Although efficacious treatments are available, most people with mental disorders do not receive even minimally adequate treatment (
1,
2,
3,
4,
5,
6,
7,
8,
9 ). Theoretical models of help-seeking behavior suggest that individuals progress through several stages before seeking mental health treatment. These stages include experiencing symptoms, evaluating the severity and consequences of the symptoms, assessing whether treatment is required, assessing the feasibility of and options for treatment, and deciding whether to seek treatment (
10 ). There has been emerging interest in understanding perceived barriers to use of mental health services. These barriers have been broadly divided into individual attitudinal factors (such as fear of stigmatization) and system-level structural factors (such as financial cost of services) (
11,
12,
13,
14,
15 ).
Previous work has demonstrated that emotionally distressed individuals most commonly identify attitudinal barriers (such as wishing to solve the problem on their own and thoughts that the emotional problem would go away) for not seeking mental health treatment (
14,
15 ). Although fear of stigmatization (
11 ) is commonly thought to be an important reason for not seeking mental health treatment, the limited number of studies (
14,
15 ) have not found fear of stigmatization to be a commonly reported barrier to seeking treatment for emotional problems.
Structural barriers, such as financial cost for mental health treatment, also may affect use of mental health services. This issue has been highly controversial, especially in the United States (
14,
15 ). In one of the very few cross-national comparisons published to date, Wells and colleagues (
14 ) demonstrated that psychologically distressed U.S. respondents were significantly more likely than respondents in New Zealand to report financial barriers as a reason for not seeking mental health treatment. In contrast with the Wells and colleagues study, a more recent study by Alegria and colleagues (
16 ) used data from three countries—the United States, Canada, and the Netherlands. They found that the income level of the respondents did not significantly affect the overall prevalence of outpatient use of mental health services across the three countries.
It remains unclear whether the greater reporting of financial barriers by the U.S. respondents noted in the Wells and colleagues study (
14 ) is a true financial hardship or indicates an unwillingness to pay that is not necessarily tied to financial resources. However, more recent administrative data from Toronto demonstrated that claimants from neighborhoods with the highest socioeconomic status were 1.6 times as likely as those from neighborhoods with the lowest socioeconomic status to utilize specialty care (
17,
18 ). In short, it remains unclear whether there are cross-national differences in structural barriers to use of mental health services.
