Recent events involving violence initiated by school-age children have raised concerns about how mental health problems may be implicated (
1,
2 ). For example, the National Research Council's analysis of eight cases of lethal school violence noted that "Serious mental health problems, including schizophrenia, clinical depression, and personality disorders, surfaced after the shootings for six of the eight boys" (
3 ). Researchers also have maintained that an important risk factor for violence is untreated conduct disorder (
4,
5 ), as reflected in the high levels of untreated mental health problems among juvenile detainees (
6,
7,
8 . Finally, data on the decision to hospitalize children show a clear association with perceptions of dangerousness (
9 ).
By law and custom, parents serve as primary gatekeepers or "key recognizers" (
10 ) of children's mental health, at least until that point in adolescence when responsibility might be shared with the child. However, mental health problems often come to light only through the child's school or through social welfare or criminal justice systems. Parents may respond rather than initiate action when problems arise. Unfortunately, research also suggests that experts in these systems, as well as those in the primary care system, are not well equipped to diagnose mental health problems (
11 ). Furthermore, a dilemma unique to mental health is faced by parents who may be required to give up parental rights in order to provide children with needed services (
11 ). This unique constellation of problems faced by children, their parents, and others suggests that cultural climate may shape children's pathways to care and the understanding of the sociocultural context, and it may offer important information for clinical encounters and policy.
Arguments such as these often lead to greater societal anxiety and stigma regarding the presumed dangerousness of children with mental health problems. Although incidents of extreme school violence (such as the 1999 shootings at Columbine High School) are rare, and extant research indicates that mental illness is not a primary cause of violence among youths in the United States (
12 ), statements by some child development experts continue to raise this specter. According to Garbarino, as quoted in McFarling (
13 ), "Virtually every school in America contains boys who are troubled enough, violent enough, and righteous enough that these shootings are destined to become part of the fabric of American adolescence."
These societywide concerns raise at least four questions. First, how dangerous does the public perceive children and adolescents with mental health problems to be? Although violence is tied to criteria for some childhood mental health disorders—such as conduct disorder and oppositional defiant disorder (
14 )—a link between violence and mental health problems has been difficult to ascertain even among adults. Evidence suggests only a modest relationship between mental disorder and violence, a relationship that is largely attributable to co-occurring substance abuse (
15 ). Unfortunately, public perceptions that mental illness and violence go hand in hand may be more important than the evidence (
16,
17 18 ). Puzzling over findings that stigma associated with mental illness has increased, the Surgeon General asked why stigma is so pervasive, despite a more informed public understanding of mental illness. The answer, he concluded, appears to be rooted in a fear of violence (
19 ). We ask, How does the general public view the potential of harm to self and others among children and adolescents with mental health problems?
A second question targets the extent to which legal measures and social pressures endorse treatment for children and adolescents with mental health problems. Again, research on children is virtually absent. A recent study found that 51% of adults receiving treatment for serious mental disorders experienced some form of "leverage" into care (
20 ). Not surprisingly, then, coercion remains a "flashpoint" in mental health law (
20 ). Yet, what we know about the topic is limited. Discussions of the legality and ethics of coercion are contentious (
21,
22 ) and represent one of the longest-running controversies among mental health professionals and civil liberties groups (
23,
24,
25,
26 ). Justifications for coercion include ensuring public safety and delivery of mental health services to reluctant or noncompliant individuals believed to need treatment. Although most existing public health laws affirm the right of people with mental disorders to withhold consent for treatment, all Western countries, motivated by concerns for both society (potential harm to others) and for the individual (potential harm to self), have legislation that allows involuntary treatment (
27,
28 ).
