Intimate partner violence is associated with severe psychopathology among its victims and costs the United States $5.8 billion annually in medical care and associated costs (
1 ). Studies investigating help seeking among battered women have found that they seek help from a wide variety of services, although most tend not to utilize specialized domestic violence services (
2 ). Furthermore, many battered women never receive mental health treatment (
3 ), with African-American women even less likely than white women to use mental health services (
4 ). No research with battered women (
2,
3,
4 ) has controlled for participants' medical coverage, and therefore, poor utilization could be a function of access. Also, battered women who seek shelter tend to have fewer resources than battered women in the community. Thus research with community samples of battered women (
2,
3,
4 ) may not generalize to battered women in shelters.
The purpose of this study was to investigate the frequency and types of resources battered women in shelters utilize before shelter admission and to determine which factors are related to greater use of mental health services and which factors are related to seeking help from a greater number of resources. We focused on both the number of resources accessed, including criminal justice services, and use of mental health resources because battered women seek help from a variety of specialized resources, in addition to mental health resources (
2,
3,
4 ). Furthermore, the criminal justice system often provides referrals for other social services and mental health resources. This study explored variables that previous research with battered women and other trauma populations have found to be associated with help seeking (race, socioeconomic status, abuse severity, and number of children) (
3 ) and with mental health treatment utilization (prior trauma, posttraumatic stress disorder [PTSD], and comorbidity) (
5 ). Unlike other studies, our study controlled for the potential confound of medical insurance status.
Methods
Data were collected from 164 battered women living in two shelters within the same shelter system between December 2004 and February 2007. All shelter residents were provided a brochure instructing them to contact research staff if they were interested in participating in the study. Only data from African-American women and white women were used, because race was a variable of interest and there was insufficient power to look at other racial and ethnic categories separately. All residents who reported violence from an intimate partner were eligible. Study procedures were approved by the Summa Health System Medical Review Committee, and all participants signed a written informed consent form.
Assessments included the Clinician Administered PTSD Scale (CAPS) (
6 ) for current PTSD related to partner violence; the mood, anxiety, and substance use modules of the Structured Clinical Interview for DSM-IV-TR Axis I Disorder, Patient Edition (SCID-I/P) (
7 ) for the number of current comorbid disorders; and a modified version of the treatment section of the Longitudinal Interval Follow-up Evaluation (LIFE) (
8 ) for service utilization in the past six months. Items were added to the LIFE to assess participants' use of community resources targeting battered women in addition to their use of traditional mental health services. Participants also completed the Revised Conflict Tactics Scales (
9 ) to assess abuse severity in the month before shelter admission and the Trauma History Questionnaire (
10 ) to assess the number of types of 24 potentially traumatic events other than domestic violence. All measures have established reliability and validity. All interviews were completed by trained graduate students in psychology or counseling under the direct supervision of a licensed psychologist. Interview training included detailed instruction, practice interviews, and observation of interviews. Interrater reliability was assessed for 11 randomly selected interviews for PTSD diagnoses (
κ =1.0) and for major depressive disorder diagnoses from the SCID (
κ =.814).
Descriptive statistics were run to determine the degree of service use over the past six months. Pearson chi square tests were calculated to determine whether service use differed as a function of race. To determine which factors most contributed to overall help seeking and use of mental health services, two regression analyses were conducted with race, medical coverage, education, employment status, number of children, abuse severity, number of prior traumas, current PTSD diagnosis, and number of comorbid disorders entered simultaneously as predictor variables. First, a regression equation was run with the number of formal supports utilized in the past six months as a dependent variable; then, a logistic regression was run with use of mental health services as a dependent variable.
Results
A total of 164 women participated in the study. Participants ranged from age 19 to 59 years (mean±SD=35.29±8.84). Seventy (43%) were white, 94 (57%) were African American, 121 (74%) were living with their abuser before admission, 126 (77%) had at least a high school degree or GED, and 118 (72%) were unemployed. Participants had an average of 2.4±1.7 children. Mean length of the index abusive relationship was 71.38±86.29 months, and participants had been in a shelter for a mean of 17.44±15.46 days at the time of the interview.