Building on previous work, this study extends the literature on this topic by examining data from the same three surveys used by Alegria and colleagues (
16 ). The three surveys—the National Comorbidity Survey (NCS) (
19 ), the Ontario Health Survey (OHS) (
20,
21 ), and the Netherlands Mental Health Survey and Incidence Study (NEMESIS) (
22 )—were large population-based surveys that have been extensively studied and described in the literature (
23,
24,
25,
26,
27,
28,
29,
30 ). These surveys were conducted with much larger samples than Wells and colleagues (
14 ) used. Two—the NCS and the NEMESIS—are nationally representative data sets, whereas the third (OHS) is representative of the province of Ontario, Canada. All three surveys used the same methodology for assessment of mental disorders, asked the same questions related to perceived need for mental health treatment, and asked respondents to endorse the same list of possible reasons for not seeking treatment. Although collected in the 1990s, the NCS, OHS, and NEMESIS data sets are, to the best of our knowledge, the most accessible data sets that allow for a cross-national comparison of perceived barriers to use of mental health services. Because the differences among the health care systems in the United States, Canada, and the Netherlands have been previously described (
6,
16,
23,
31,
32 ), we only summarize them here (see
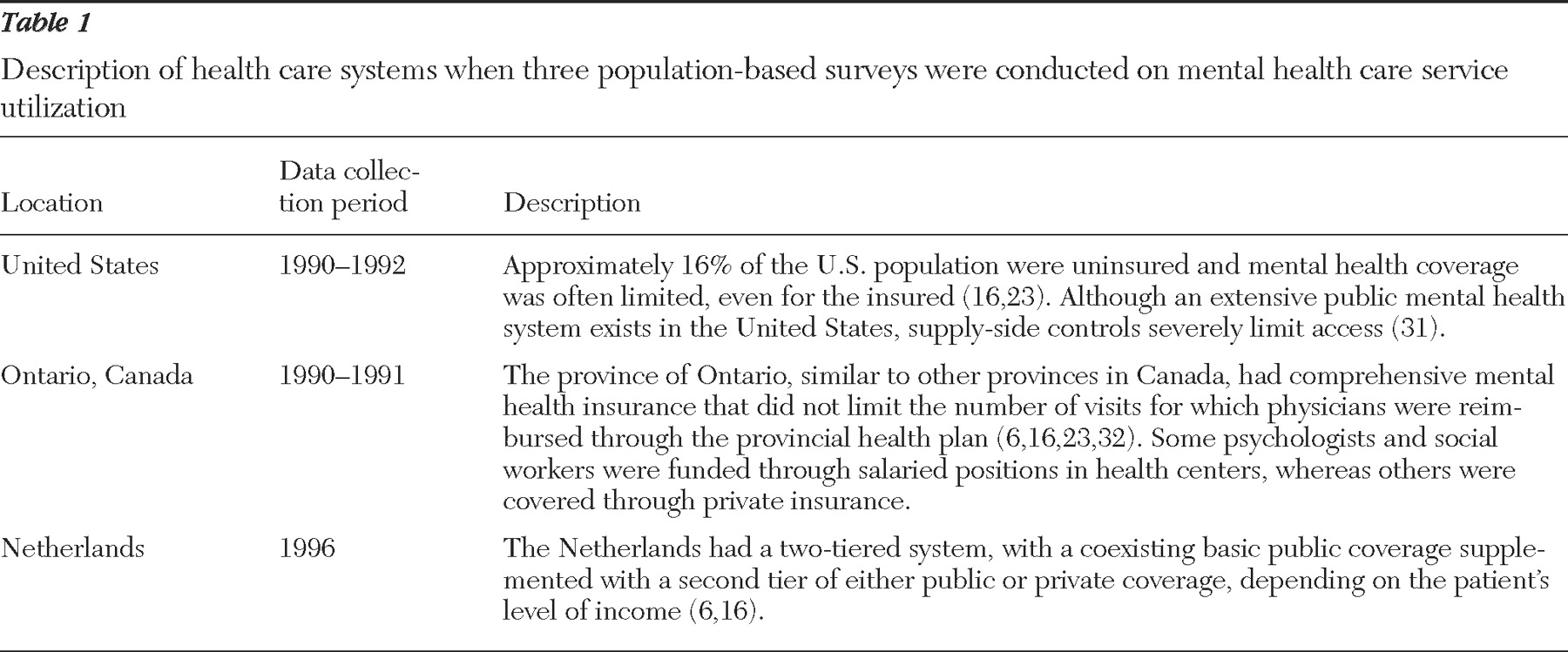
Table 1 ).
The aim of this study was to systematically explore the distribution of self-reported barriers to use of mental health services within and across three countries with differing health care systems. We also examined the sociodemographic and mental disorder correlates of each of the barriers.
Methods
Surveys
Data came from the U.S. NCS between 1990 and 1992 (N=5,384), the OHS between 1990 and 1991 (N=6,261), and the NEMESIS in 1996 (N=6,031) (
16,
19,
21,
33 ). Each of these surveys conducted face-to-face interviews with a probability sample of the general population and obtained parallel information on the prevalence of
DSM-III-R mental disorders and use of services. Response rates for the surveys were 82.4% in the NCS (
19 ), 67.4% in the OHS (
21 ), and 69.7% in the NEMESIS (
34 ). Details of the design of each of the surveys have been published extensively (
23,
24,
25,
28,
29,
33,
35,
36,
37,
38,
39 ). Because the age range of the three surveys differed slightly, all analyses were based on the age range of 18 to 54 years.
Perceived barriers
In each survey, all respondents were asked, "Was there ever a time during the past 12 months when you felt that you might need to see a professional because of problems with your emotions, nerves, or your use of alcohol or drugs but didn't go?" If this question was endorsed, a follow-up question asked respondents their reasons for not going. The respondents were asked to endorse all the reasons that were applicable from a list of reasons. The choices were not mutually exclusive.
