The development of cognitive-behavioral therapy (CBT) for the treatment of anxiety has resulted in diagnostically specific protocols for each of the six anxiety disorders—panic disorder, with or without agoraphobia; obsessive-compulsive disorder (OCD); social phobia; generalized anxiety disorder; specific phobia; and posttraumatic stress disorder (PTSD). Although each of these clinical strategies is potent, few mental health clinics have the resources to offer six different treatment strategies. Recently, we have considered a format more suited to many clinical services—that is, a protocol based on standard CBT techniques to treat patients with different anxiety disorders in a single group. This article describes a randomized controlled trial of a single CBT group for patients with various anxiety disorders.
Conceptually, several considerations point to combining patients with different anxiety disorders into a single treatment group. The first is common content. Most diagnosis-specific protocols, for example, teach about anxiety and its physiology, provide a rationale for graded exposure exercises, and teach cognitive restructuring. Diagnosis-specific content—for example, interoceptive exposure for panic disorder or cognitive challenges to the fear of negative evaluation for social anxiety—is present in most protocols, but such content is covered in a minority of sessions.
A second rationale for a mixed-diagnosis CBT group is related to the fact that many individuals have more than one anxiety disorder. Evidence from both clinical (
1 ) and epidemiological (
2 ) samples indicates that people are as likely to have multiple anxiety disorders as to have one. Thus the skills aimed at treating multiple anxiety disorders of the same patient may be taught concurrently in a single group.
Recently, some investigators have returned to the concept of a single underlying negative-affect syndrome underlying unipolar depression and many anxiety disorders (
3 ). Others have proposed a tripartite model (
4 ), which identifies three common components of anxiety and depression. To the extent that common processes are present across anxiety disorders, a pandiagnostic treatment strategy may be warranted.
A fourth consideration is related to potential clinical efficiencies gained from a group format. With patients who have generalized anxiety disorder (
5,
6 ) and those who have panic disorder (
7,
8 ), for example, CBT has been offered equally often in individual and group formats and has resulted in similar effect sizes. Moreover, for social phobia, the group format is not only as effective as the individual format, it costs half as much (
9 ).
Finally, an array of diagnosis-specific groups is simply not possible in some clinical services. Many general mental health clinics do not have eight to 12 patients with the same anxiety diagnosis who all need services and who are all available at the same time for a group. Assembling a cohort of diagnostically similar clients is a lengthy process in many clinics, which compromises the availability of timely service and may even produce unethical delays. Similarly, many clinics cannot devote resources to providing individual-format diagnosis-specific CBT. Conversely, most clinics would have little difficulty assembling patients with various anxiety disorders for a heterogeneous group—if such a strategy was effective.
To offer such a novel group format clinicians and administrators would wish to see substantial effect sizes, whether or not they are equivalent to those derived from diagnostically homogeneous strategies. Effect sizes from diagnosis-specific CBT for anxiety disorders are of large to very large magnitude (
10 ). They range from an average effect size for social phobia of .84 (
9 ), to 1.3 for panic disorder (
8 ) and PTSD (
11 ), and to 1.7 for generalized anxiety disorder (
6 ).
In the limited literature describing diagnostically heterogeneous CBT groups for patients with anxiety disorders, the effect sizes reported are generally in the medium-to-large range. Two uncontrolled studies described immediate and enduring reductions in both self-reported anxiety symptoms (
12,
13 ) and behavioral avoidance (
12 ). A third pandiagnostic group CBT strategy (
14 ) used a randomized controlled design with a small sample and found that clinician ratings of anxiety severity and the proportion of patients meeting criteria for an anxiety disorder were significantly reduced. Posttreatment effect sizes were large to very large (d=.75 to 1.50).
The study reported here is the first to employ an effectiveness paradigm to assess the immediate and enduring effects of the mixed-diagnosis group strategy for patients with anxiety disorders. We used a blocked, randomized wait-list controlled design. We had two primary hypotheses—first, that between-group analyses based on a randomized design would reveal greater reductions in anxiety among the immediate-treatment group than among the wait-list control group, as assessed with a pandiagnostic measure of anxiety, and second, that within-group analyses would reveal immediate and enduring reductions in anxiety severity, as assessed with the pandiagnostic measure.
Methods
This effectiveness study was based on a randomized, wait-list-control research design implemented at three sites. Consistent with the effectiveness paradigm, broad inclusion and narrow exclusion criteria were used to emulate the patient-centered clinical mandate of many mental health services. The study was approved by the University of British Columbia Behavioural Research Ethics Board and conducted between January 2003 and January 2005.