The situation for children and adolescents is more complicated and less discussed. A clash of rights exists, pitting the rights of parents to rear children as they see fit against the rights of children to receive treatment and against the rights of the community to be protected. Forcing a child into treatment is seen by some as "a legitimate role for parents or guardians … especially in the case of school-age children, who only rarely initiate requests for help" (
29 ). Children and adolescents infrequently initiate treatment; they tend to enter services through the efforts of "gateway providers" (
10 ), including parents, teachers, and juvenile justice authorities (
30,
31 ). Regardless, Costello and colleagues' (
10 ) question remains; that is, "Under what conditions is it the mark of good parenting to consult a professional, and a cause for concern if the family cannot or will not do so?" The answer is not simple and centers on the cultural norms in both lay and professional communities. Simply stated, what does the public expect when mental health problems arise?
Third, to what extent do different subgroups in the community stigmatize persons with mental health problems? For example, it is well documented that tolerance of individuals considered to be "different" varies by the characteristics of the evaluator—for example, better educated evaluators tend to exhibit more tolerance across a range of issues, by region of residence (that is, residents of southern states are generally less tolerant than residents elsewhere), and size of place of residence (that is, urban dwellers are generally more tolerant than nonurban dwellers) (
32 ).
Fourth and finally, does the label of "mental illness" per se contribute to perceptions of dangerousness or a willingness to invoke coercive means? We hypothesized that children described as having a mental health problem (specifically, attention-deficit hyperactivity disorder [ADHD] or major depression) and those whom respondents see as having a mental illness will be more likely to be perceived as dangerous to self or others and more likely to be seen as candidates for legally coerced treatment when compared with children described as having asthma or routine problems.
Using data from the National Stigma Study-Children (NSS-C), we examined these competing questions by evaluating responses to two vignettes describing children who met
DSM-IV diagnostic criteria for ADHD and those who met criteria for major depression. As a control, two additional vignettes described children who had "daily troubles" and those who had asthma. [Vignettes are included as an online supplement to this article at ps.psychiatryonline.org.] We examined community-based beliefs on dangerousness, community norms surrounding willingness to coerce treatment, the link between the two, and the links to cultural subgroups. This research design allowed for a test of Costello and colleagues' (
10 ) claim that the threshold for initiating treatment for mental health is set higher than that for physical health problems.
Methods
Sample
Data came from the 1,152 respondents to the 2002 General Social Survey with complete data on the coercion and dangerousness items in the NSS-C module (
33 ). Of this subsample, 899 (78%) were white, 172 (15%) were African American, and 81 (7%) were of another race (such as Asian American). Respondents had a mean±SD age of 44±16.4 years. They also had 12.0±2.8 years of education and a family (household) income of $50,000±$39,490. In the analyses reported here, we used data from responses about two vignettes that described youths who met criteria for ADHD and depression or who had asthma and "daily troubles." The sample used in this analysis was self-weighting. Institutional review board approval for the General Social Survey was provided by the University of Chicago, and approval for secondary data analysis was given by Indiana University. Per standard protocol for in-person surveys, oral informed consent was secured at the time of the interviews.