Mental disorders
Across the three surveys, the highly reliable and valid Composite International Diagnostic Interview (CIDI) (
40,
41 ) was used to make
DSM-III-R mental disorder diagnoses. We categorized three mental disorder variables: past-year mood disorder (major depression, dysthymia, and bipolar disorder), past-year anxiety disorder (social phobia, simple phobia, panic disorder, agoraphobia, and generalized anxiety disorder), and past-year substance use disorder (alcohol abuse or dependence and drug abuse or dependence). We considered whether to limit the analysis to those meeting criteria for a mental disorder diagnosis assessed in the survey. However, previous work has demonstrated that perceived need without meeting criteria for a mental disorder is associated with disability, distress, and suicidal behavior (
42,
43 ). Thus we decided to include all respondents who reported a perceived need for treatment.
Sociodemographic variables
Age was measured in number of years across four categories (18–24, 25–34, 35–44, and 45–54 years). Education was measured by the highest level of attainment and was then dichotomized into less than grade 12 or grade 12 or more. Marital status was divided into three categories: never married; married or common-law marriage; and separated, divorced, or widowed. (Because race and ethnicity variables were not comparable across data sets, we do not report on them here.)
We carefully considered the optimal method of defining income groups for comparison between locations (
16,
23,
36 ). There are multiple methods to define comparable income groups, each with strengths and limitations. A standardized income measure based on distributions of income in each site was considered the optimal method of creating income groups (
44 ). All respondents in each survey were asked questions about the total family income before income tax deductions. First, we divided the family income by the number of people living in the household. Next, in each of the surveys, all respondents' income status was divided by the median income level in each of the represented countries. On the basis of this ratio, we created three categories of income: poor (less than .5), low to average income (.5–1.0), and above-average income (greater than 1.0) (
16,
23,
36 ).
Statistical analysis
We combined the three surveys into one data set. In all analyses, the appropriate statistical weight was used to ensure the data were representative of the population of each survey. Standard errors were calculated by using the Taylor series linearization method in the SUDAAN program (
45 ) and stratification information provided in each survey specifically for calculating design-based standard errors.
First, we used chi square analyses to determine within-site and between-site differences in perceived need for mental health treatment without seeking care associated with sociodemographic factors and mental disorders. Second, we examined whether there were within-site differences between those with and without a mental disorder in reporting of perceived barriers. Third, we used multiple logistic regression to determine the between-site, sociodemographic and mental disorder correlates of barriers to use of mental health services. Here, we limited the sample to individuals with perceived need who did not seek care and entered all the sociodemographic variables, mental disorder variables, and the three sites (Netherlands, Ontario, and the United States) in the same regression to determine the correlates of each barrier.
Because of small cell sizes in the four age categories, we used a continuous measure of age rather than categories. In the first set of regressions, the reference site was the OHS, and in the second set of regressions, the reference site was the NEMESIS. Finally, we examined whether there were significant interactions between place of residence and income level or type of mental disorder for each of the reported barriers. In multiple regression analyses testing the income-by-site interaction, we adjusted for age, gender, education, and marital status. To test the interactions of mental disorder and site, we again adjusted for all sociodemographic factors (age, gender, education, income, and marital status). For the conservative reader, a significance level of p<.01 was established for all analyses.
Results
The prevalence of perceived need for professional mental health treatment without seeking care was 6.5% (95% confidence interval [CI]=5.9–7.2), 6.5% (CI=5.5–7.5), and 7.1% (CI=6.2–8.0) for the NEMESIS, OHS, and NCS, respectively. These prevalence rates did not differ significantly across sites.