Sample
The participants were drawn from three outpatient services in Vancouver, British Columbia: two were in large teaching hospitals, and the third was a training clinic at an academic department of psychology. Clinically, this approach provided a broad range of clients—from those with a single moderate anxiety problem who had good social and occupational functioning to severely distressed clients with multiple comorbid conditions whose functioning was both troubled and troublesome.
Consistent with the effectiveness paradigm, the sole inclusion criterion was the presence of a current anxiety disorder: panic disorder with or without agoraphobia, OCD, social phobia, generalized anxiety disorder, specific phobia, or PTSD. Patients with a residual diagnosis, such as anxiety disorder not otherwise specified, were not included. The exclusion criteria were also minimal: active substance abuse or dependence or psychosis. There were no limitations on past or concurrent treatments.
Procedure
Upon receipt of the referral, all potential participants were contacted for a ten-minute telephone screen. A total of 281 referrals were received. A significant number of referred patients (N=96) did not return our calls, indicated that the group would not be convenient, or stated they did not have significant anxiety.
When the screen indicated significant anxiety, we scheduled an intake diagnostic interview. At the interview we reviewed the content of the group and the wait-list-control nature of the study, and we obtained written consent. A total of 185 patients then participated in a structured diagnostic interview—the Structured Clinical Interview for DSM-IV (SCID-IV) (
15 ). Of these, 156 patients received a principal diagnosis of an anxiety disorder. The others received a diagnosis of anxiety disorder not otherwise specified and thus were not eligible to participate. None were ineligible because of exclusion criteria. Four eligible patients withdrew before randomization, leaving a final sample of 152. Together, these procedures ensured that all referrals received in the three clinics during the trial period were considered.
When approximately 24 participants had completed the diagnostic assessment, they were grouped by diagnosis and then stratified by scores on the Global Assessment of Functioning (GAF) (
15 ). For example, when four patients with panic disorder had been identified, they were divided into higher- and lower-GAF pairs, and one from each pair was randomly assigned to the immediate- and delayed-treatment conditions. Thus diagnostically heterogeneous but equivalent groups were created.
After receiving a diagnosis, participants attended a group assessment session where they completed baseline, or time 1 (T1), measures of symptom severity. They were then informed of their assignment to either the immediate-treatment or delayed-treatment condition. Those in the former condition began the 11-week group the following week. All returned for a second group assessment session, which was held concurrent with the end of the first group cycle at time 2 (T2). The delayed-treatment participants began the group one week after the T2 assessment session and later completed a third set of questionnaires on completion of the group (T3). All participants completed a similar set of measures six months after completion of treatment (T4).
Six participants randomly assigned to the delayed-treatment group withdrew from the study between baseline (T1) and the start of their group (T2). Anticipating this attrition, we had assessed a small number of patients who could serve as replacements. Thus 79 participants were in the delayed-treatment condition, and 73 were in the immediate-treatment condition.
Treatment
The treatment consisted of 11 weekly two-hour sessions with two group leaders. Each treatment group included nine to 13 participants. At each site a senior doctoral-level psychologist (DHE, ASJ, and KT) served as the senior group leader and was assisted by a senior graduate student in clinical psychology. The content of the group sessions, summarized in the box on this page, was designed to include most common CBT elements, as well as many disorder-specific treatment elements. In general, the behavioral components were prominent in the first half of the protocol. In the second half, starting with the sixth session, the cognitive elements were prominent. All patients made a commitment to engage in daily homework tasks, all of which were recorded in a homework log and discussed in each session.
Measures
The selection of measures was guided by the "gold standard" principle—that is, measures chosen are conceptually sound, have good psychometric properties, and are widely used. The SCID-IV was used to determine the principal anxiety disorder as well as concurrent anxiety and mood disorders. Estimates of interrater reliability in diagnoses resulted in a kappa of .80.
Because we wished to assess anxiety severity in a manner that would allow comparisons of the magnitude of change between as well as within diagnostic groups, we chose the Beck Anxiety Inventory (BAI) (
16 ) as a pandiagnostic measure of anxiety severity. The BAI was administered at three assessment points for the immediate-treatment group and four assessment points for the delayed-treatment group.
To better characterize the samples at baseline, we also assessed several other features related to symptom severity. To gauge current depressive symptoms, we asked participants to complete the Beck Depression Inventory II (
17 ). The Anxiety Sensitivity Index (
18 ) was used to assess participants' fear of the physical sensations of anxiety states. Their adaptive functioning was rated in the initial diagnostic interview by using the GAF (
15 ). Data were analyzed with SPSS version 13.
Results
Results describing within- and between-group changes in symptom severity are presented below. First, however, we present data related to baseline status, which allow a characterization of the sample and an assessment of the adequacy of the matching and randomization procedures.
