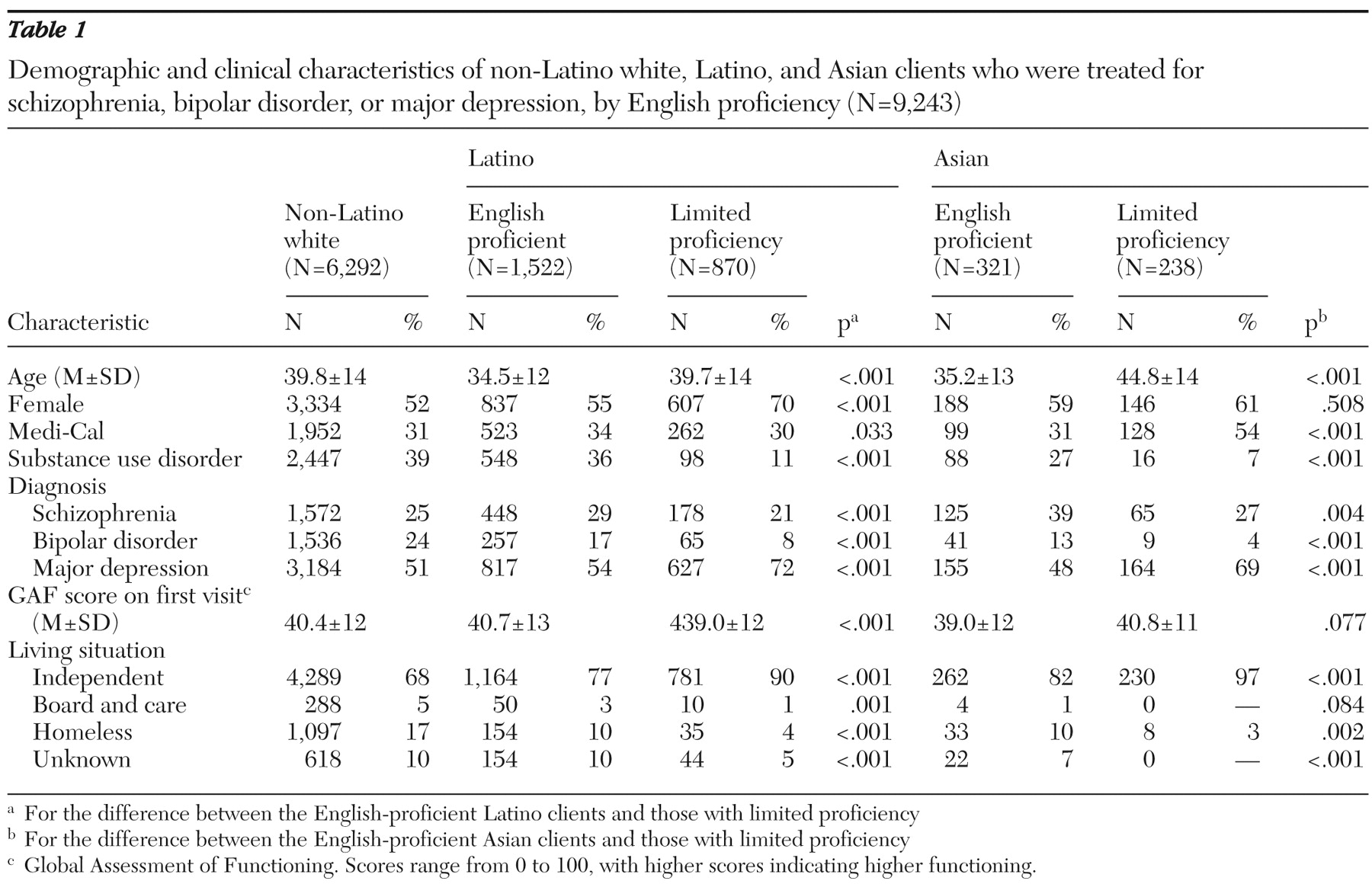
Table 1 summarizes the sociodemographic characteristics of clients with limited English proficiency and those with proficiency. This study of clients with severe mental illness identified 2,392 Latinos (1,522 with English proficiency and 870 with limited proficiency), 559 Asians (321 and 238, respectively), and 6,292 non-Latino whites (all English proficient) who were living in the community and who initiated use of public mental health services during fiscal years 2000–2004.