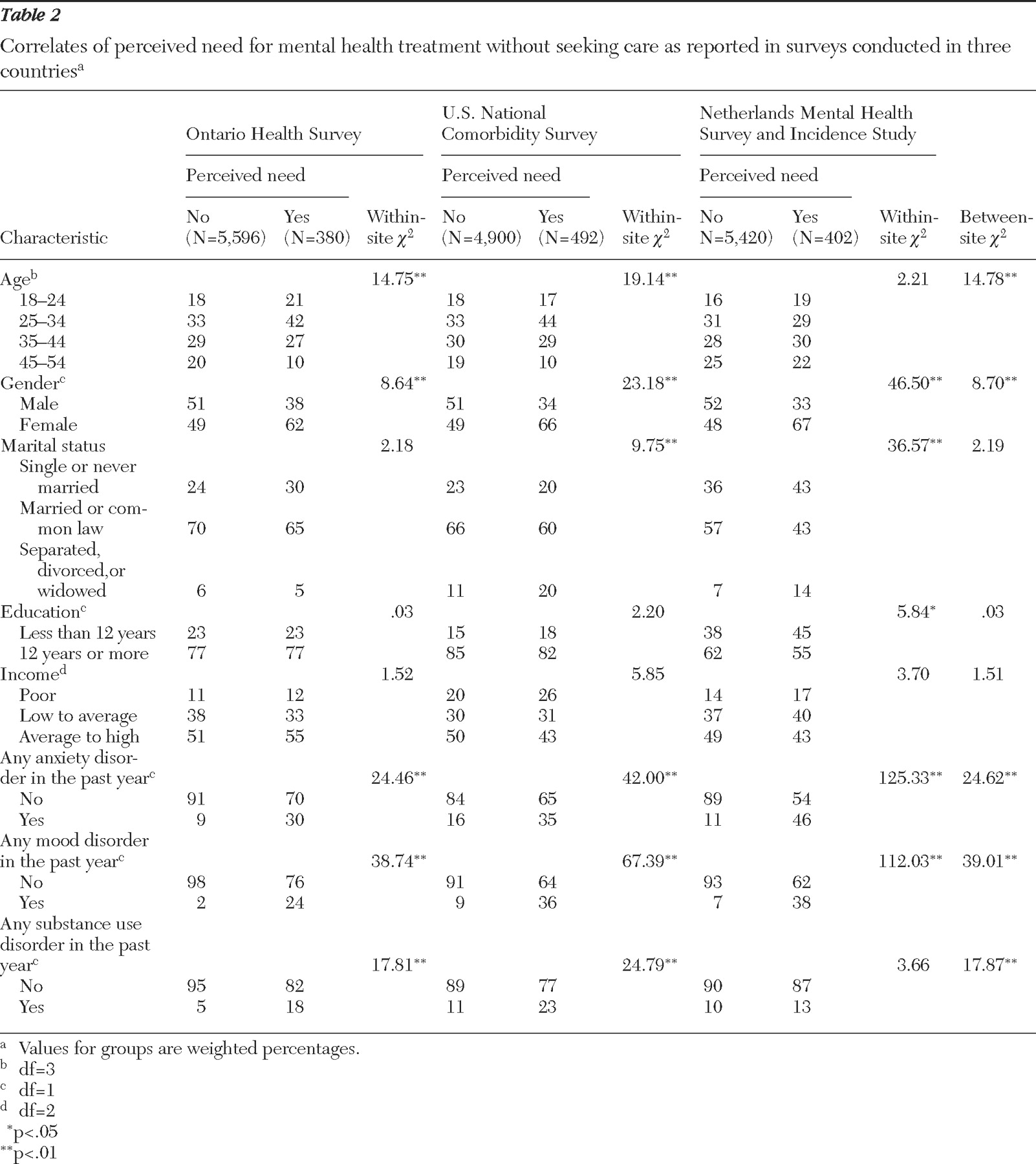
Table 2 illustrates the significant between-site differences in the presence of perceived need that were found for age, gender, and past-year anxiety, mood, and substance use disorders.