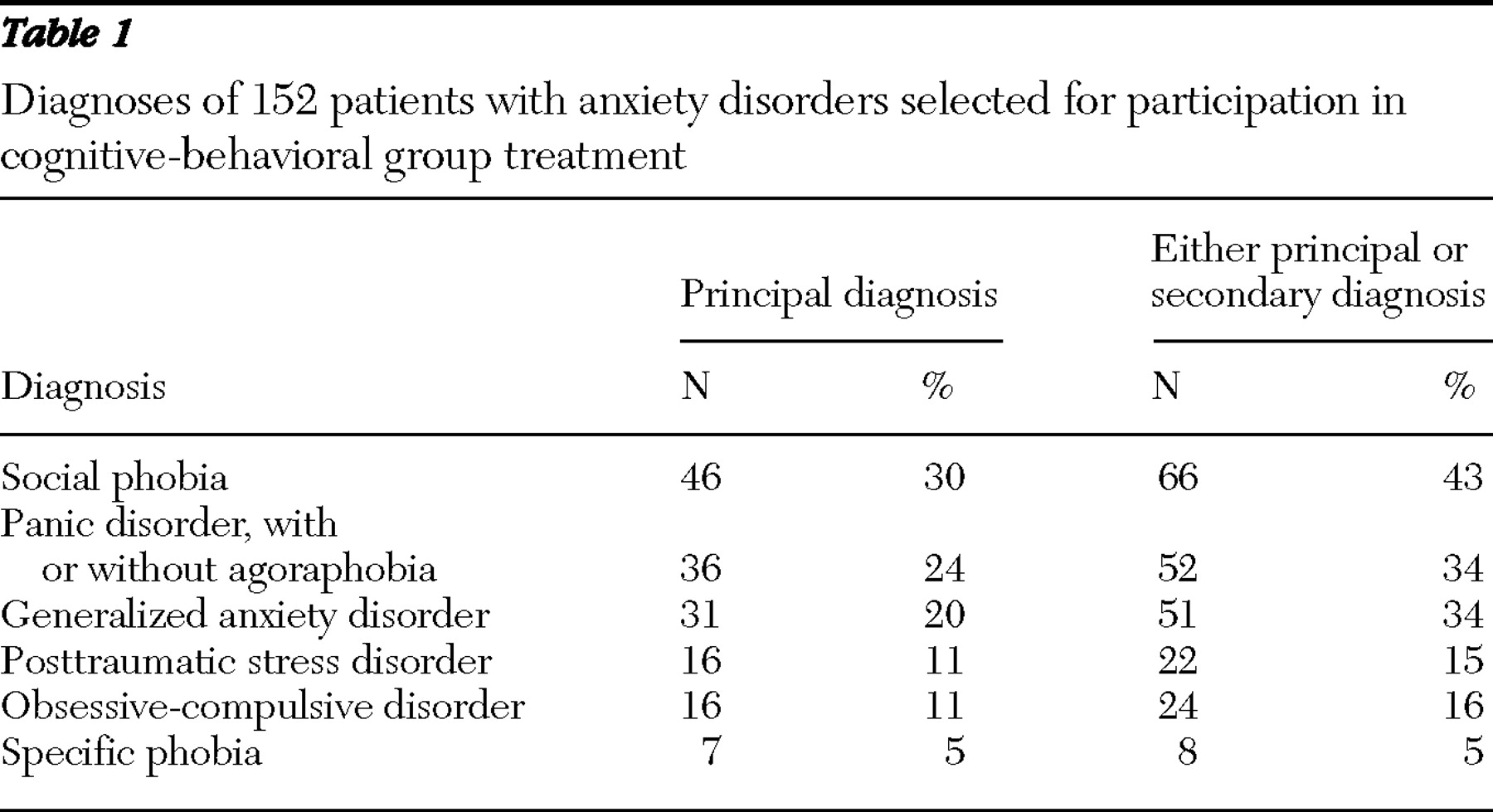
As shown in
Table 1, the sample met the objective of diagnostic heterogeneity. The original plan called for 24 patients with each of the six principal diagnoses. The data in
Table 1 indicate that five of the six anxiety diagnoses were well represented in the sample. Only specific phobia was underrepresented.
Comorbidity was common: 66 of the 152 participants (43%) had more than one current anxiety diagnosis. The proportion of patients who had multiple anxiety disorders ranged from 65% (N=20) of those with a principal diagnosis of generalized anxiety disorder, to 14% (N=1) of those with a primary diagnosis of specific phobia.
Table 1 shows the number of participants with primary diagnoses and the number who met criteria for any of the six diagnoses, whether primary or secondary.
Concurrent diagnoses outside the anxiety spectrum were also common. Thirty-one (20%) met criteria for a current major depressive episode, and 46 (30%) met criteria for lifetime major depressive disorder. In addition, ten participants (7%) met criteria for past substance use disorders.
