Data published over the past two decades suggest that comorbidity is common among persons with bipolar disorder. In both epidemiological and clinical samples the comorbid conditions most often observed with bipolar disorder are alcohol and drug abuse or dependence followed by anxiety disorders (
1,
2,
3 ). Of the anxiety disorders, posttraumatic stress disorder (PTSD) is estimated to be prevalent in 7% to 40% of persons with bipolar disorder (
2,
3,
4,
5,
6,
7,
8 ), compared with 7.8% in the general population (
2 ). However, relatively few studies have examined the impact of comorbid PTSD on the outcome of patients with bipolar illness.
Emerging evidence suggests that comorbid PTSD adversely affects the course of bipolar disorder (
4,
5,
6,
7,
8,
9 ). For instance, Simon and colleagues (
4 ) established that patients with comorbid bipolar disorder and PTSD had shorter euthymic periods and a higher frequency of suicide attempts. Sajatovic and colleagues (
5 ) found that older veterans with comorbid bipolar disorder and PTSD generally utilized outpatient psychiatric and nonpsychiatric services more frequently than their counterparts with bipolar disorder alone.
The primary aim of this study was to test the hypothesis that nongeriatric patients with comorbid bipolar disorder and PTSD have more severe psychopathology and utilize health services more frequently than those with bipolar disorder or PTSD alone. This was accomplished by retrospectively reviewing the charts of 139 individuals with bipolar disorder, PTSD, and both conditions. The study was designed to compare the demographic and clinical characteristics and the service use patterns of the three groups.
Methods
Patients were identified via a search of the Department of Veterans Affairs Salt Lake City Health Care System's (VASLC's) electronic medical records for ICD-9 codes indicating bipolar disorder, PTSD, or comorbid bipolar disorder and PTSD. The medical records were reviewed by the investigators to confirm the diagnosis of bipolar disorder (type I or type II), PTSD, or both. The study was approved by the institutional review board of the University of Utah and the VASLC Health Care System Research and Development Committee. Patients were included in the data analysis if they were male, were aged 18 to 65 years, and had received two years of continuous treatment between 2000 and 2005. Patients with comorbid psychiatric conditions were included with the following exceptions: schizophrenia, schizoaffective disorder, or substance-induced mood disorder. Patients who received treatment from the mental health intensive case management team were excluded.
The following data were collected by review of the identified medical records: age, race, marital status, and service-connected disability; type of PTSD criterion A trauma attributed as the etiology of PTSD; the presence of a history of alcohol or drug abuse or dependence; the number of comorbid medical disorders; and the total number and type of medication prescriptions during two years of treatment. Illness severity during the two years of treatment was retrospectively determined at four-month intervals by using the Clinical Global Impression-Severity Scale (CGI-S). Health service use was assessed by measuring the number of primary care visits, mental health prescriber visits, psychotherapist visits, substance abuse treatment visits, psychiatric emergency department visits, medical emergency department visits, psychiatric hospitalizations, and medical hospitalizations throughout the two years of treatment.
Analysis of variance, the chi square test, and Fisher's exact probability test were used to examine differences in demographic, clinical, and course-of-illness variables between patients diagnosed as having bipolar disorder, PTSD, or comorbid bipolar disorder and PTSD. Analysis of covariance was used to control for the presence or absence of a substance use disorder in comparing mean CGI-S scores. Multivariate analysis of variance was used to control for the presence or absence of a substance use disorder in comparing the proportion of patients requiring inpatient psychiatric hospitalization. [A longer methods section and additional references are available as an online supplement at ps.psychiatryonline.org.]
Results
Our study was designed a priori to compare the demographic and clinical characteristics and the service use patterns of the first 50 patients satisfying all of our inclusion and exclusion criteria in each subgroup. By using our exclusion criteria, our final sample of 139 male veterans consisted of 49 patients with bipolar disorder, 49 patients with PTSD, and 41 patients with comorbid bipolar disorder and PTSD.