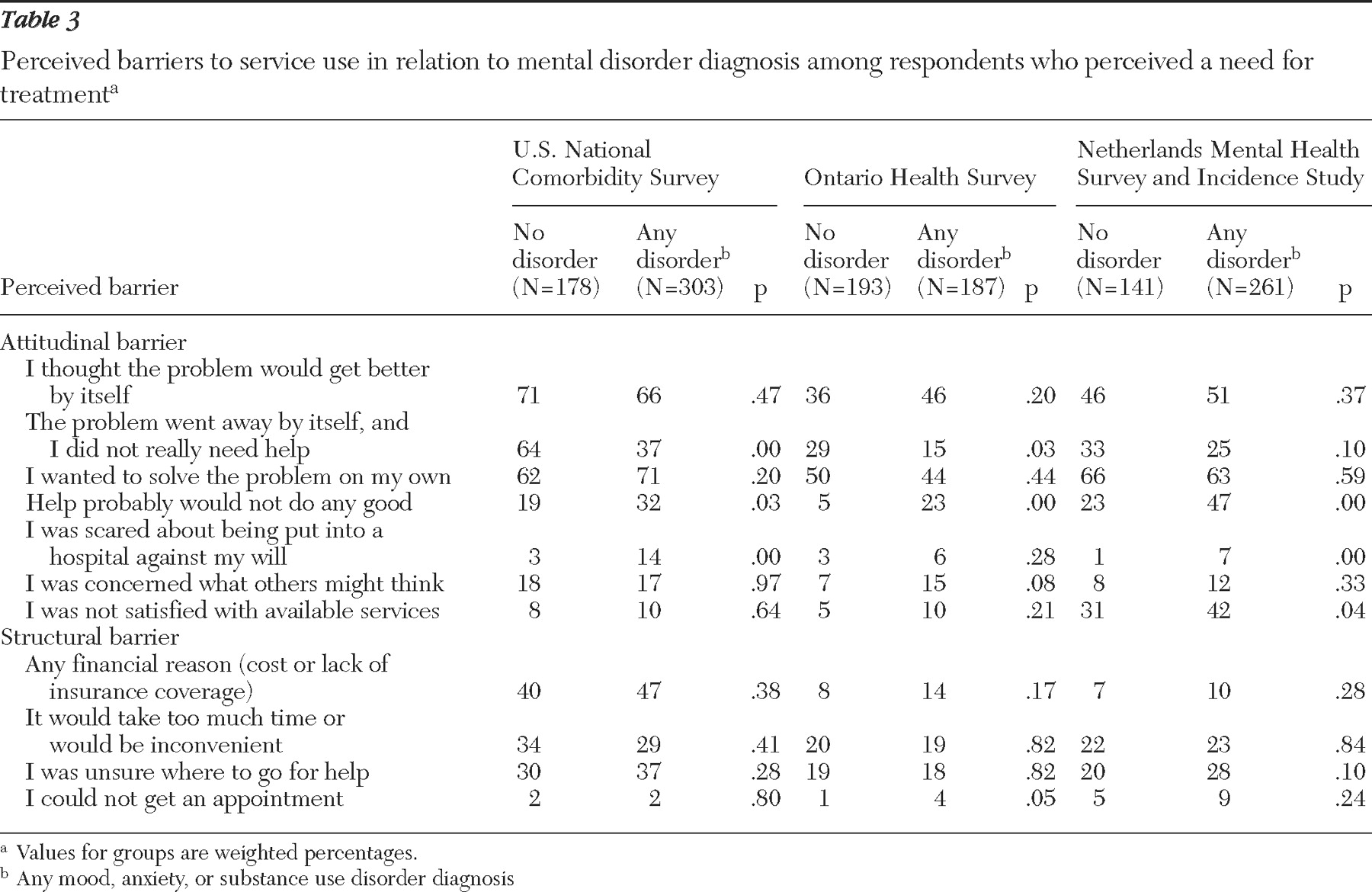
The overall pattern of reporting of barriers across the three sites was similar between respondents with or without a mental disorder (
Table 3 ). Individuals without a mental disorder were more likely than those with a mental disorder to report that "the problem went away." On the other hand, individuals with a mental disorder diagnosis were more likely than those without a mental disorder to report that "help probably would not do any good" and a fear of involuntary hospitalization.