Sample description
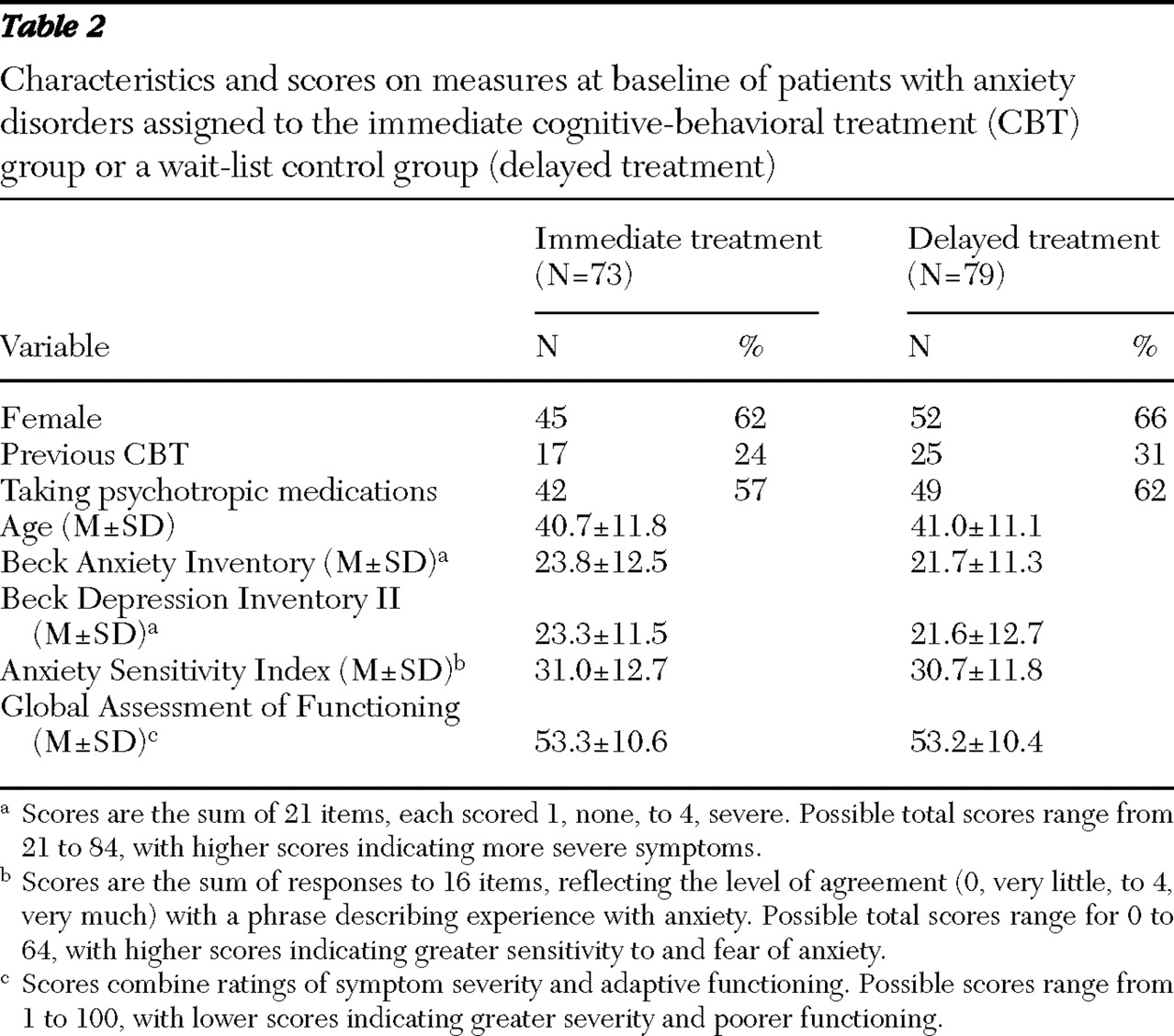
Demographic data shown in
Table 2 indicate a profile commonly seen in populations of patients with anxiety disorders: two-thirds were women, there was a wide age range (19–70 years), and many were taking medications (usually selective serotonin reuptake inhibitors). Twenty-eight percent stated they had previously received CBT for anxiety. Data regarding cultural or racial origin were not collected.
Symptom severity data at baseline show a troubled clientele. As shown in
Table 2, across all diagnostic categories, patients' anxiety as reported on the BAI was on average in the moderately severe range. Thirty-eight patients (25%) had GAF scores less than 49, indicating severe symptoms or severe impairment. The randomization did not yield significant group differences in several measures of baseline symptom severity, as measured by multivariate analysis of variance.