Among Asian clients, 157 (28%) were Filipino, 129 (23%) were Vietnamese, 45 (8%) were Chinese, 39 (7%) were Cambodian, 38 (7%) were Japanese, and 27% were from other Asian ethnic groups. A large number of Latino and Asian populations had specific linguistic needs; 43% of Asian clients reported a preference for services in Asian languages, and 36% of Latinos reported a preference for Spanish-language services. As shown in
Table 1, compared with Latinos who were proficient in English, Latino clients with limited proficiency were older, less likely to be diagnosed as having schizophrenia or bipolar disorder (they were more likely to have major depression), less likely to be diagnosed as having a substance use disorder, and more likely to live independently. Latino clients with limited English proficiency were also more likely than English-proficient Latinos to be women and less likely to have Medi-Cal. Asian clients with limited English proficiency were older than English-proficient Asians and more likely to have Medi-Cal. The proportion of women was about the same in both Asian groups.
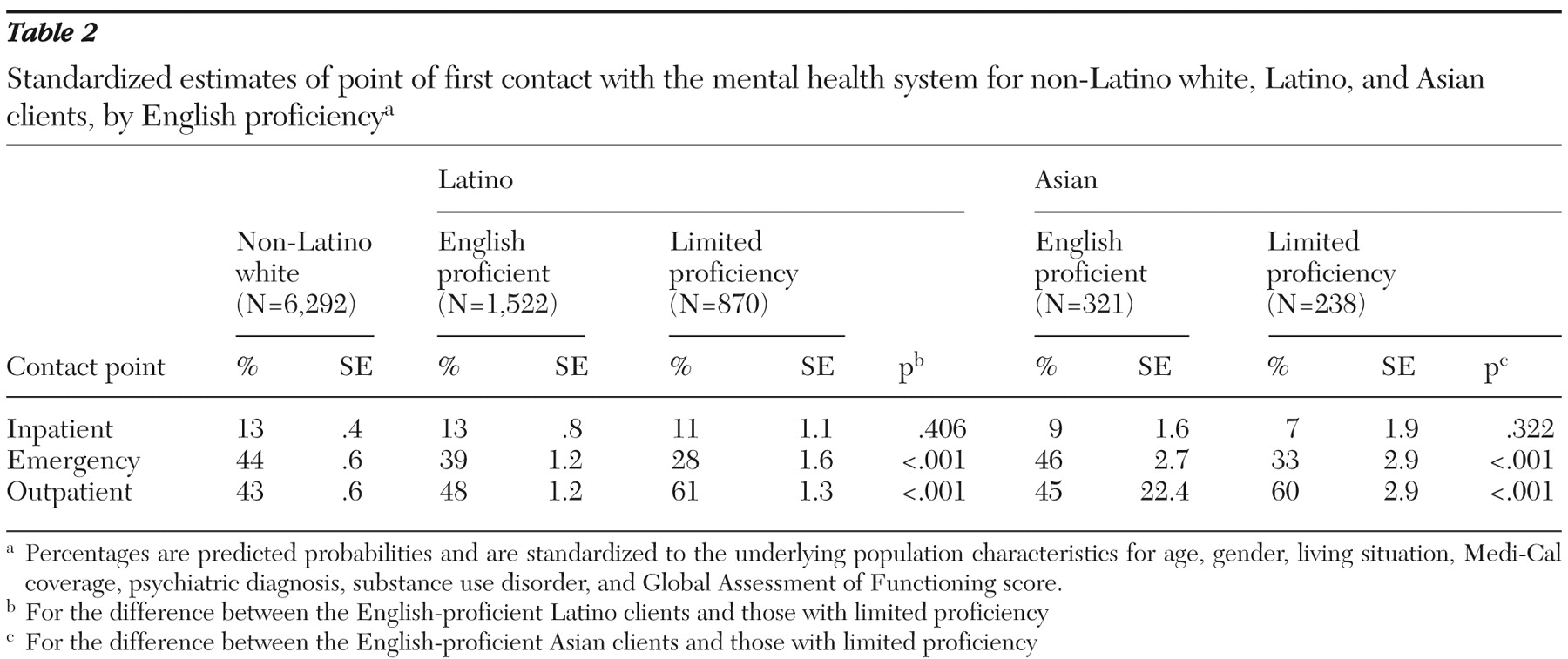
Standardized estimates of point of first contact by ethnicity and language status are shown in