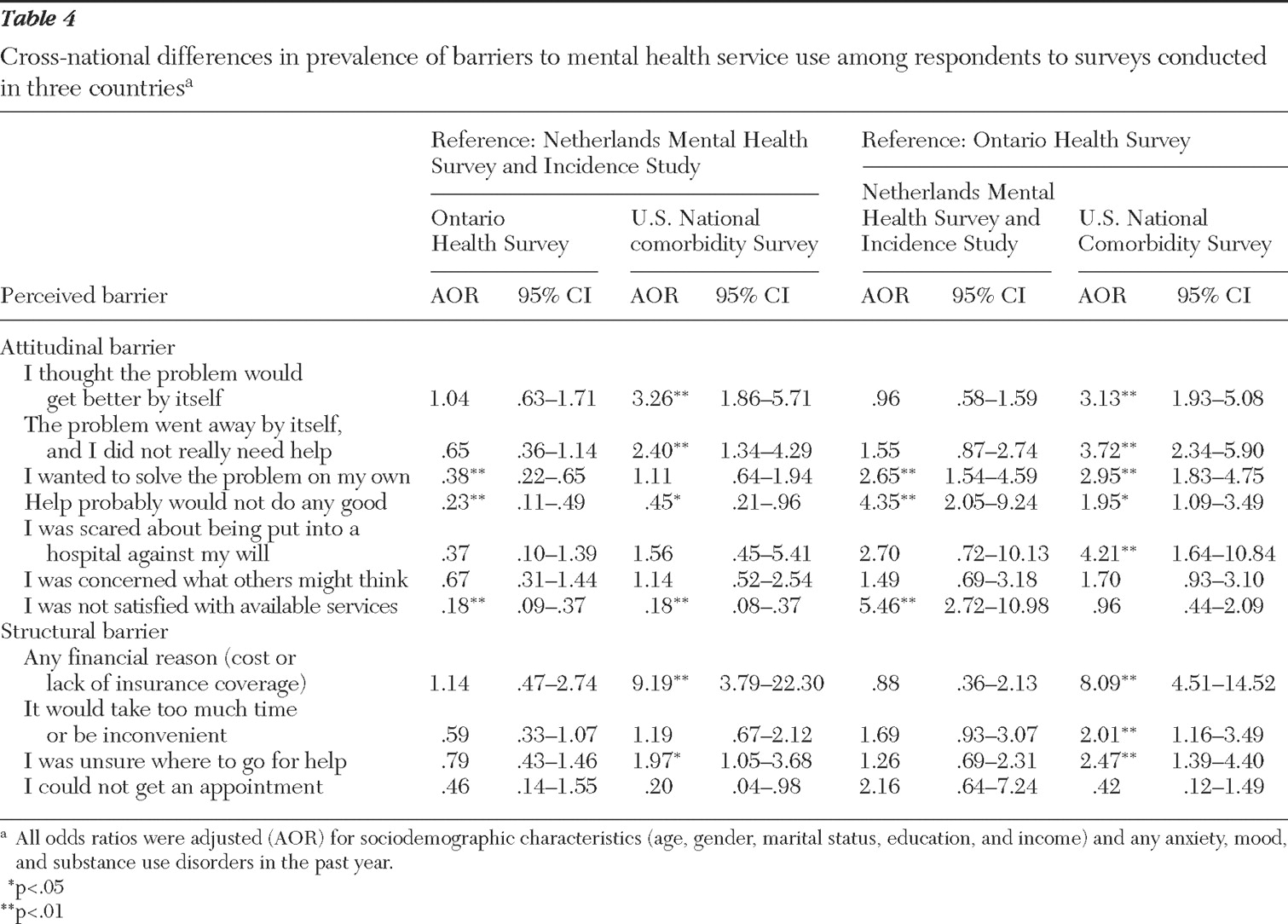
Table 4 shows that, in multivariate models, the strongest cross-national differences were financial barriers, which were much more likely to be reported in the United States than in the Netherlands or Ontario. Respondents in the United States were also much more likely than those in the other two locations to report that they wanted to solve the problem on their own, that the problem went away, and that they were "unsure where to go for help." Respondents in the Netherlands were significantly more likely than those in the United States and Ontario to report dissatisfaction with available services and that "help probably would not do any good."