Attrition was similar to that seen in many clinical settings, although it was greater than attrition in other effectiveness studies (
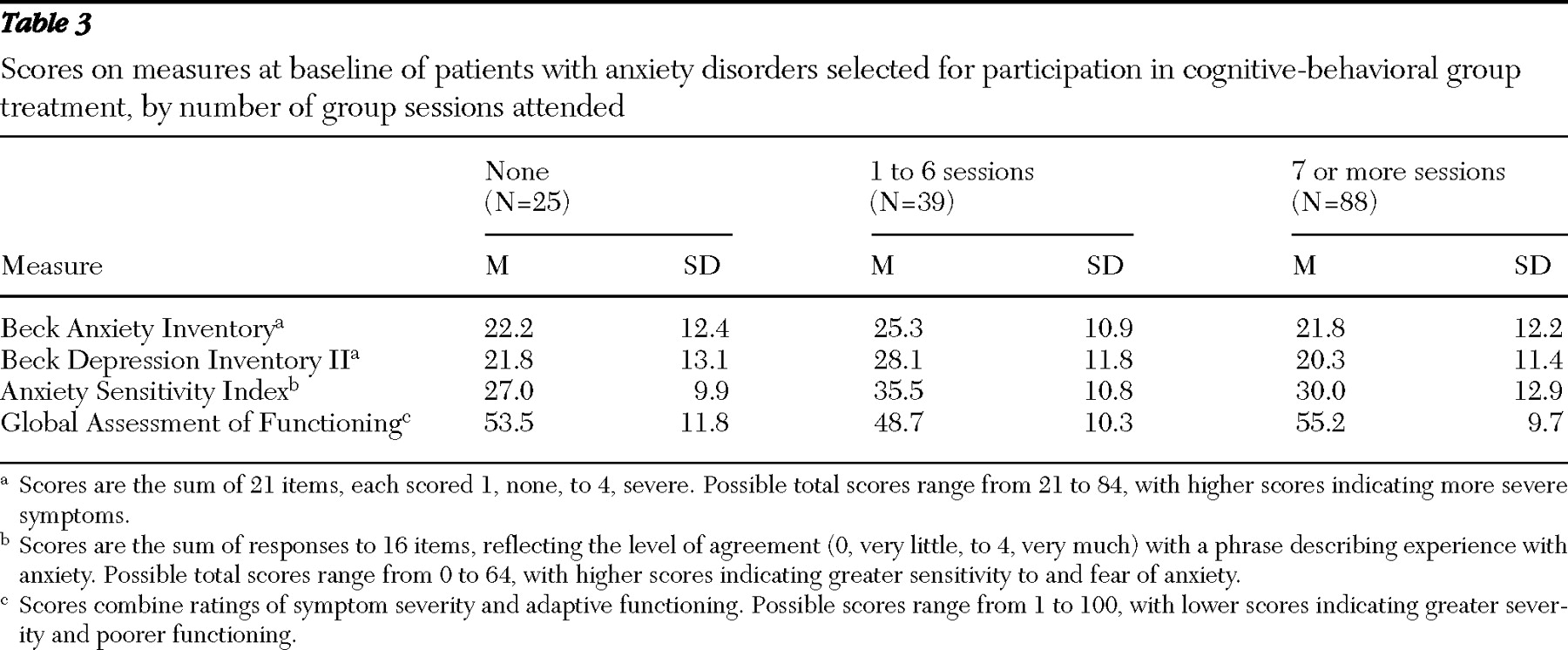
7 ). A total of 25 participants (16%) did not attend any sessions, despite having attended the baseline questionnaire session. Of those who did attend at least once, 39 (26%) dropped out—that is, they attended six sessions or fewer. A total of 88 participants completed the group—that is, they attended seven or more sessions (69% of those who attended at least once and 58% of the 152 participants at baseline).
Significant group differences were found in completion rates. A comparison of the three categories (never attended, dropped out, and completed) indicated that the proportion of those never attending was significantly larger in the delayed-treatment group than in the immediate-treatment group (20 participants, or 25%, compared with five participants, or 7%). However, the proportion of participants who dropped out after attending at least one session was similar in the two groups (25 participants, or 31%, in the immediate-treatment group, and 19 participants, or 26%, in the delayed-treatment group).
Those who started the group but then dropped out had more severe symptoms and lower levels of functioning than those who completed or did not attend. A multivariate comparison of the baseline severity measures in
Table 3 found significant differences between the groups (F=2.38, df=8 and 174, p=.02). It is notable that those who dropped out were comparable in terms of anxiety severity but had higher levels of depressive symptoms and lower functioning (p<.05) than those who never attended or who completed the groups.
