Unfortunately, 40% to 80% of individuals on second-generation antipsychotic medications gain up to 20% of their ideal body weight. Clozapine and olanzapine are the worst offenders (
1 ). In fact, the second-generation antipsychotic medications cause more weight gain than the low-potency first-generation antipsychotic medications (
1,
2,
3,
4 ). Weight gain is also associated with the use of many other psychotropic medications, including mood stabilizers and antidepressants (
5 ). For people taking these medications, weight gain and its sequelae are major health concerns.
Among people with schizophrenia, antipsychotic medications and poor lifestyle factors contribute to high rates of obesity, hyperlipidemia, and diabetes (
6,
7,
8 ). People with schizophrenia frequently experience motivation and energy problems, symptoms that reduce their capacity for healthy nutrition and regular physical activity (
9,
10 ). What makes matters worse is that second-generation antipsychotic medications increase the risk of diabetes and lipid abnormalities (
8,
11 ). Also, the fear of weight gain may undermine medication compliance (
12 ), which may lead to relapse.
One approach to weight gain is regular exercise at a gym. Archie and colleagues (
13 ) offered patients with schizophrenia a six-month membership to a YMCA fitness facility and at six months found a high drop-out rate. The main reason given for poor attendance was lack of motivation. Motivating a patient to participate in an exercise program that he or she is not ready for poses a great challenge for clinicians.
The transtheoretical model (
14,
15 ), also known as the stages of change model, helps clinicians assess patients' readiness for changing lifestyle factors. It identifies six stages of change: precontemplation, contemplation, preparation, action, maintenance, and relapse. During the contemplation stage, therapists motivate individuals by training them to use cognitive strategies, such as decisional balance—that is, weighing the pros and cons of exercise. During the action stage, therapists train individuals to use behavioral strategies, such as scheduling rewards for completing exercise, to mobilize action (
14 ).
According to randomized control trials, the transtheoretical model may be more effective than standard interventions in promoting physical activity in sedentary but healthy populations (
16,
17,
18 ). But many researchers have criticized this model because in general populations it did not predict level of physical activity (
19 ). Nevertheless, the literature provides some evidence that use of this model increases physical activity (
20,
21 ) when researchers target intervention strategies (motivational interviewing, cognitive therapy, or behavioral therapy) to participants' readiness to change.
Despite the success of the transtheoretical model in promoting adaptive behaviors in schizophrenia populations (
22,
23 ), use of this model for lifestyle counseling has been largely ignored by the schizophrenia research community. In response to these concerns, we aimed to identify the diet and physical activity patterns of persons with a psychotic disorder and to use the transtheoretical model to identify a subgroup of patients who were ready to consider lifestyle changes.
Methods
A cross-sectional survey design was used to collect information about the stages of change for physical activity and eating habits among individuals given a diagnosis of schizophrenia or other psychotic disorders. The research ethics boards of Hamilton Health Sciences and McMaster University approved the study protocol.
Trained medical and nursing students, supervised by a research nurse, conducted the study between June 2004 and April 2005. The research assistants recruited all interested clinic patients who met all the eligibility criteria, obtained informed consent, and ensured that participation was voluntary and confidential. Each participant completed self-administered questionnaires, with the assistance of a research assistant if any questions needed clarification.
Study population and setting
The population of interest comprised all community patients with a psychotic disorder who were taking antipsychotic medications. It involved a convenience sample of clinic patients who met all the inclusion criteria. The first 101 eligible patients who agreed to participate entered the study. Patients were approached by clinic staff while waiting for their appointments. Eligible patients were between 18 and 55 years of age, were on an antipsychotic medication, had outpatient status, and had a
DSM-IV (
24 ) diagnosis of schizophrenia, schizoaffective disorder, delusional disorder, bipolar disorder, or depression with psychotic features or a first episode of psychosis. The study defined "first episode" as the first illness episode involving psychotic symptoms of a patient who had received less than six months of antipsychotic medication treatment before clinic involvement. Psychotic symptoms included the following (
4 ): delusions, hallucinations, marked formal thought disorder, and grossly disorganized, bizarre, or inappropriate behavior. Diagnosis was confirmed by chart review.
All participants were registered patients from the Psychotic Disorders Clinic or the Hamilton Program for Schizophrenia: ambulatory clinics in Canada that specialized in treating patients with schizophrenia and other psychotic disorders. Clinic referrals were from family physicians, emergency departments, teaching hospitals, and other psychiatrists.