In multivariate models that adjusted for country of respondent, all other sociodemographic factors, and each type of mental disorder, we found a number of significant correlates of each perceived barrier. Among sociodemographic factors, poor respondents across all sites were significantly more likely than those with above-average income to endorse that "help probably would not do any good" (adjusted odds ratio [AOR] of 5.97, CI=1.77–20.11). Increasing age of respondents was significantly associated with a lower likelihood of reporting fears of involuntary hospitalization (AOR=.90, CI=.83–.99) and concerns about embarrassment from using mental health services (AOR=.95, CI=.90–1.00). Across the three sites, the presence of a past-year mood disorder was associated with increased likelihood of endorsing a financial barrier (AOR=2.48, CI=1.03–5.98) and a fear of involuntary hospitalization (AOR=5.21, CI=1.56–17.42). Similarly, the presence of a past-year substance use disorder was associated with an increased likelihood of endorsing a financial barrier (AOR=3.16, CI=1.12–8.93), a fear of involuntary hospitalization (AOR=5.37, CI=1.37–22.07), and concerns about embarrassment from using mental health services (AOR=3.20, CI=1.20–9.08). Finally, the presence of a past-year anxiety disorder was positively associated with beliefs that "help probably would not do any good" (AOR=3.18, CI=1.27–7.95).
In multivariate models, we also tested interactions between site, level of income, and presence of each type of mental disorder—mood, anxiety, or substance use disorder—for each perceived barrier. We found only one significant site-by-income interaction (AOR=2.43, CI=1.18–4.98), such that people with low income in the United States were more likely to report a financial barrier than those with low income in Ontario or the Netherlands.
Discussion
The findings of this investigation should be interpreted in the context of the following three limitations. First, the reasons for not seeking mental health treatment in the context of a perceived need are complex issues that may be difficult for the individual to delineate in a semistructured interview. There may be a whole host of factors that the surveys did not ask about, or the exact reasons for not pursuing treatment may have been difficult for respondents to articulate. Second, data from the current United States and Ontario surveys were collected in the early 1990s. There have been significant changes to both the Canadian and the U.S. health care systems since the early 1990s, which may have ultimately led to changes in perceived barriers to mental health treatment. Third, the study examined perceived barriers across three Western countries. Findings from our work may not be generalizable to developing countries. In light of these limitations, there are several important findings.
First, the items "I wanted to solve the problem on my own" and "I thought that the problem would get better by itself" were the two most commonly endorsed barriers across the three surveys. These findings are consistent with previous data collected in the early 1980s in cities in the United States and New Zealand (
14 ) and with data from a recent survey in Chile (
15 ) and an Australian clinical sample (
12 ). However, these results are somewhat counterintuitive, because on the one hand respondents have endorsed a need for professional help and on the other report a desire to solve the problem on their own. One possible explanation is that even when individuals perceive a need for treatment, they contemplate the risks and benefits of acquiring it (
10 ). Before seeking treatment, individuals may decide to wait and see if the symptoms resolve without treatment, or they may try to solve the problem on their own (for example, with self-help books) (
46 ). Although these attitudinal barriers may reflect mild or transient distress, it is important to note that the wish to solve the problem on their own may be an important factor contributing to the long delays between onset of mental disorders and initial contact with a mental health professional (
2,
47 ).
Second, this study is the first to systematically demonstrate that low-income respondents in the United States are more likely to report a financial barrier to use of mental health services than low-income respondents in countries with fewer restrictions on accessibility to services. These findings are in contrast to Alegria and colleagues' (
16 ) work showing that the United States, Ontario, and the Netherlands did not have significant between-site differences in the relationship between income level and service utilization. However, Alegria and colleagues noted that higher income in the United States was associated with greater likelihood of specialty care service than in Ontario or the Netherlands. It is possible that the financial barriers in the United States may affect utilization of specialty mental health services specifically rather than overall mental health services.