Implementation
We assessed fidelity of implementation in two ways. First, we assessed clinicians' adherence to the protocol by asking independent raters to listen to audiotapes of a random sample of sessions (33 tapes, or one of every four sessions). Overall, the ratings indicated that group leaders adhered closely to the intended protocol and that quality of implementation was midway between good and very good.
The second implementation check assessed participants' adherence by rating their compliance with behavioral homework tasks as reviewed in each of the 11 sessions. The average homework compliance ratings indicated that participants acted according to plan when doing two or three behavioral tasks per week but were falling short in their commitment to daily behavioral challenges.
Between-groups analyses
Our primary hypothesis was that participants in the immediate-treatment group would experience greater reductions in anxiety than would participants in the wait-list control group.
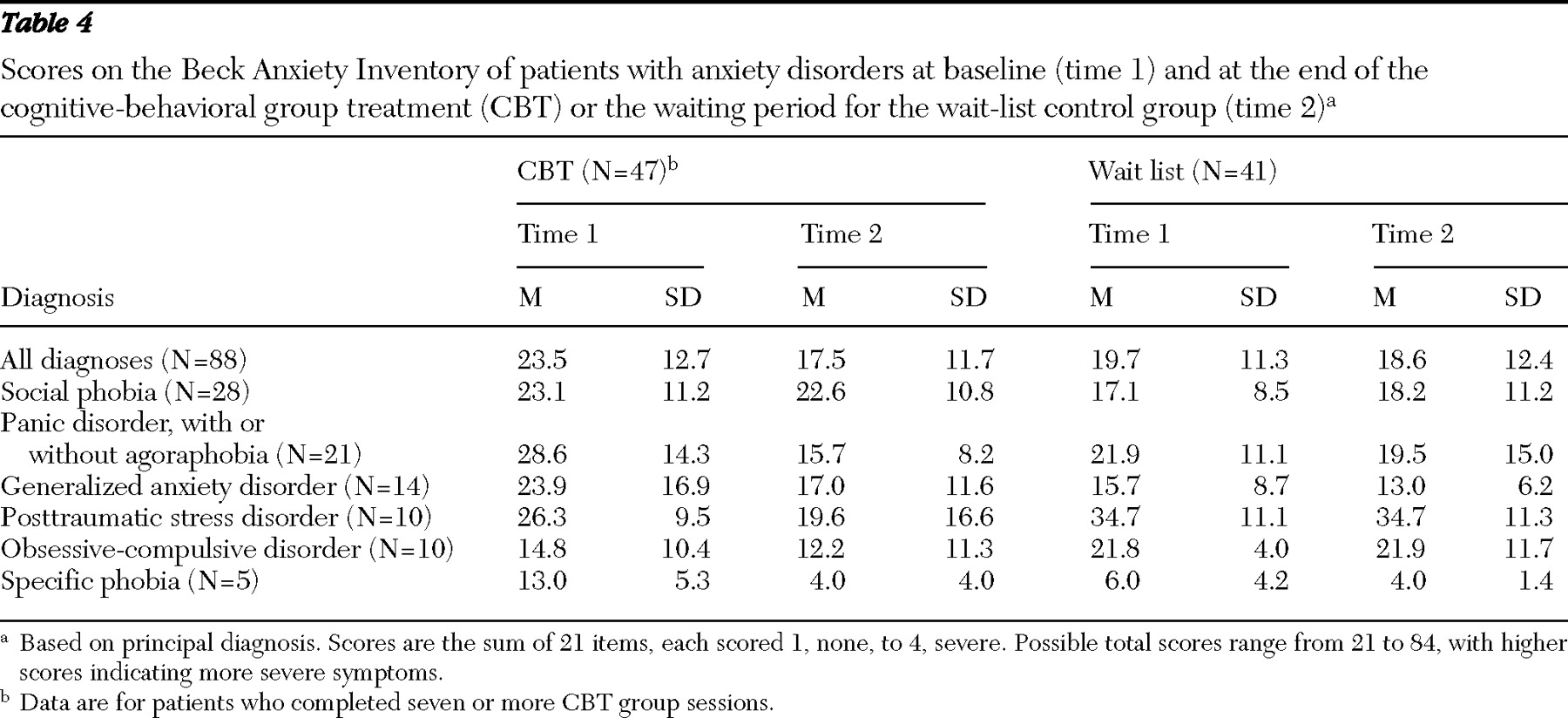
Table 4 shows the BAI scores at baseline and at the end of either the treatment group or the waiting period for the two groups (T2). To assess the between-groups differences, we used analysis of covariance, with T2 BAI scores as the dependent measure and T1 BAI scores as the covariate. In
Table 4 the first row shows that across all diagnoses the reduction in BAI scores was larger in the immediate-treatment group than in the wait-list control group (F=8.12, df=1 and 10.34, p=.017). The magnitude of the between-groups effect immediately after treatment or the waiting period (partial
η 2 =.44) corresponds to a medium effect size.