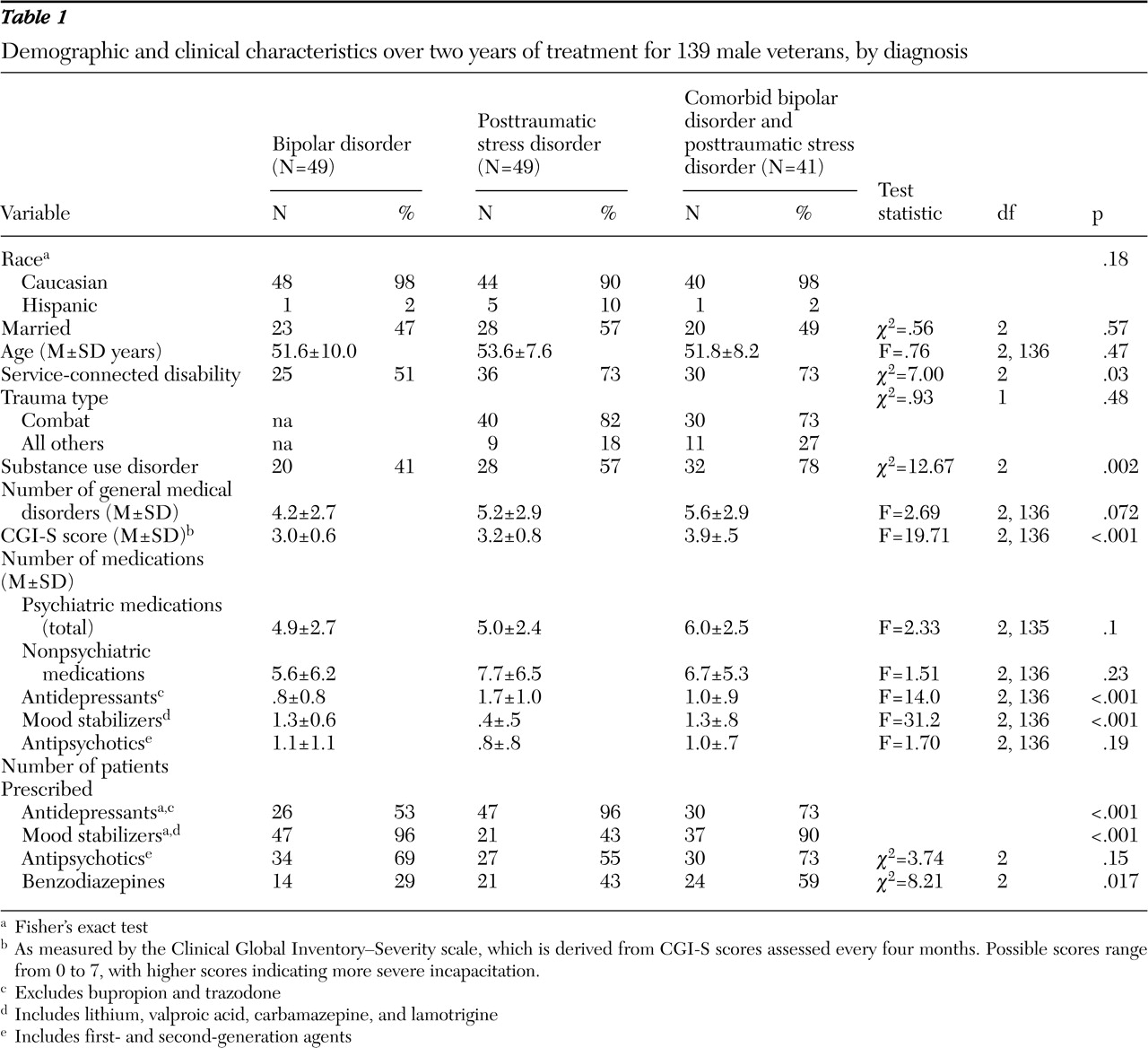
Demographic and clinical characteristics are presented in
Table 1 . The group with comorbid bipolar disorder and PTSD was significantly more likely to have a history of a substance use disorder compared with the other two groups (p=.002). The group with comorbid bipolar disorder and PTSD had significantly higher mean CGI-S scores compared with the other two groups (3.9 compared with 3.0 in the bipolar disorder group and 3.2 in the PTSD group; p<.001). This association remained significant after the analysis controlled for the presence of a comorbid substance use disorder (p<.001).