These findings are consistent with previous work demonstrating that U.S. respondents were more likely than New Zealand respondents to report financial barriers (
14 ). However, although significant changes have occurred in the U.S. health care system since the time of data collection for the NCS, recent work from the National Health Interview Survey has found that there was an increase in the prevalence of reporting financial barriers to mental health treatment between 1997 and 2002 (
48 ). Together, these findings strongly suggest that increased accessibility to mental health services in the United States may have an impact on this unmet need, especially among the poor. However, it is noteworthy that financial barriers were also reported in a single-payer universal health care system (Ontario). These findings, together with other recent data showing that higher-income respondents are more likely to receive mental health services than lower-income individuals in Canada (
17,
18 ), suggest that increasing outreach to low-income individuals with emotional problems may be required across countries.
Third, compared with respondents in the United States and Ontario, respondents in the Netherlands were significantly more likely to report dissatisfaction with available services and that "help probably would not do any good." These findings have not been reported previously. These findings may reflect a more critical attitude toward or higher expectation of mental health services available in the Netherlands. Further replication of these findings is required in contemporary samples.
Fourth, fear of stigmatization was endorsed infrequently across the three surveys (10%–17% of those who perceived a need for mental health treatment without seeking care). These findings are inconsistent with the commonly held belief that fear of stigmatization is an important reason for not seeking treatment (
49,
50,
51 ).
Fifth, across the three countries, we found important associations between particular sociodemographic factors and types of mental disorders in relation to perceived barriers. Younger age was positively associated with fear of involuntary hospitalization and concerns about embarrassment from using mental health services. These findings imply that younger people are more likely to have such concerns, which may reflect a lack of knowledge about mental health treatment and mental illness in general. The presence of an anxiety disorder was positively associated with endorsement of the item that help probably would not do any good. These findings suggest that individuals in the community may not be aware of the treatable nature of anxiety symptoms and disorders.
It is well known that anxiety disorders often have an early age of onset and have much longer delays in receiving treatment (
52 ). We speculate that individuals with anxiety disorders might view their anxiety symptoms as untreatable parts of their personality (for example, a person with social phobia who has always viewed himself or herself as extremely shy may not be aware that treatments can reduce the symptoms of shyness) (
53 ). The presence of a past-year mood disorder and substance use disorder was positively associated with a fear of involuntary hospitalization. Individuals with mood disorders may fear involuntary hospitalization because of a personal experience of involuntary hospitalization in the past, knowing someone who was hospitalized, or a lack of awareness that most mood and substance disorders are usually treated without hospitalization.
Finally, the presence of a substance use disorder was associated with concerns of embarrassment about using mental health services. This finding is consistent with a previous study showing that the presence of an alcohol use disorder was associated with concerns of embarrassment (
54 ). It is possible that among the common mental disorders, the fear of stigmatization is more likely to be related to substance use disorders. These barriers may be due to perceptions in the community that individuals with substance use disorders have only themselves to blame and need to "pull themselves together" (
11 ).
Conclusions
Untreated mental illness is believed to be a serious burden to the health and productivity of the community. This study demonstrated that attitudinal barriers to mental health service use are more common than structural barriers across countries with differing health care systems. An important exception, however, is the finding that low-income U.S. respondents perceived greater financial barriers to access to mental health services than low-income respondents in the Netherlands or Canada.
Acknowledgments and disclosures
The National Comorbidity Survey was supported by grants R01-MH-DA-46376 and R01-MH-49098 from the National Institute of Mental Health (NIMH), a supplement to NIMH grant R01-MH-DA-46376 from the National Institute on Drug Abuse, and grant 90135190 from the W. T. Grant Foundation. The Ontario Government conducted the Ontario Health Survey. The Netherlands Mental Health Survey and Incidence Study was conducted by the Netherlands Institute of Mental Health and Addiction (Trimbos-instituut) in Utrecht. The Netherlands Ministry of Health, Welfare, and Sports provided financial support to conduct the survey. Preparation of the manuscript was supported by the Manitoba Health Research Council, by the University of Manitoba Paul Thorlakson Fund, and by grant MH-64122 from NIMH. The authors thank Tracie O. Afifi, M.Sc., for her statistical work on this study.
The authors report no competing interests.