The medium effect size overall does not identify the presence of clinically significant changes. Therefore, we calculated the proportions of participants in each condition who achieved either a 20% or 40% improvement in their BAI scores. The immediate-treatment group was superior in both respects: 61% (25 of 41) achieved the 20% change criterion compared with 31% (11 of 35) in the control group ( χ 2 =6.61, df=1, p=.01); and 42% (17 of 41) reached the 40% change criterion compared with 17% (six of 35) of the control group ( χ 2 =5.29, df=1, p=.02).
Table 4 also shows reductions in anxiety severity for each diagnostic group. To assess the secondary hypothesis, albeit with limited power because of the small number of cases, we used analysis of covariance for each diagnostic group. For patients with panic disorder, the results indicate that the immediate-treatment group did significantly better than their counterparts (F=7.42, df=1 and 19,
η 2 =.28, p<.01). No other diagnosis-specific changes in BAI scores approached significance.
Within-groups analyses
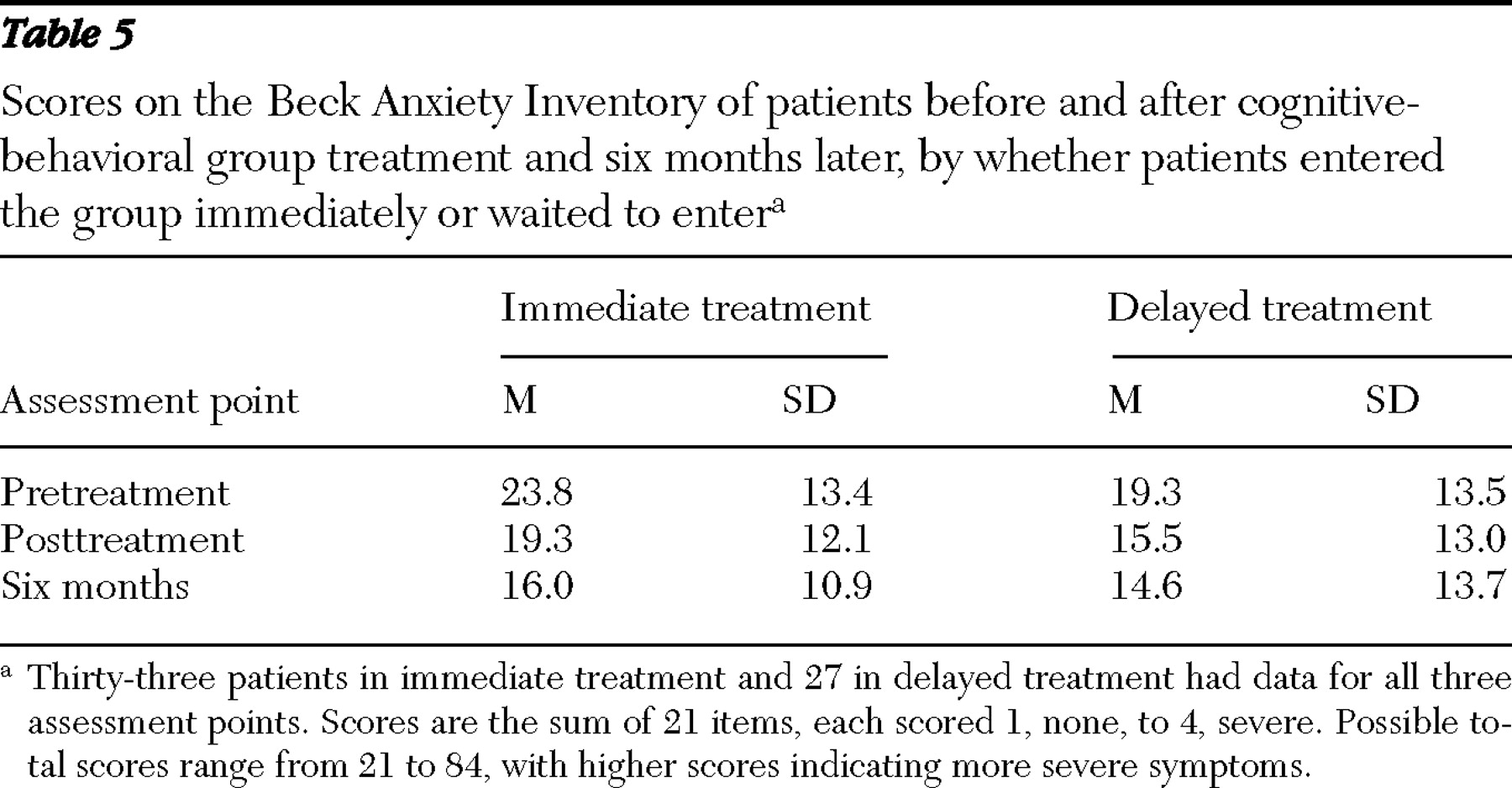
Because the between-groups analyses showed that treatment produced an immediate effect on BAI scores, we assessed the durability of the reductions in anxiety across time. We used a mixed-model (between and within) repeated-measures analysis of variance in BAI scores over time. The results are shown in
Table 5 .