Measures
Body mass index (BMI) was calculated as weight in kilograms divided by the square of height in meters. All participants were measured by the research assistants at the time of questionnaire completion.
Stages of change were assessed by using the Patient-Centered Assessment and Counseling for Exercise and Nutrition (PACE) questionnaires (
21,
25,
26 ). The PACE protocol simplifies the traditional six stages of change into three stages that approximate the precontemplation, contemplation-preparation, and action stages. The PACE assessment forms for nutrition and physical activity help health care providers understand their client's readiness to engage in more healthy eating habits or physical activity. Participants simply choose the statement that they feel reflects their usual eating habits—for example "I eat fewer than 5 servings per day of fruits and vegetables, and I have been thinking about starting to eat more in the next 6 months" represents the "ready to change" stage. The PACE nutrition statement selected by the participant determines whether the respondent is not ready to change (precontemplation), ready to change (contemplation-preparation), or meeting guidelines (action stage) for healthy eating habits. The PACE physical activity score determines whether the respondent is inactive and not ready (precontemplation), inactive but ready (contemplation-preparation), or active (action stage).
Body image was assessed with the Adult Body Satisfaction Questionnaire (
27 ). It has two main factors, body appearance and body function. It has been standardized on middle-aged and older adults, and it correlates with level of fitness, measures of body satisfaction, and subjective well-being.
Physical activity was assessed with the Godin Leisure Time Exercise Questionnaire (
28 ). This questionnaire rates intensity of physical activity over a seven-day period as vigorous, moderate, or mild and rates frequency of physical activity over a seven-day period as often, sometimes, or never. Participants circle the recreational activities they engage in regularly, such as walking, jogging, or hockey.
The Dietary Fat Screener and the Fruit and Vegetable and Fibre Screener are standardized, one-page food intake screeners that monitor fat, fruit, and vegetable intake (
29 ). It correlates with the 100-item Block Food Frequency Questionnaire (
30 ). It can be completed in five minutes and does not require elaborate recording of foods or portion sizes. The screener identifies individuals with a high percentage of calories from fat and those with a low intake of fruits and vegetables.
Statistical methods
Data analyses were performed with SPSS. One-way analysis of variance was used to examine associations between patient characteristics and lifestyle factors (BMI, body function, body appearance, fat intake, and fruit and vegetable intake). We compared stages of change, fat intake, and fruit and vegetable intake with normative data by using the chi square test. All post hoc comparisons were performed by using the Bonferroni adjustments for multiple comparisons. Associations between stages of change, physical activity, and medication were conducted by using the chi square test or Fisher's exact test if more than 20% of cells had an expected count of less than five. All p values presented are two-tailed; p<.05 was considered statistically significant.