Dependent variables
Respondents were asked how likely the vignette child was to be dangerous to self or others. Specifically, "How likely in your opinion is it [Name] would do something violent toward other people—is it very likely, somewhat likely, not very likely, or not at all likely?" and "How likely in your opinion is it [Name] would do something violent to [him/her]self?" Response categories were coded from 4 to 1, respectively. In all multivariate analyses (
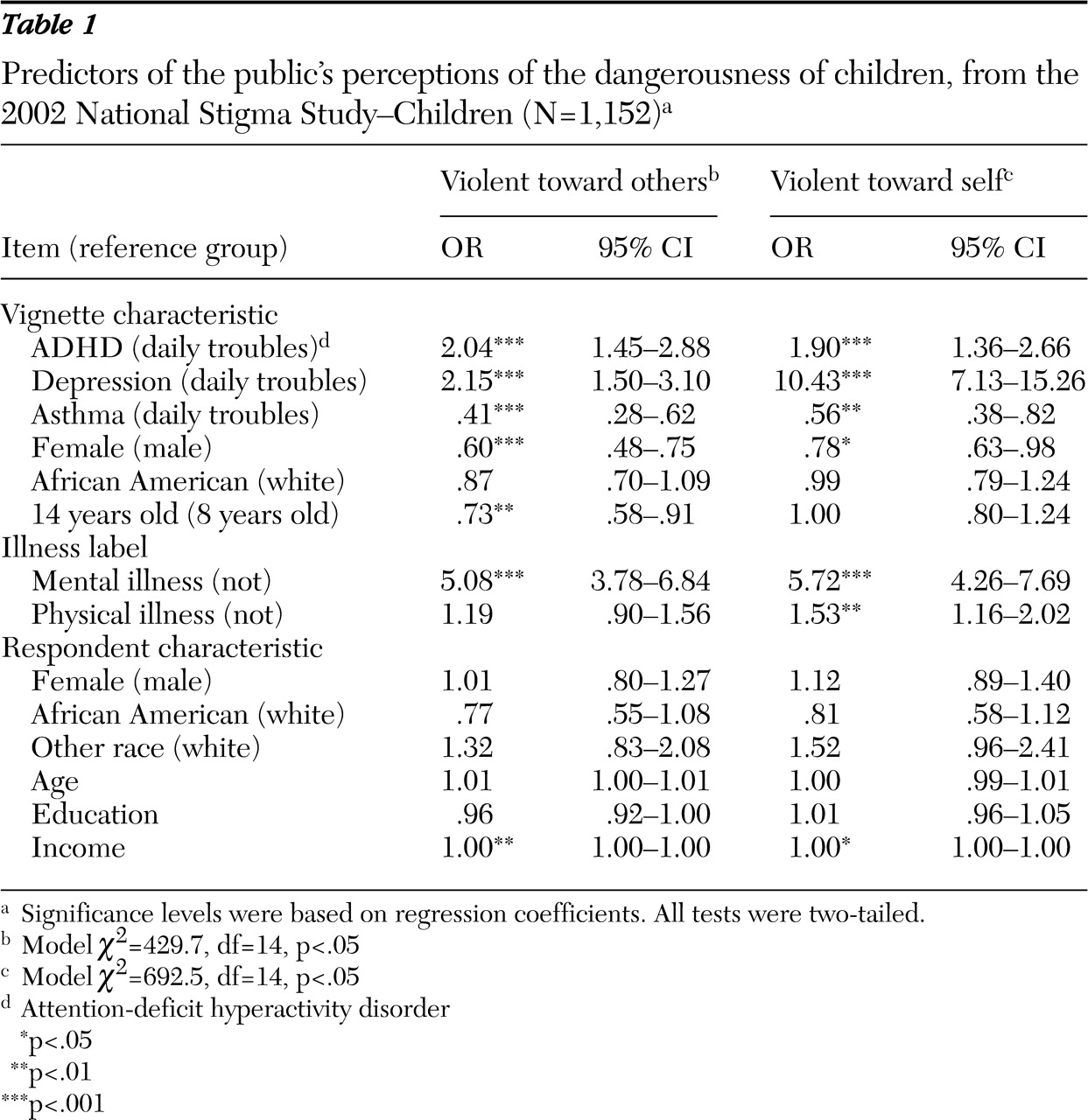
Tables 1 and
2 ), the "very likely" and "somewhat likely" responses were combined and coded 1. The "not very likely" and "not at all likely" responses were also combined and were coded 0.
Respondents were also asked, "Do you think that parents of children like [Name] should be forced by law to have [Name] treated at a clinic or by a doctor?", "…. to take a prescription medication to control [Name's] behavior?", and "… to admit [Name] to a hospital for treatment?" Response categories were yes (coded 1) and no (coded 0).
Independent variables
Vignette types were coded into a set of binary dummy variables (ADHD, depression, and asthma), with the "daily troubles" condition serving as a reference category. Three characteristics of the child described in the vignette were coded: gender (female, 1; male, 0), race (African American, 1; white, 0), and age (14 years old, 1; eight years old, 0). Respondents were also asked whether the vignette child's problem represented a mental illness, a physical illness, or both (illness labels were coded 1 for yes and 0 for no).