Table 2 . We found that Latino clients who preferred to receive mental health care from providers who spoke Spanish and Asian clients who preferred to receive mental health care from providers using Asian languages were significantly less likely than English-proficient Latino or Asian clients to initially access the public mental health system through emergency services (among Latinos, 28% compared with 39%; among Asians, 33% compared with 46%); they were more likely to access the system through outpatient services (among Latinos, 61% compared with 48%; among Asians, 60% compared with 45%) (p<.001 for each comparison).
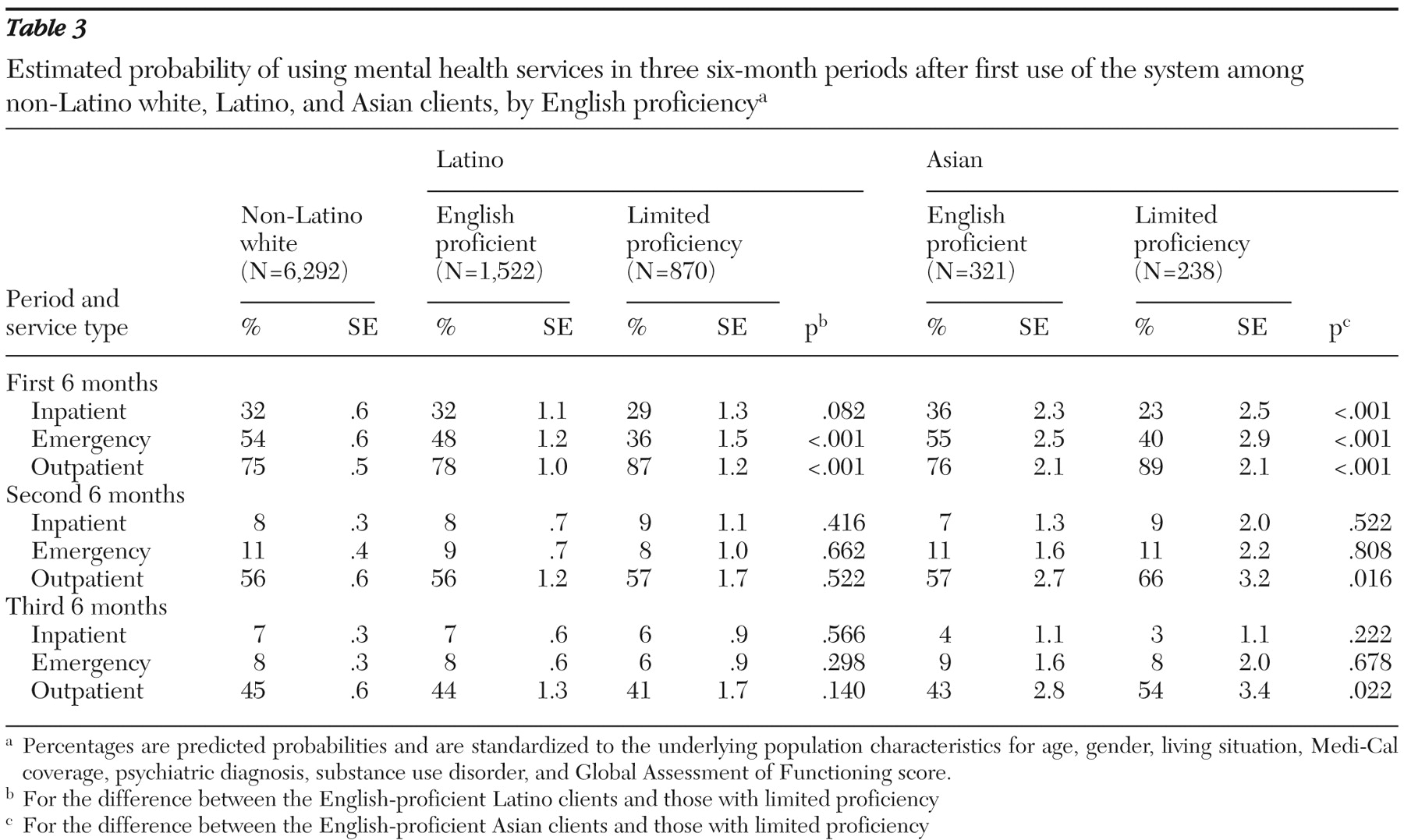
Table 3 shows the probability of using inpatient, emergency, and outpatient services across ethnicity and language groups in the three six-month periods after the initial visit. Results for the first period are similar to results from the analysis of point of first contact: Latinos and Asians with limited English proficiency were less likely than their English-proficient peers to use emergency services and were more likely to use outpatient services. Asian clients with limited English proficiency were also less likely than English-proficient Asian clients to use inpatient services or crisis residential facilities (23% compared with 36%, p<.001). However, service use in the second and third six-month periods was similar among clients with limited English proficiency