Results
Demographic data
One hundred and four interested patients were approached, and only three (3%) of these patients declined to participate. The patients who declined all had schizophrenia, two of them were women, and their ages ranged from 22 to 33 years old. There were no apparent differences between those who agreed to participate and those who declined.
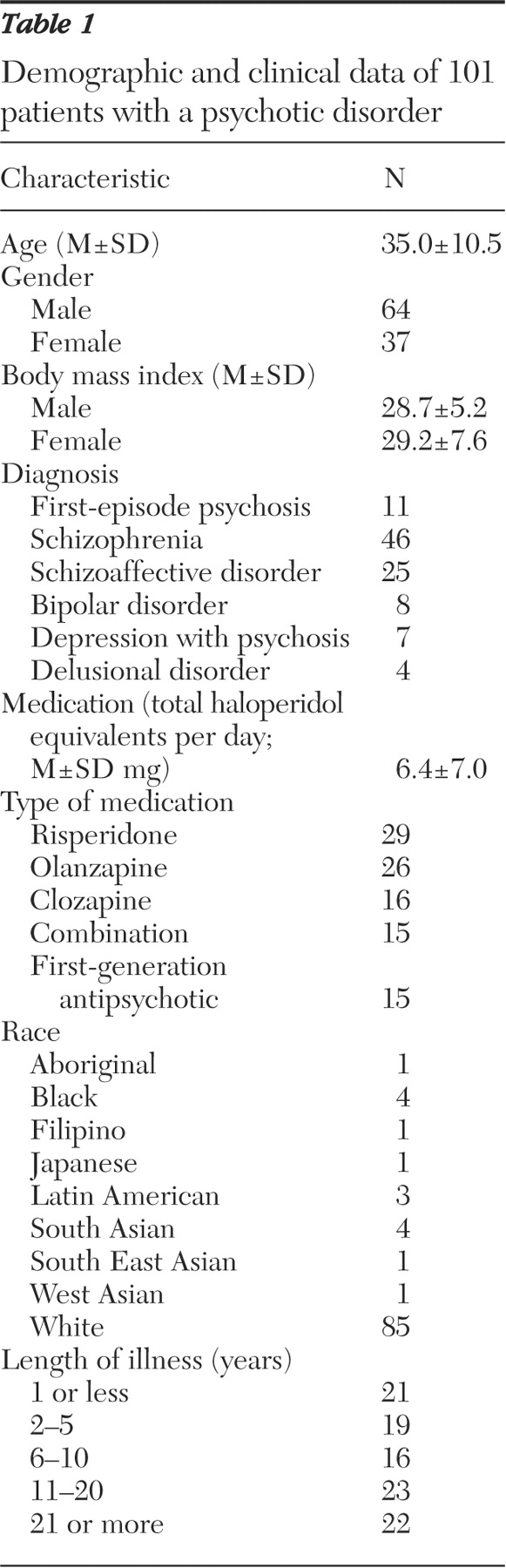
A total of 101 participants aged 18 to 55 years completed this study. However, data were missing on BMI, body appearance, and total fat intake for two participants. In addition, for one of these two participants, data were missing on body function and fruit and vegetable intake.
Table 1 shows the clinical and demographic characteristics of the sample. Schizophrenia and schizoaffective disorder were the most common diagnoses, occurring in 71% of the sample; bipolar disorder and depression with psychotic features (affective psychoses) occurred in 15% of the sample. A majority of the sample was Caucasian and was treated with second-generation antipsychotic medications. The mean BMI score for women was higher than that for men, but this difference did not reach statistical significance.
The relationship between weight and dosage of antipsychotic medication was statistically significant (Spearman ρ =.225, p=.02). (Dosage was calculated by converting all antipsychotic medications to haldol equivalents.) Because of the expected small frequencies in cross-tabulation, we were unable to assess the relationship between type of medication (second or first generation) and BMI category. Because of the cross-sectional design of this study, we were unable to assess the relationship between type of medication and weight gain over time.
Of the 99 participants for whom a BMI score was calculated, only 24% had BMI scores within the normal range (BMI of 18.5-24.9), and yet, according to Statistics Canada, 46.7% of Canadians had BMI scores within the normal range (
31 ). In fact, 38% of the sample were overweight (BMI of 25.0-29.9), compared with 33.3% of Canadians, and 36% of the sample were obese (BMI≥30), compared with 14% of Canadians. Overall, the BMI scores of the study sample were significantly higher than those of the general population in Canada as reported by the 2003 Statistics Canada Canadian Health Survey (
χ 2 =40.75, df=3, p<.001).
U.S. data suggest that women with schizophrenia have significantly higher BMIs than women in the general population (BMIs of 27.4 versus 24.5, respectively) (
9 ). U.S. data also showed that the mean BMI for men with schizophrenia was similar to that of men without schizophrenia, but both groups had a high proportion of BMIs in the obese range (35% versus 25%, respectively) (
9 ).