Five sociodemographic variables determined relevant for assessments of dangerousness or coercion by previous research (
28,
32,
35 ) were included to describe respondents: age (in years), gender (men, 1; women, 0), race (African Americans, where African Americans and respondents of other races were coded 1 and whites were coded 0), family income (annual total family or household income in tens of thousands of dollars), and education (in years).
Analyses
Bivariate and multivariate analyses assessed responses on perceived dangerousness and willingness to use coercion. Bivariate techniques (chi square analyses) were used to determine whether dangerousness and coercion varied according to the vignette child's type of problem. Estimates from ordered logistic regression models were used to examine whether children's or respondent's characteristics shaped perceptions of potential for violence. Bivariate logit regression estimated these predictors' effects on coercion. Additional analyses (not shown) were conducted with multinomial logistic models, and results were consistent. Odds ratios and 95% confidence intervals are reported, and all significance tests were two-tailed.
Results
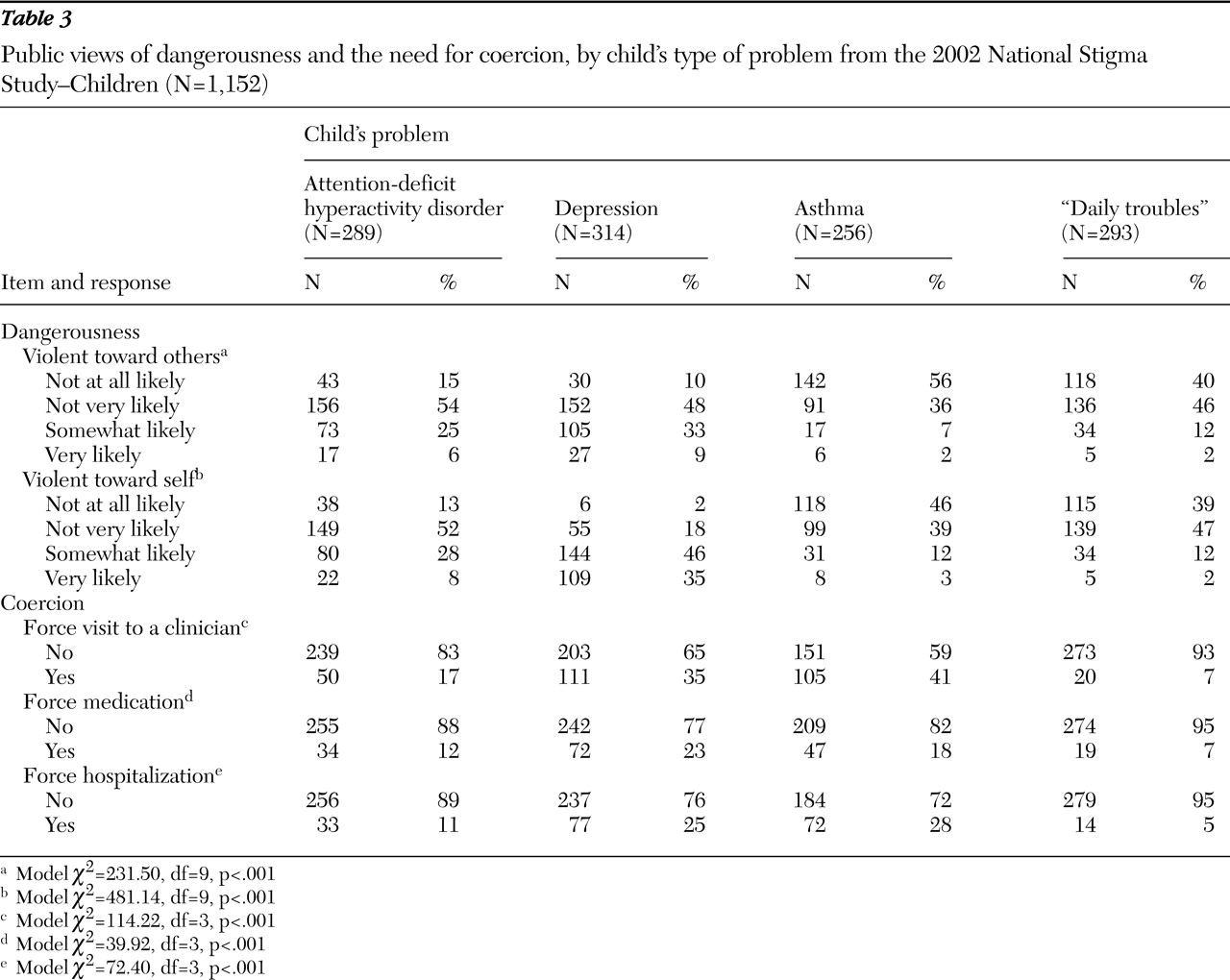
Examination of the bivariate data indicates that public perceptions of dangerousness and willingness to use coercion differed significantly by vignette type (
Table 3 ). For perceived dangerousness, significantly more respondents saw the child with ADHD or depression (versus the other children) as likely to be violent toward others (
χ 2 =231.50, df=9, p<.001). An even stronger pattern emerged regarding violence toward self, where 33% perceived the child with ADHD, and an overwhelming 81% viewed the child with depression, as at least somewhat likely to be at risk of harming him- or herself (
χ 2 =481.14, df=9, p<.001).