and English-proficient clients, with the exception that Asians with limited proficiency remained more likely than English-proficient Asians to use outpatient services (66% compared with 57% in the second period, p=.016; and 54% compared with 43% in the third period, p=.022).
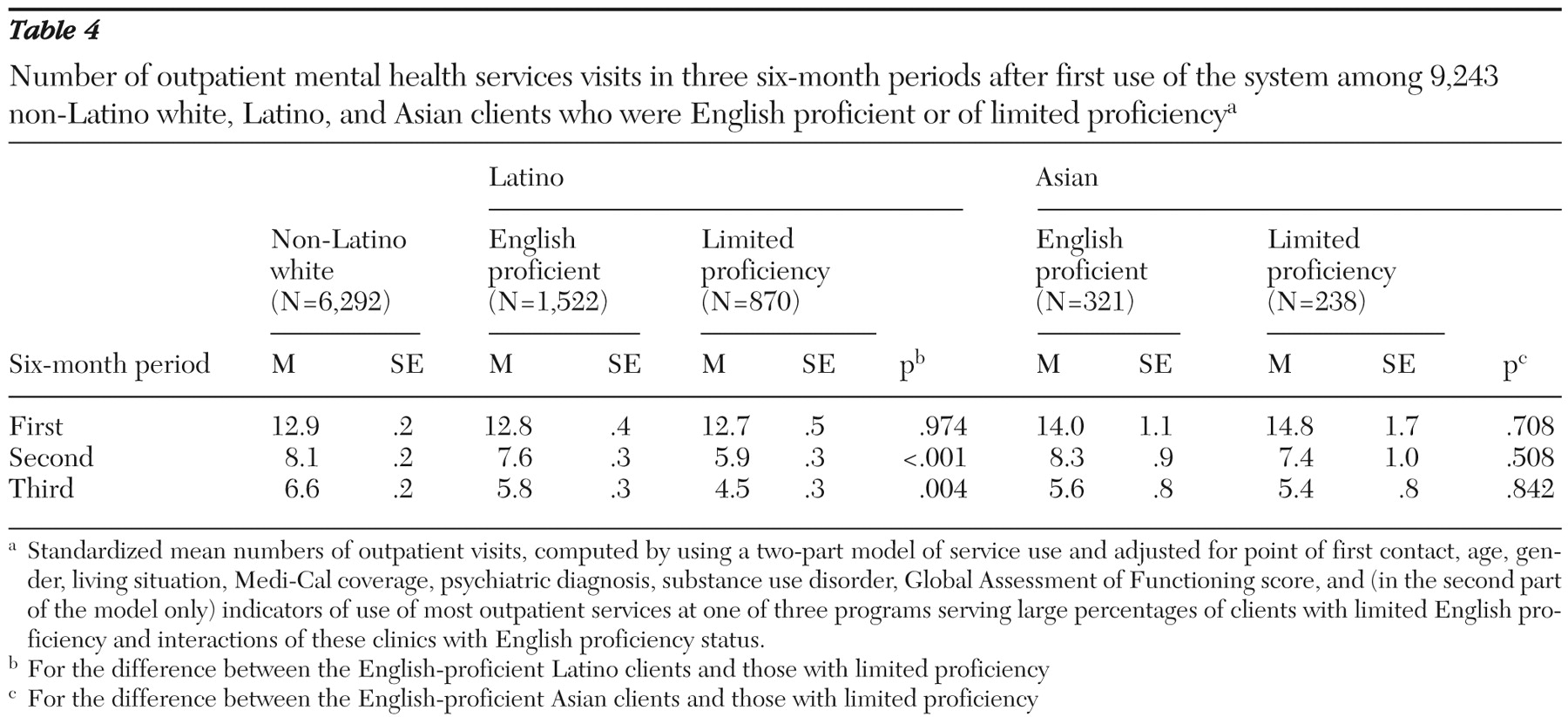
Standardized estimates of the intensity of outpatient service use are shown in
Table 4 . In the first six months after initial use, clients with limited English proficiency received a similar number of outpatient services as English-proficient clients. The experiences of Latino and Asian clients with limited English proficiency diverged in the later periods compared with their English-proficient peers. Latino clients with limited English proficiency had fewer outpatient visits than English-proficient Latino clients in the second period (5.9 compared with 7.6 visits, p<.001) and the third period (4.5 compared with 5.8, visits, p=.004). The number of visits by Asian clients with limited English proficiency was similar to the number made by their English-proficient peers.
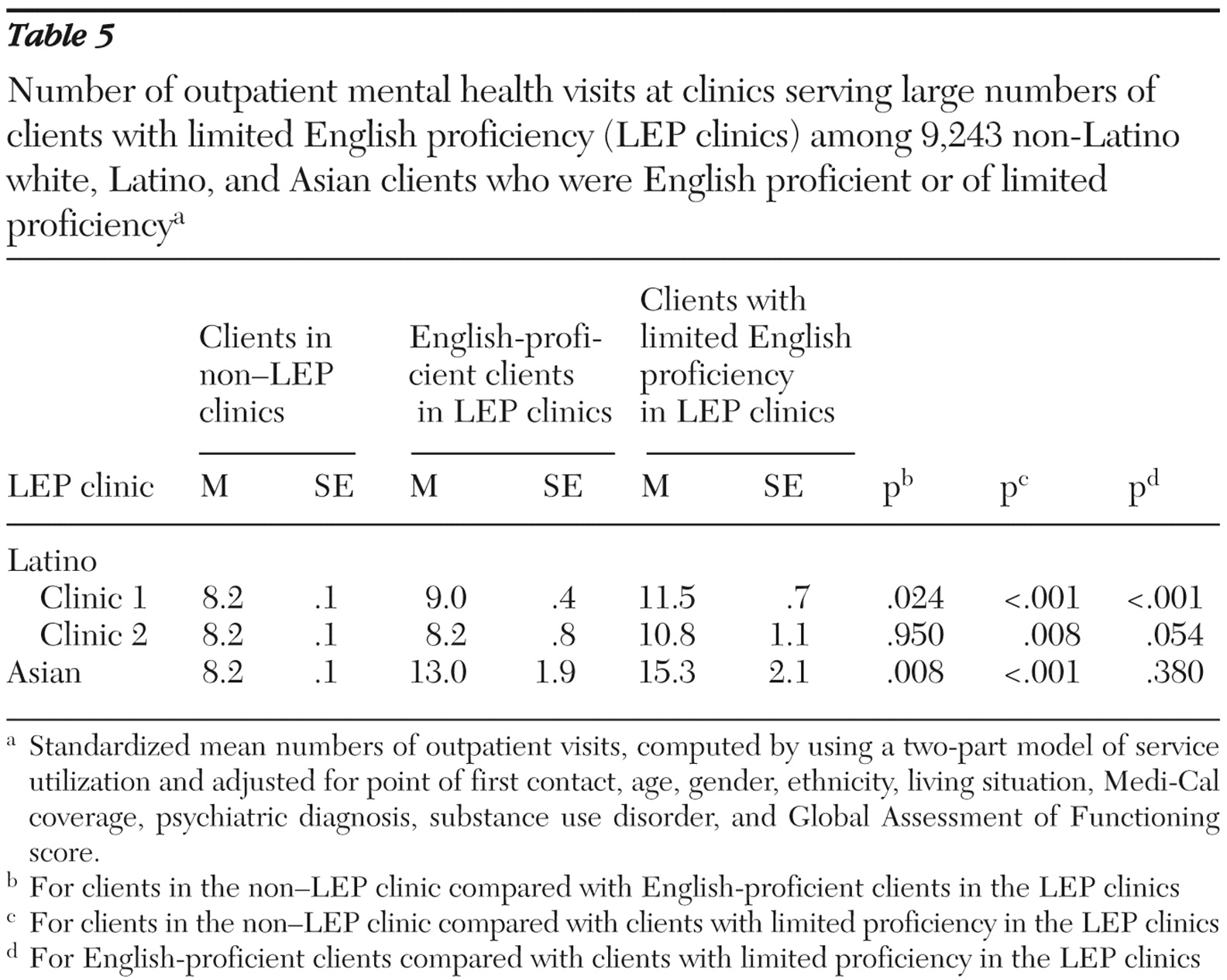
Standardized estimates of the intensity of outpatient service use for each of the three clinics serving large numbers of clients with limited English proficiency are shown in