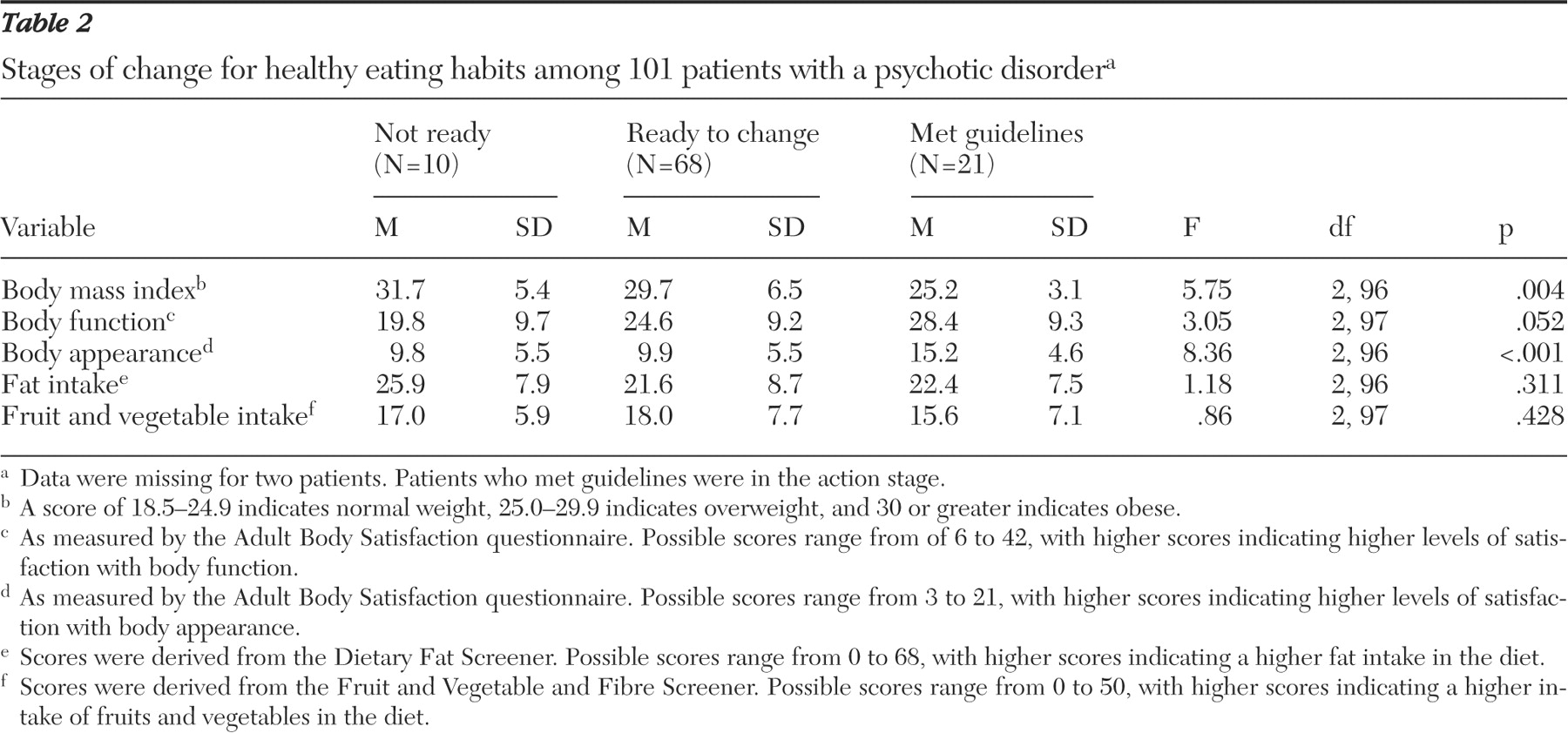
Stages of change for healthy eating habits
Table 2 shows that the stages of change for eating habits were significantly associated with BMI. Overall, the group that was not ready to improve eating habits was obese, the group that was ready to change was overweight, and the group that met guidelines was normal weight. Participants who meet guidelines had significantly better perceptions of their body function and appearance than those in the other two groups.
Stages of change for eating habits and for physical activity were significantly associated with each other (Fisher's exact test, p=.04). Thus participants who were in the contemplation-preparation stage for eating habits were also in the contemplation-preparation stage for physical activity habits. No significant differences existed between the readiness-to-change groups for healthy eating on the basis of gender. Because of the expected small frequencies in cross-tabulation, we were not able to assess the relationship between stages of change for healthy eating and type of antipsychotic medication (risperidone, olanzapine, clozapine, first generation, or combination) or diagnosis.