The group with PTSD was prescribed a larger mean number of antidepressants and fewer mood stabilizers (p<.001 in both cases) than the group with bipolar disorder or the group with both conditions. Patients with bipolar disorder or both conditions were significantly more likely than those with PTSD to have received a prescription for a mood stabilizer (96% and 90%, respectively, compared with 43% in the PTSD group; p<.001), but these groups were significantly less likely to have received a prescription for an antidepressant (53% and 73%, respectively, compared with 96% in the PTSD group; p<.001). Patients with PTSD or both conditions were significantly more likely to have received a prescription for a benzodiazepine (43% and 59%, respectively, compared with 29% in the bipolar disorder group; p=.017).
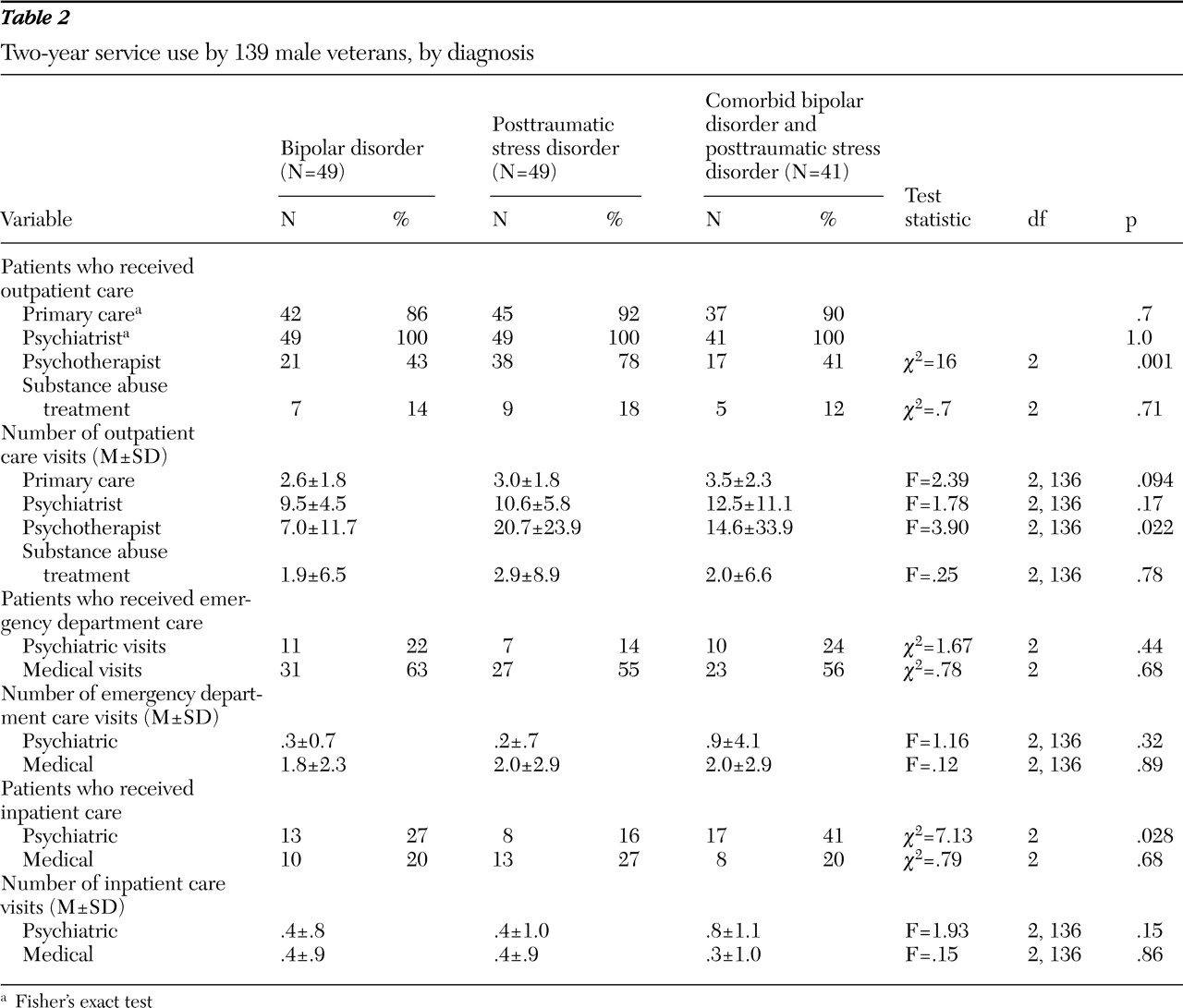
Health service utilization is presented in
Table 2 . The PTSD group had a significantly larger mean number of psychotherapy visits compared with the other two groups (20.7 compared with 7.0 in the bipolar disorder group and 14.6 in the group with both conditions; p=.022). A significantly smaller proportion of patients in the bipolar disorder group and the group with comorbid bipolar disorder and PTSD received psychotherapy compared with the group with PTSD (43% and 41%, respectively, compared with 78% in the group with PTSD; p=.001). Notably, patients with both conditions were significantly more likely to require inpatient psychiatric hospitalization than those with either disorder in isolation (p=.028), but this association was not statistically significant (p=.063) after the analysis controlled for the presence of a comorbid substance use disorder.