A somewhat different pattern emerged across coercion types. Simply stated, regardless of treatment type (visits with a clinician, medication, or hospitalization), respondents were significantly more likely to endorse forced treatment for children meeting criteria for depression or asthma. This pattern was particularly clear for forced clinical visits, where more than one-third of respondents would force a clinical visit for a depressed child, and more than 40% would force a visit for an asthmatic child ( χ 2 =114.22, df=3, p<.001). A similar pattern was shown for the willingness to force medication ( χ 2 =39.92, df=3, p<.001) and hospitalization ( χ 2 =72.40, df=3, p<.001), where respondents were also significantly more likely to invoke coercive means for the child with asthma and the child with depression.
Predictors of dangerousness
The ordered logistic regression of perceived dangerousness toward others (model 1) and toward self (model 2) indicated that the behaviors described in the vignettes were significant correlates of public responses (
Table 1 ). Respondents were most concerned with likelihood of violence among children with depression. Indeed, compared with the child with "daily troubles," the vignette child with depression was more than twice as likely to be assessed as dangerous toward others and ten times as likely to be assessed as dangerous toward himself or herself.
A similar pattern emerged in regard to children with ADHD. Compared with the child with "daily troubles," the child with ADHD was perceived as roughly twice as likely to be dangerous to others and to self. However, respondents saw children with asthma as only half as likely to be violent. Equally notable, regardless of the referent (dangerousness to self or others or both), individuals who labeled the child as having a mental illness were more than five times as likely to perceive a potential for violence.
Only a few other factors mattered, although the effects tended to be inconsistent. Respondents evaluated girls as less dangerous to self or to others. The 14-year-old was also perceived as significantly less likely than the eight-year-old to be dangerous to others. Finally, respondents with higher incomes were nominally more likely to see potential for both types of violence.