Stages of change for physical activity
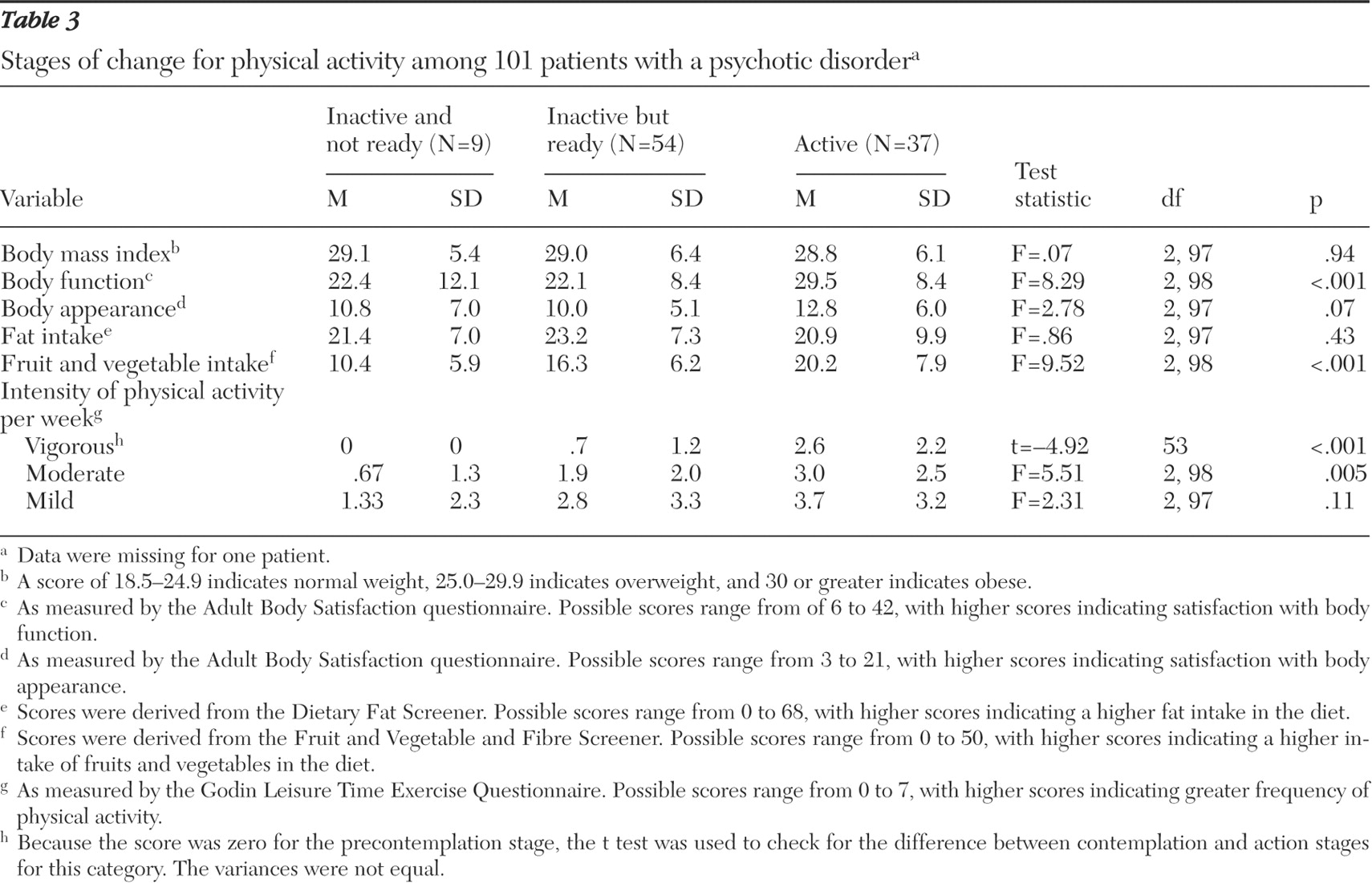
The PACE counseling protocol for physical activities suggests the following proportions of family practice patients will meet criteria for the stages of change: 10%, not ready to change stage (precontemplation); 50%, ready to change stage (contemplation-preparation stage); and 40%, meets guidelines (action stage) (
25 ). Fifty-four percent of our sample were in the contemplation-preparation stage for physical activity, similar to the proportion reported in the PACE manual (
2 ). As shown in
Table 3, stages of change for physical activity were associated with vigorous- and moderate-intensity physical activity. Stages of change for physical activity were also associated with both fruit and vegetable intake and perceived body function but not perceived appearance. Thus participants in the contemplation-preparation stage for physical activity were eating more fruits and vegetables than those who were not ready to change their physical activity habits. Unlike stages of change for eating habits, stages of change for physical activity were not associated with BMI. Furthermore, no significant differences existed between the three stages for physical activity by diagnosis or type of medication.