Table 5 . Separate estimates are provided for English-proficient clients and clients with limited proficiency in each clinic. As a comparison, an estimate is also provided for clients of clinics that did not provide limited-English-proficiency services; this estimate is identical across clinics by design. Compared with clients in clinics that did not provide limited-English-proficiency services, English-proficient clients in one Latino clinic and in the Asian clinic that provided such services had a greater intensity of outpatient service use (p<.05 for each comparison). Clients with limited English proficiency in all three clinics had a greater intensity of outpatient service use than clients in clinics that did not provide limited-English-proficiency services (p<.01 for each comparison). In one Latino clinic that provided such services, clients with limited English proficiency had a greater intensity of outpatient service use than English-proficient clients (11.5 and 9.0 visits, p<.001).
Discussion
This study examined use of public mental health services by Latino and Asian clients with limited English proficiency compared with use by their English-proficient peers. We found that Latino and Asian clients with limited English proficiency were more likely than English-proficient clients to first access mental health services through outpatient providers than through emergency services (including the emergency psychiatric unit and psychiatric emergency response team). Similarly, in the first six months after their initial use of services, Latino and Asian clients with limited English proficiency were less likely to use emergency services and more likely to use outpatient services and had more outpatient visits than their English-proficient peers. Thus both patient groups with limited English proficiency had a more favorable initial pattern of mental health service use.
However, the experiences of Latino and Asian clients with limited English proficiency diverged in the later periods, with the Asian clients continuing to be more likely to receive outpatient services than English-proficient Asians. In contrast, Latino clients with limited English proficiency received fewer outpatient services over time than their English-proficient peers. We expect that a primary reason that clients with limited English proficiency are more likely than English-proficient clients to present in an outpatient setting is that they have higher levels of familial and other social support to help direct them to this setting. The divergence in utilization profiles between Latino and Asian clients with limited English proficiency after initial service use deserves further investigation.