Participants reported experiencing an average of 7.23±4.40 different types of trauma besides domestic violence. The most frequently reported trauma types were rape (N=87, or 53%), robbery (N=76, or 46%), and a serious accident (N=75, or 46%). Regarding psychopathology, 113 (69%) met all diagnostic criteria for current PTSD related to partner violence, four (2%) met criteria for having acute stress disorder, 77 (47%) met criteria for having major depressive disorder, 31 (19%) met criteria for having another mood disorder, 21 (13%) met criteria for having a substance use disorder, and 69 (42%) met criteria for having another anxiety disorder. Average duration of PTSD symptoms was 38.57±69.38 months. African-American women had significantly more children (mean=2.7±1.94), compared with white women (mean=2.0±1.30). No racial differences were found for PTSD, education, employment status, medical coverage, number of different types of trauma, or abuse severity. Only 66 women (40%) received any mental health treatment in the past six months.
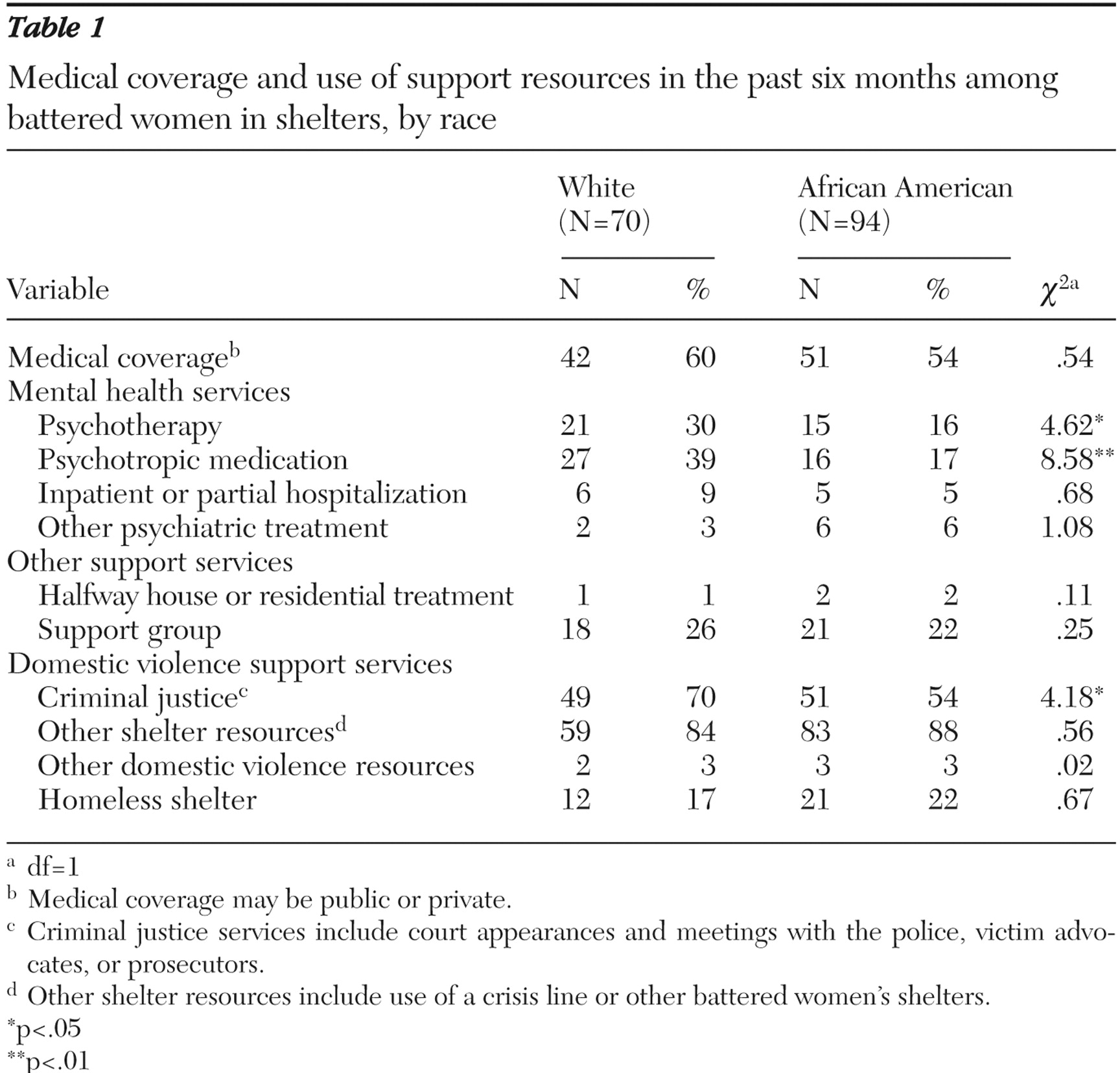
African-American women were significantly less likely than white women to use psychotherapy, psychotropic medications, and services provided by the criminal justice system (see
Table 1 ). Results of the multiple regression analysis suggest that battered women with more trauma types tended to seek help from significantly more sources (
β =.24, p<.01). No significant effects were found for race, medical coverage, education, employment status, number of children, abuse severity, current PTSD related to partner violence, and number of comorbid disorders.