Diet and physical activity habits
The mean fruit and vegetable score for our sample was 17.5±7.5, well above a score of 11, which represents three servings a day of fruit and vegetables (
29 ). Unfortunately, the mean±SD score that measures fat intake was 22.2±8.3, just below 23, the score that represents unacceptable levels of fat. Women had significantly higher mean fruit and vegetable scores than men (t=2.00, df=99, p<.05). Men and women had the same fat intake scores. However, when we converted the fat intake scores into total fat and saturated fat estimates (
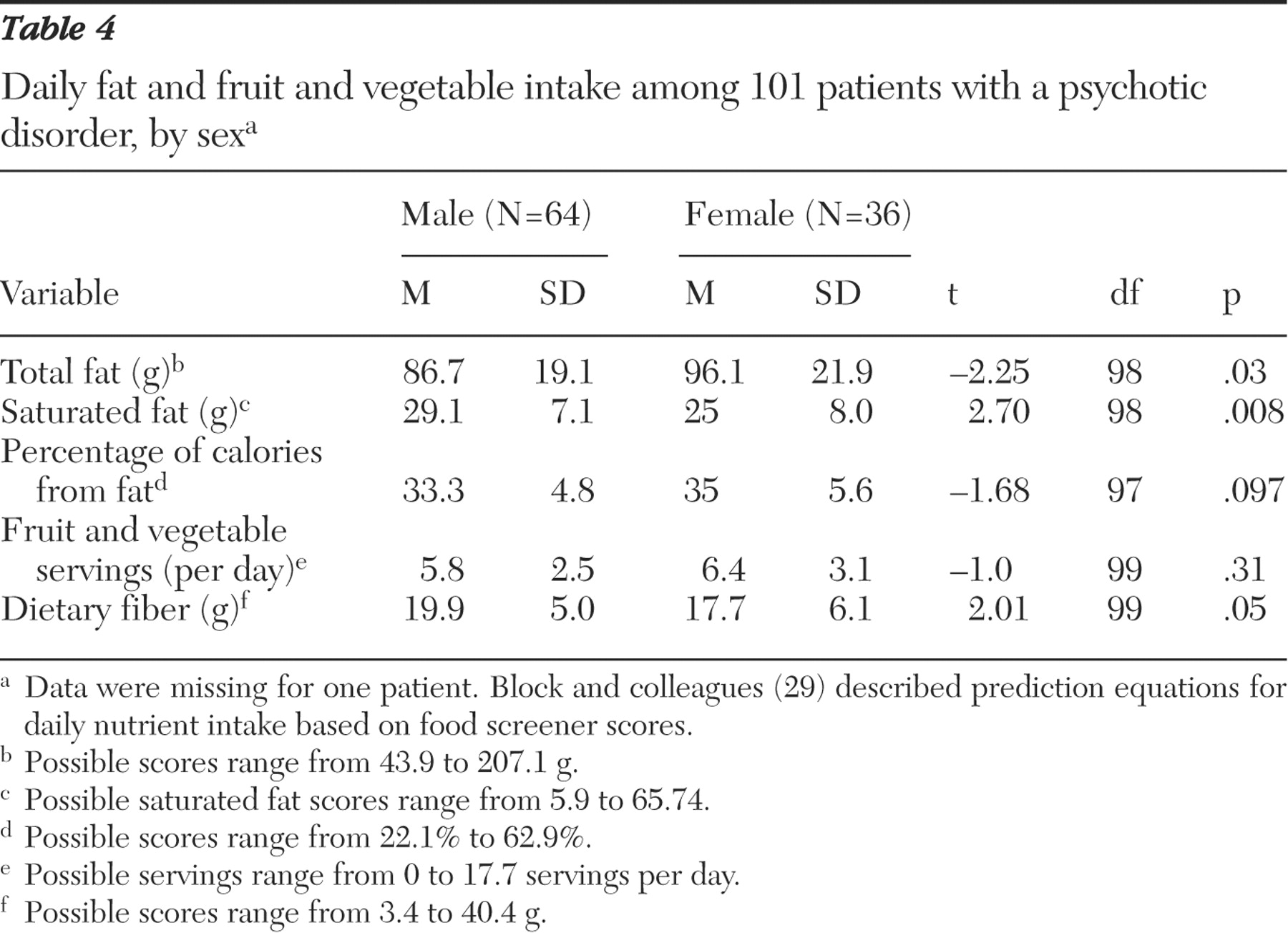
Table 4 )—on the basis of prediction equations for daily nutrient intake reported by Block and colleagues (
29 )—women had significantly higher mean intake of total fat (in grams) than men; yet men had significantly higher mean intake of saturated fat (in grams) than women. Dietary fiber intake for men was significantly higher than that for women.
The sample as a whole consumed vegetables and fiber infrequently: 8% consumed vegetables once a day, 17% consumed fruit at least twice a day, and 38% consumed green salad once a week. The most commonly consumed high-fat foods included whole milk, margarine, mayonnaise, French fries, and cheese.