Our analysis revealed a greater level of outpatient utilization among both English-proficient Asians and Asians with limited proficiency who were receiving services from a specific Asian-focused outpatient program. This organization has provided an array of services to San Diego's Asian and Pacific Islander communities since 1974; staff represent more than 30 Asian cultures, languages, and dialects. Its stated mission is to improve the general well-being and education of the Asian and Pacific Islander community as well as other ethnic communities in San Diego County while recognizing the diverse ethnic and cultural identities and strengths of these communities and their need for self-sufficiency.
We also found a greater level of outpatient utilization among both English-proficient Latinos and Latinos with limited English proficiency who were receiving services from a specific Latino-focused outpatient program (Latino clinic 1 in
Table 5 ). This clinic utilizes a cross-cultural model of assessment and intervention that is provided by a multidisciplinary and bilingual-bicultural team to ensure that the needs of the large Latino population in the U.S.-Mexico border region of San Diego are linguistically and culturally addressed. All Spanish-speaking consumers are able to receive services in their language of choice. Although the second clinic (Latino clinic 2 in
Table 5 ) has large numbers of Latino clients, it does not have a Latino focus in its mission statement.
Asian clients with limited English proficiency in this study received services primarily from a single Asian-focused program that was specifically funded by AOAMHS to provide culturally and linguistically competent services to Asian populations in San Diego. By contrast, Latino clients with limited English proficiency received services at multiple programs throughout the county. This geographic dispersion of the Latino population, combined with the fact that Latino clients with limited English proficiency outnumber Asian clients with limited English proficiency by 3.7 to 1, makes it more challenging to provide programs to Latino clients that focus on those with limited English proficiency. These findings reinforce the need for public mental health services that meet the specific needs of the client population. For persons with mental illness from ethnic minority groups, this includes access to linguistically appropriate mental health services. Future research could identify specific program effects that improve quality of care that might be replicated in other settings and for other populations with limited English proficiency.
Our results are limited by the use of administrative data, which do not capture all dimensions needed to fully study issues related to access and utilization of mental health services by ethnic minority populations. We lacked data on clients' self-reported English proficiency or on the language most commonly spoken at home, measures that have been used in other research examining the impacts of language on health service use (
34 ). Another limitation is a lack of detailed information on illness severity. Although we used the GAF in this investigation, a more detailed measure of psychopathology, such as the Positive and Negative Syndrome Scale or the Hamilton Rating Scale for Depression, may have provided a more reliable measure of severity. Without this information, it is impossible to determine whether the differences seen in this analysis are due to differences in illness severity rather than language proficiency. We were also unable to measure differences in service quality, improvements in functioning and quality of life, or client satisfaction with services, all of which are potentially important factors that could affect service utilization.
Conclusions
Despite these limitations, we believe that these findings are both important and timely. Counties in California are currently implementing new programs with funding legislated by the Mental Health Services Act (MHSA), which implements a supplemental tax on individuals with annual incomes above $1 million in order to expand public mental health services. One of the mandates of this MHSA funding is to expand services for the unserved and the underserved, many of whom are heavy users of inpatient and emergency services who use few outpatient services. In their planning efforts, the counties and their stakeholder planning groups must decide what additional services to provide and how to deliver them. AOAMHS has an explicit goal of improving access to services among Latino and Asian residents of San Diego County. These data suggest that culturally and linguistically competent programs may be an effective approach for engaging populations that are underrepresented in the mental health system.
Acknowledgments and disclosures
Financial support was provided by grants P30-MH-0066248 and K23-MH-067895 from the National Institute of Mental Health and by the Department of Veterans Affairs. The authors gratefully acknowledge the County of San Diego Health and Human Services Agency Adult and Older Adult Mental Health Services for access to the management information systems.
Dr. Jeste has received donations of antipsychotic medications for another study from AstraZeneca, Bristol-Myers Squibb, and Eli Lilly and Company. He is a consultant for Otsuka American Pharmaceuticals, Solvay Pharmaceuticals, and Wyeth Pharmaceuticals. The other authors report no competing interests.