Predictors of coercion
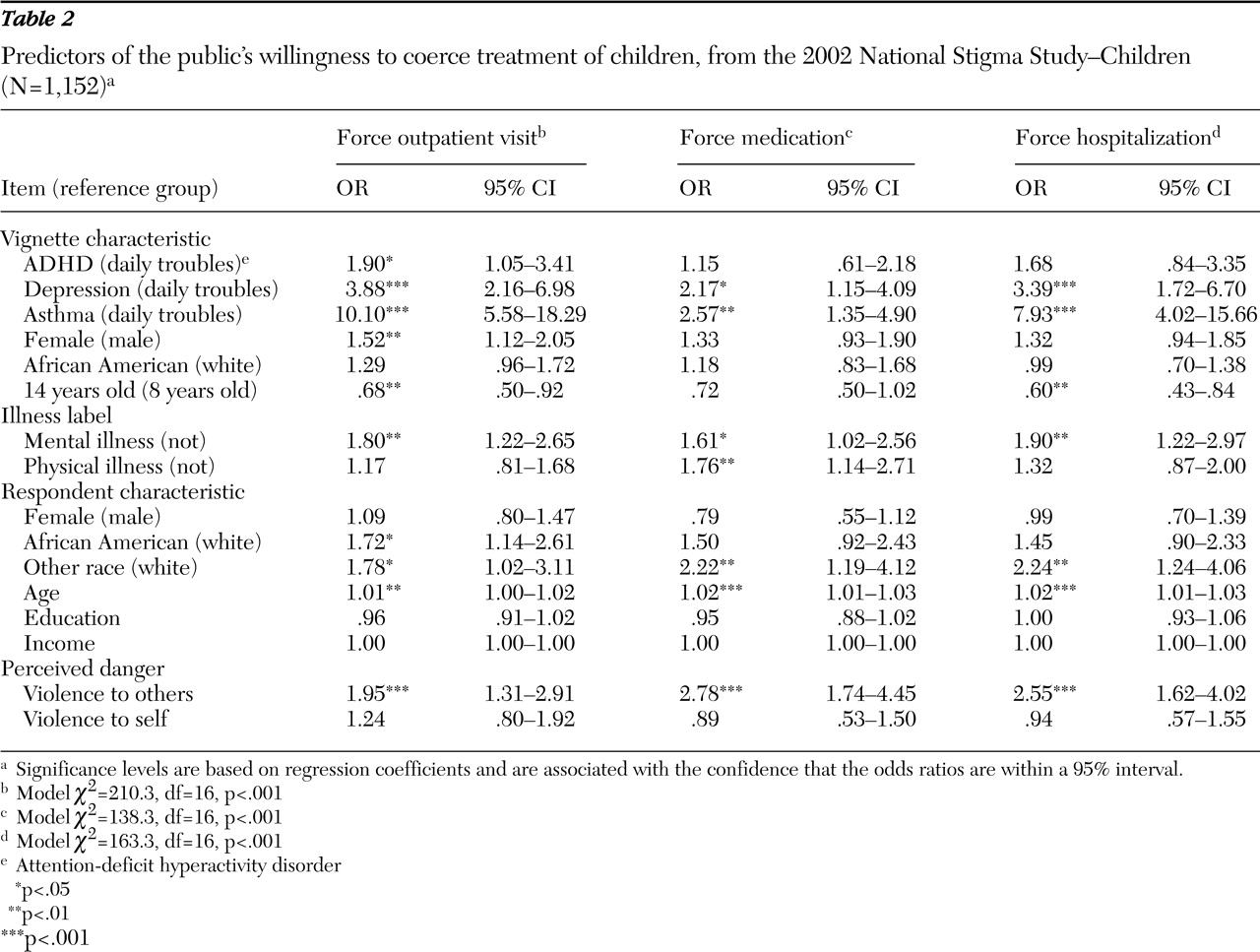
Relative to disorder types, respondents also varied in willingness to use coercive means to ensure treatment (
Table 2 ). The largest effects were observed for the child with asthma, where, compared with the child with "daily troubles," respondents were eight to ten times as likely to support coercion. Respondents were also more likely to support coercion for medication of the asthmatic child.
Respondents were also more likely to support coercion for the child with depression than for the child with "daily troubles." A somewhat different pattern emerged for the child with ADHD. Here, with the exception of a forced clinical visit, respondents were not willing to use legal means to force the child with ADHD to take medication or be admitted to a hospital.