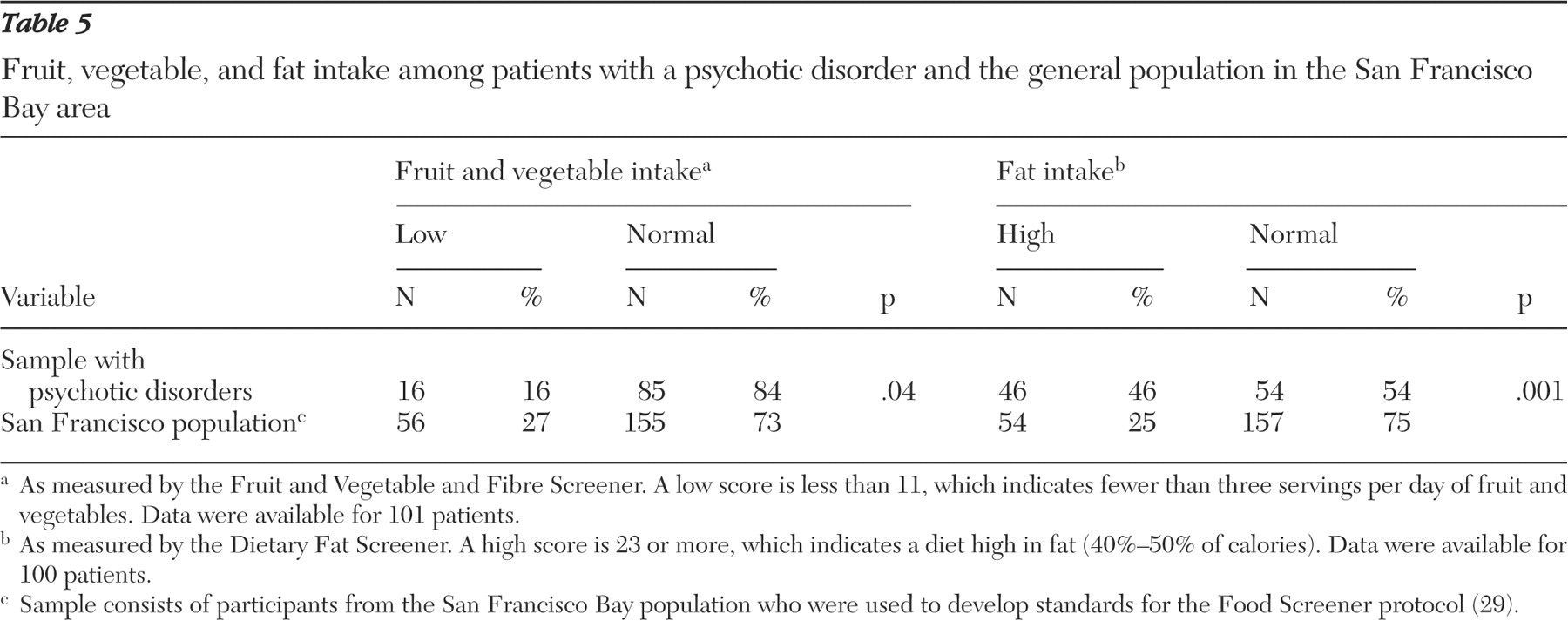
Table 5 shows that our sample's fruit and vegetable intake was significantly higher than that of the San Francisco Bay sample, which was used to standardize the protocol; however, our sample's fat intake was significantly higher than that of the San Francisco Bay sample (
29 ). The San Francisco Bay area sample consisted of 208 employees invited to participate in a Nutrition Education and Research Program conducted by the University of California (
29 ). The sample was predominantly white (68%) and female (64%), and the ages ranged between 20 and 69 years of age. In summary, our sample's diet was too high in fat but was better for fruit and vegetable intake. Women's diets were high in total fat, but men's diets were higher in saturated fat. A high saturated fat intake is associated with increased lipid levels and a high monosaturated fat intake.
Not surprisingly, the physical activity levels were also low for our sample. On average, our sample exercised for 30 minutes a mean of 1.4±1.9 times per week. The British Heart Foundation recommends 30 minutes of vigorous exercise five times per week (
32 ). Only 15% of the sample rated their physical activity over a seven-day period as occurring often, 48% rated it as occurring sometimes, and 38% rated it as never occurring. The most common physical activities engaged in regularly by those in the contemplation-preparation stage included walking (73%), bicycling (20%), and jogging (11%).