As presented in
Tables 1 and
2, there were no significant between-group differences in age, race, marital status, the mean number of general medical conditions, the mean total number of psychiatric medications prescribed, the mean total number of nonpsychiatric medications prescribed, the mean number of antipsychotics prescribed, the proportion of patients who received antipsychotic prescriptions, the proportion of patients who had primary care visits, and the mean number of primary care visits, psychiatrist visits, substance abuse treatment visits, psychiatric emergency department visits, medical emergency department visits, medical hospitalizations, trauma, and medical inpatient care.
Discussion
The aim of the study presented here was to increase our understanding of the clinical characteristics and health service utilization of patients with comorbid bipolar disorder and PTSD. Published reports estimate that 7% to 40% of persons with bipolar disorder have comorbid PTSD (
2,
3,
4,
5,
6,
7,
8 ). Our finding that 38% of patients in our bipolar disorder sample had comorbid PTSD may in part be due to the increased prevalence of PTSD in the veteran population compared with that of the general population (
10 ). Nonetheless, taken together with other reports, our finding suggests that comorbid bipolar disorder and PTSD is relatively common. This is likely to be especially critical in veteran populations.
We hypothesized that patients with both conditions would generally have worse outcomes than those with either condition alone. As others have observed (
4,
7 ), we found a significant increase in illness severity among those with both conditions (CGI-S score of 3.9 compared with 3.0 in the group with bipolar disorder alone). Although direct comparison to previous observations (
4,
7 ) is precluded because of the use of different psychometric tools, our results provide further support that comorbid PTSD increases the illness severity of bipolar disorder. In our sample, the population with both conditions exhibited a significantly higher prevalence of substance abuse or dependence that mirrors the findings of others (
4,
11 ). Many reports suggest that substance use disorders negatively impact the course of bipolar disorder, including increased suicidality (
12 ) and decreased time spent in remission (
13 ). Thus it would not be unreasonable to attribute the observed adverse outcomes in the group with comorbid bipolar disorder and PTSD as secondary to the increased prevalence of comorbid substance use disorders. However, regression analyses controlling for the presence of comorbid substance use disorders revealed significant independent effects of PTSD on bipolar disorder outcomes. Thus, as was also observed in the study by Simon and colleagues (
4 ), the increase in illness severity observed in comorbid bipolar disorder and PTSD was only partially mediated by the presence of a substance use disorder.
Our sample closely resembled that of Sajatovic and colleagues (
5 ), who compared service utilization among geriatric patients with bipolar disorder and those with comorbid bipolar disorder and PTSD, in regard to the mean number of outpatient mental health care visits. Patients with bipolar disorder in our sample had a mean of 18.4 mental health care visits over two years (compared with 17.0 in the study by Sajatovic and colleagues). Patients with comorbid bipolar disorder and PTSD had a mean of 29.1 mental health care visits over two years (compared with 33.1 in the study by Sajatovic and colleagues). However, in contrast to the findings of Sajatovic and colleagues (
5 ), who found no substantial difference in the proportion of geriatric patients with comorbid bipolar disorder and PTSD who were hospitalized, we found an increase in the proportion of patients requiring inpatient psychiatric treatment in the group with comorbid bipolar disorder and PTSD. After the analysis controlled for substance abuse or dependence, this difference lost statistical significance, thereby suggesting that substance use disorders largely mediated the observed increase in inpatient psychiatric care. Comorbid substance use disorders may thus represent modifiable risk factors that if properly treated could potentially mitigate the disease burden of those with comorbid bipolar disorder and PTSD.