The data in
Table 5 suggest that the BAI scores at the six-month follow-up were at least equivalent to scores immediately after treatment. The analysis of variance indicated a main effect for time (F=12.58, df=2 and 57, p<.001) but no effect either for treatment condition or for the interaction of condition by time. Post hoc pairwise comparisons that pooled the immediate- and delayed-treatment groups indicated that posttreatment reductions in anxiety continued to be present at the six-month follow-up (the mean difference in the pretreatment and six-month BAI score plus SE: 6.3+1.3; d=.50, p<.001). The comparison of posttreatment and six-month BAI scores indicated a nonsignificant trend toward further reduction in anxiety during the follow-up period (p=.07).
Discussion
We designed a CBT group in which patients with different and multiple anxiety disorders were treated concurrently in the same group, which is a format more amenable to general mental health clinics. The 11-week protocol includes CBT elements common to the treatment of many anxiety disorders, as well as diagnosis-specific techniques. Specifically, we have shown that treatment with the heterogeneous group format reduced the severity of self-reported anxiety symptoms compared with a wait-list control group. Significant reductions in BAI scores, equivalent to a medium effect size, were apparent immediately after treatment and were maintained over the following six months. Substantial portions of clients achieved clinically important reductions in symptom severity.
No large, controlled trial in the published literature has examined this format. This study is the first to have adequate power to estimate an effect size for the full sample and to consider—in the context of secondary hypotheses—the effect of the format for at least one diagnostic group.
Moreover, the presence of clinically and statistically significant changes in the context of an effectiveness paradigm enhances the external validity of the mixed-disorders format.
Despite rigorous methods and a large sample, the effect size was substantial (d=.50) but less than that typically obtained with diagnosis-specific CBT protocols. The effectiveness paradigm, and the concomitant inclusion of many patients with severe and complex disorders, may have been partly responsible for the medium effect size (
19 ). The effect size here is consistent with that described in two earlier uncontrolled effectiveness trials (
12,
13 ) and smaller than that described by Norton and colleagues (
14 ) in an efficacy trial.
Like many studies, this investigation was not without limitations. One limitation is the reliance on a single pandiagnostic measure of outcome, based on self-report. Clinician ratings of symptom severity or functional status, often seen to be more sensitive to change, may have resulted in a larger effect size. Further, the choice of the BAI as the sole self-report measure may have focused on change in physiological aspects of anxiety at the expense of cognitions and behavior and thus may have been more sensitive to change among patients with panic disorder.
Another limitation may have been the treatment protocol itself. Our clinical impressions were that too much information was presented and that too many skills were discussed and taught. That Norton and colleagues (
14 ) detected between-groups differences despite a small heterogeneous sample may have reflected their "minimalist" strategy to teach only a small number of skills in their mixed-anxiety CBT group.
A third limitation is related to the selection of primary and secondary hypotheses. Our study was designed to detect a medium effect size overall and not intended to detect the varying effect sizes of the different diagnostic groups. Further research will pursue this important question.
A final limitation may have been a consequence of the effectiveness paradigm. The clientele at our three clinics have substantial differences, especially in terms of comorbidity and adaptive functioning. A substantial minority of clients were both severely distressed and impaired. In the future, we may reconsider the rationale for a single group protocol that is suitable for virtually all anxiety clients. For example, we may wish to broaden the exclusion criteria (for example, excluding those with a GAF score under 40) or add an inclusion criterion (for example, including only those with behavioral avoidance [
12 ]).
Conclusions
In terms of population health, few people with anxiety disorders receive good treatment. That CBT has been available only in diagnosis-specific protocols has, in our opinion, played a significant role in limiting needed treatment services. A CBT protocol for a heterogeneous group of patients with anxiety disorders may make effective treatment more broadly available, similar to other dissemination efforts that include peer-led treatments (
20 ) and self-help strategies (
21,
22 ). Further research addressing the nature of the mixed-disorders protocol, the magnitude of effects for different diagnostic groups, and suitable inclusion and exclusion criteria is needed before this format is ready for dissemination.
Acknowledgments and disclosures
The authors gratefully acknowledge the support of the Special Opportunities Research Fund (grant V02-0030) awarded by the VGH and UBC Hospital Foundation.
The authors report no competing interests.