Discussion
Not only did this study identify a target group of patients with psychotic disorders that was contemplating changing their eating habits, but it also identified a target group that was contemplating changing physical activity habits. Those in the contemplation-preparation group for eating habits were characterized by increased self-perceived satisfaction with body function, increased fruit and vegetable intake, and increased intensity and frequency of physical activity, whereas those in the contemplation-preparation stage for physical activity were characterized by lower BMI, increased readiness to consider changing physical activity habits, and increased self-perceived satisfaction with body function and appearance.
Fifty percent of our sample were in the contemplation-preparation stage; only 10% were in the precontemplation stage for either eating habits or physical activity. This finding is in stark contrast to previous studies in schizophrenia populations, which found lower proportions of patients in the contemplation-preparation stage (
33,
34 ). Furthermore, even though our sample's fat intake and physical activity habits were not as good as those in the general population, we found that our sample was just as interested as a general sample in changing physical activity habits (
25 ), and it indicates that our sample's perceived fruit and vegetable intake was higher than that of the San Francisco Bay sample. Our findings differ from those of most studies (
35,
36 ), but few studies have actually investigated whether patients are considering lifestyle changes. In addition, our patients are regularly counseled on fruit and vegetable intake to protect against the weight gain and constipation caused by the antipsychotic medications.
Despite these encouraging findings, we identified several "special needs" concerns. Too many participants avoided good sources of fiber. Only 15% of participants engaged in regular physical activity. Furthermore, this study confirmed the significantly higher BMI scores among populations with psychosis, compared with the general population. Our results suggest that stages of change for eating habits are associated with BMI: participants in the contemplation-preparation stage were at increased risk of being overweight; even worse, participants in the precontemplation stage were at risk of being obese.
Although women ate more fruits and vegetables than men, the total fat consumption of women was significantly higher than that of men; however, men had significantly higher intake of saturated fat (in grams) than women. Saturated fats are linked to cardiovascular disease. This finding suggests that women are making healthier choices regarding fat intake than men. We did not find significant gender differences for BMI (
9 ), but the sample size may have been insufficient to detect any differences.
This study has some weaknesses that limit its generalizability—lack of a matched control group, use of a convenience sampling method, and a small sample. Our study participants may be different from most patients with a psychotic disorder—for example, our sample was willing to participate in a study on diet and exercise, suggesting they might be more interested than most in lifestyle factors. The study used self-report questionnaires, and therefore, the participants may have overestimated their fruit or vegetable intake or their level of physical activity. Family members or health care providers may have estimated food intake or activity level differently. Also, we did not measure weight gain, even though weight gain is associated with second-generation antipsychotic medication (
37 ).
Conclusions
Our study results suggest that more patients may be ready to consider lifestyle changes than clinicians realize. Mental health workers often overlook diet and exercise as viable interventions for people with mental illness (
38 ). Very few controlled trials of lifestyle interventions exist for this population (
39 ). However, a few studies suggest modest improvements in weight can be achieved through lifestyle interventions (
40,
41,
42,
43 ). Our findings suggest that walking, jogging, and bicycling are acceptable and feasible exercises for this population. Fortunately, these activities are inexpensive and beneficial for preventing disease and promoting health and well-being (
38 ). Educating patients about saturated fat content in commonly consumed foods, such as whole milk and butter, may help them to make healthier food choices.
Identifying a patient's stage of change could help clinicians individually tailor lifestyle counseling. Patients in the precontemplation stage could be encouraged to identify potential benefits, drawbacks, and roadblocks to healthy eating or physical activity. Patients in the precontemplation stage could also benefit from motivational interviewing because it allows them to explore their own goals and take a more active role in their treatment (
44,
45 ). Patients ready for change (contemplation-preparation group) could be encouraged to use decisional balance: weighing the benefits and costs of healthy lifestyle activities. Finally, patients in the action stage could be shown how to reward themselves for healthy choices to reinforce healthy habits. Ultimately, in choosing the most suitable antipsychotic medication, clinicians could consider an individual's stage of change, choosing antipsychotics that confer the least weight gain, such as ziprasidone (
4 ), for those in the precontemplation stage.
Acknowledgments and disclosures
The authors thank Rainka Joshi, Sarah Clarke, and Susan Gensey for their help with data collection. They also thank Harriet Woodside, O.T., for her comments on the manuscript. The authors acknowledge Kathleen Martin Ginis, Ph.D., for her recommendations regarding appropriate instruments to assess physical activity. The authors also thank Shelley Osborne, R.N., and Heather Hobbs, R.N., for their support with the data collection. The authors also thank Julie Buffett.
The authors report no competing interests.