Results of the logistic regression for use of mental health services indicate that African-American women were significantly less likely than white women to seek mental health services (odds ratio [OR]=.38, 95% confidence interval [CI]=.18–.80, p<.05), that women with medical coverage were significantly more likely than those without coverage to seek mental health treatment (OR=2.11, CI=1.02–4.38, p<.05), and that women with more trauma types were significantly more likely to seek mental health treatment (OR=1.20, CI=1.09–1.31, p<.001). No significant effects were found for education, employment, number of children, abuse severity, PTSD, and number of comorbid disorders. Additionally, because there was a significant racial difference in the number of children, the interaction between race and number of children was also tested in both regressions and was found to not be significant. Finally, a Pearson chi square test was computed to further evaluate the relationship between medical coverage and mental health treatment seeking. A significantly larger number of women who sought mental health treatment had medical coverage (43 of 65 women, or 66%) than did not (22 of 65 women, or 34%) (N=164, χ 2 =3.91, df=1, p<.05). However, only 43 of the 93 women with medical coverage (46%) received mental health treatment in the past six months.
Discussion
Consistent with prior research (
2 ), this report found that battered women in shelters seek help from a variety of different services. However, given the degree of need within this population, the degree of help seeking is less than expected. Although this population displayed significant psychopathology, a majority of women received no recent mental health treatment. Furthermore, consistent with prior research (
4 ), African-American women appear to utilize even fewer resources than white women, with African-American women less likely to access mental health treatment, as well as criminal justice interventions, even when the analyses controlled for socioeconomic status, number of children, and medical coverage. Many factors may contribute to African-American women's reduced use of mental health resources, including their tendency to rely on prayer and clergy in times of stress, as well as greater associated stigmatization within the African-American culture (
4 ).
Contrary to prior research with other trauma populations (
5 ), this study also found women with medical coverage to be more likely to utilize mental health resources, highlighting the importance of helping recent victims of partner violence obtain health coverage. However, even with medical coverage, only a minority of women sought mental health treatment (46%), suggesting that there are multiple barriers (for example, transportation and access to child care) that may interfere with battered women's use of mental health resources in addition to the possession of health coverage.
Besides race, number of traumas was the most consistent predictor of help seeking in this sample. Battered women with more trauma types tended to seek help from more resources, including mental health services. This finding suggests that help-seeking battered women have a complicated trauma history and highlights the importance of assessing for multiple traumas among battered women. Contrary to prior research with trauma survivors (
5 ), this study did not find that abuse severity, current PTSD, or comorbidity was significantly related to help seeking by battered women in shelters. Our finding may reflect the severe impairment of women with mental illness plus the burden of recent battery, which can impede seeking help. Additionally, there may have been a ceiling effect, given the high rate of PTSD in this sample (69%). Limitations of this study include its cross-sectional design, relatively small sample size, and use of retrospective report of trauma and abuse. Further, it is possible that some participants sought resources outside of the six-month window assessed. Strengths of this research are inclusion of medical coverage as a control variable, as well as standardized clinical interviews to assess PTSD related to partner violence, comorbidity, and treatment utilization in a well-defined and ethnically diverse sample of battered women in shelters.
Conclusions
Battered women in shelters have a great need for multiple resources. However, few of the women in our sample, in particular African-American women, utilized available resources, especially mental health treatment. Future research should examine the barriers, including medical coverage, battered women face in utilizing mental health and other resources.
Acknowledgments and disclosures
This research was supported by grant K23-MH-067648 from the National Institute of Mental Health and by pilot funds from the Summa-Kent State Center for the Treatment and Study of Traumatic Stress. The authors thank Cynthia Cluster, M.A., Keri Pinna, M.A., Sara Perez, M.A., and the Battered Women's Shelter of Summit and Medina Counties for their assistance in data collection.
The authors report no competing interests.