Contrary to our expectations, there were no significant differences between the groups in the utilization of most types of outpatient psychiatric and nonpsychiatric services, the sole exception being the use of psychotherapy. Given the much higher prevalence of substance use disorders in our group with comorbid bipolar disorder and PTSD, our findings are consistent with those of Verduin and colleagues (
12 ), who observed no between-group differences in the mean number of outpatient primary care visits, medical specialist visits, and emergency care visits in a sample of veterans with bipolar disorder with and without comorbid substance use disorders. These findings could relate to factors specific to the Department of Veterans Affairs health care system. For example, it is conceivable that all groups receive more treatment than they might in other settings. Further research will be needed to clarify this issue.
With the exception of the study by Simon and colleagues (
14 )—which found no significant difference between bipolar disorder and comorbid bipolar disorder and PTSD in "anxiety treatment adequacy"—this is, to the best of our knowledge, the first report of medication use patterns specific to comorbid bipolar disorder and PTSD. Our analysis of medication use patterns revealed that the group with comorbid bipolar disorder and PTSD mirrored the bipolar disorder group in regard to use of mood stabilizers, antipsychotics, and antidepressants. Taken together with our finding that the proportion of patients with bipolar disorder and those with comorbid bipolar disorder and PTSD who received psychotherapy was significantly smaller than that of patients with PTSD, it appears that a diagnosis of bipolar disorder may in fact deter the use of potentially efficacious pharmacotherapies and psychotherapies. Indeed, experts in the management of PTSD recommend a combination of psychotherapy and psychopharmacology for the treatment of refractory PTSD (
15 ). As noted above, significantly fewer patients in the comorbid group had received psychotherapy. Moreover, significantly fewer patients in the comorbid group than in the group with PTSD had received treatment with an antidepressant. Although the latter finding is likely due to the concern of inducing mania with antidepressant use among patients with bipolar disorder, it is not unreasonable to hypothesize, as previously done by Simon and colleagues (
4 ), that the increased severity of illness observed among those with comorbid bipolar and anxiety disorders may in part be due to undertreatment of the comorbid anxiety disorder.
Our results must be interpreted with caution because of the limitations inherent in the design of the study. Because this was a retrospective chart review, it was not possible to completely ascertain the reliability of diagnoses. However, charts were carefully reviewed in regard to substantiation of diagnoses and only those for which there was compelling evidence (specific documentation of symptoms that met DSM-IV-TR criteria) were included. Moreover, illness severity estimates (as measured by the CGI-S) relied solely on information available in the existing medical record. All patients were veterans, all patients were male, and most had combat-related PTSD, which may limit the generalizability of results to civilian populations. Furthermore, because all patients had received two years of continuous treatment, our results may be generalizable only to persons who consistently seek treatment. However, this exclusion criterion eliminated only about one-quarter of our study population, and thus our findings should be widely generalizable to the veteran population.
Despite these limitations, our results confirm and extend existing reports that patients with comorbid bipolar disorder and PTSD generally have a more severe course of bipolar illness than those with bipolar disorder alone. Moreover, to our knowledge this is the first study to report specifically about patterns of psychiatric treatment use and utilization of outpatient, emergency, and inpatient services among nongeriatric patients with comorbid bipolar disorder and PTSD. Taken together, our findings suggest that persons involved in the administration and delivery of mental health treatment to patients with comorbid bipolar disorder and PTSD should attend carefully to several issues. First, given its greater prevalence and association with increased inpatient psychiatric service utilization, special care should be given to the identification of substance use disorders and diversion into chemical dependence treatment. Second, given their proven efficacy in the treatment of PTSD and our finding that they are underutilized in our comorbid sample, careful attention should be given to the judicious use of outpatient psychotherapy and antidepressant pharmacotherapy.