In the case of clinical visits, respondents were more willing to use coercion for girls or for those labeled as having a mental illness. Indeed the label of mental illness significantly increased the likelihood that respondents would support coercion for clinical visits, medication, and hospitalization.
Finally, respondents were less supportive of clinical or hospital-based treatment options for the 14-year-old than for the eight-year-old. African Americans and individuals of other races were more supportive of coerced clinical visits, with the latter group more supportive of medication and hospitalization. Older respondents also were more likely to support forced treatment by clinicians, prescription medications, and hospitalization. Finally, respondents evaluating the child as more likely to be dangerous to others were roughly twice as likely to support coercive treatment.
Discussion
Informed by the contemporary climate of concern about violence in schools and a hypothesized link to mental health problems among children and adolescents, we targeted public views of the dangerousness of children and the concomitant willingness to use legal means to force children into treatment. Our results indicate that the public perceives boys and children with depression or ADHD as the groups most likely to be dangerous to self or others.
Although the findings relative to dangerousness are clear and consistent, the findings on coercion revealed some surprises in how the American public thinks about medical care for children with physical and mental disorders. Over one-third of respondents were willing to use legal means to force children with depression to visit a clinician, and even more were willing to do so for the asthmatic child. This finding suggests that more than social control and fear underlie attitudes about involuntary treatment in this country. Indeed, in the case of a physical illness such as asthma, where standard treatments are readily available, our respondents were most willing to support legal means to ensure that these children received medical care, apparently ignoring the realization that similarly well-documented standardized regimens are available for treating depression and ADHD. This finding supports Costello and colleagues' (
10 ) contention that the threshold for mental health problems may well be set higher than for physical problems.
Our findings also clearly illustrate that the stigma attached to child and adolescent mental health problems is associated with the label of mental illness. It is this condition that may be the most potent trigger for initiating treatment. Individuals labeling "the situation" as mental illness, after the analysis controlled for the behaviors described, were five times as likely to report likelihood of violence. This label, along with evaluating the vignette child as dangerous to others (but not to self), doubled the likelihood that the public would support use of coercion. Consistent with data collected from adults with mental health problems, these results continue to reflect underlying negative attitudes toward persons presumed to have mental health problems (
34 ). What also clearly emerged from these analyses was that sociodemographic characteristics did not offer powerful proxies of the cultural beliefs, values, and norms of the public.
Regarding limitations, this study asked only about legal coercion and did not explore what has been called "informal," "extra-legal," or "covert" coercion (
35,
36 ). Also it did not address reactions to possible agents of coercion (such as family, teachers or other educators, and police).
Conclusions
Analyses from the NSS-C suggest that the U.S. public stigmatizes children with mental health problems. Particularly in regard to depression, the public is likely to attribute dangerousness to youths and endorse the use of coercion into treatment. However, more than stigma is evident. More of the public supports the use of physicians, even through legal means, to ensure that children with asthma receive care. These findings highlight concern among the public regarding parents and their responsibilities.
Hannigan and Cutcliffe (
37 ) maintained that policy and legal frameworks surrounding the provision of mental health care are becoming more coercive globally. Furthermore, Anthony (
38 ) agreed that the mental health system cannot move to a recovery model under a climate of coercion. If this is the case, the need to understand public, provider, and client views of coercion and their link to perceptions of dangerousness is pressing. As Solomon (
39 ) noted, "the consequences of the competing values between preserving individual autonomy and protecting vulnerable individuals" are becoming "increasingly visible." Nowhere may this be more important than in the case of children and adolescents with mental health problems.
Acknowledgments and disclosures
The authors acknowledge project support by the National Science Foundation to the National Opinion Research Center; Eli Lilly and Company; the Office of the Vice President for Research, Indiana University; and grant K02-MH-012989 from the National Institutes of Health and National Institute of Mental Health to Dr. Pescosolido, principal investigator. The authors thank Tom Smith and staff members of the Indiana Consortium for Mental Health Services Research, Schuessler Institute for Social Research, Indiana University.
The authors report no competing interests.