Shared decision making denotes the process of enabling clients to participate actively and meaningfully in their treatment by providing them with accessible information and choices. There are ethical, clinical, and economic arguments for shared decision making (
1 ). Self-determination over one's body is considered a fundamental principle of medical ethics (
2 ). Clients are often best suited to make treatment decisions because only they can value trade-offs in efficacy and side effects (
3 ). Furthermore, they often experience better outcomes when given information and choices (
1 ). Several studies have shown that decision aids decrease enthusiasm for expensive and questionably effective therapies and are thus cost-effective (
4 ). Active client participation often increases satisfaction, facilitates treatment adherence, and in some cases decreases symptom burden (
4 ). Although many current mental health interventions promote client-centered care, client choice, and self-directed care, the research is just beginning on shared decision making in mental health for clients with severe and persistent mental illness (
1,
5 ).
Methods
We explored clients' preferences for decision-making style in a pilot study by administering several decision-making questionnaires, including qualitative and quantitative approaches, to 30 persons with severe mental illnesses at a community mental health center in New Hampshire between July 1 and November 1, 2004, and July 1 and November 1, 2005. Institutional review boards for the state of New Hampshire and for Dartmouth Medical School approved the study, and all respondents provided written informed consent for their participation.
The first 15 interviews were conducted with a convenience sample of clients of the mental health center. The last 15 clients were randomly selected from the entire client list at the same center (repeats were excluded). The groups differed minimally in that the randomly selected group was more likely to have had more than a high school education (N=11, or 73%, and N=7, or 47%) and was less likely to be diagnosed as having schizophrenia (N=2, or 13%, and N=8, or 53%), but the findings were similar for the two groups. We therefore present data for the combined study group of 30 clients.
We administered two scales to assess preferences for decision-making style. The Autonomy Preference Index Decision-Making scale (API-D) (
6 ) consists of six discrete Likert questions related to a preference for autonomous decision making and medical information. The responses are scaled from 0 to 100, and a higher score indicates a greater preference for autonomous decision making. The Control Preferences Scale (CPS) (
7 ) consists of one question that conceptualizes decision making along a linear axis from "mostly my doctor's decision" to "mostly my decision." We applied this simple scale to several decision areas, including medications, housing, jobs, choice of a practitioner, and general medical care. For all scales, instances of "doctor" were replaced with "psychiatrist." We also asked clients open-ended questions regarding decision-making experiences and preferences, and these discussions were used to validate their preferences and perceptions of current services.
We examined the association between the CPS rating and the following categorical independent variables: age (older than 50 years), sex, education (further than a high school diploma), self-reported substance abuse, and self-reported diagnosis of schizophrenia. For this analysis we used the chi square test, and we analyzed the API-D results with Student's t test. We compared preferred roles with perceived roles and psychiatric roles with general medical care roles on the CPS by using the Wilcoxon ranked-sum test.
Results
The mean±SD age of the participants was 47±10 years, 14 (47%) were male, ten (33%) reported having a schizophrenia spectrum diagnosis, 19 (63%) were unemployed, eight (27%) had not completed high school, four (13%) completed high school, and 18 (60%) had some education beyond high school.
Mean scores on the 100-point API-D preference subscale were 51±9. There were no significant differences in role or information preferences (according to the API-D or the CPS) in relation to age, sex, education, substance abuse, or schizophrenia diagnosis.
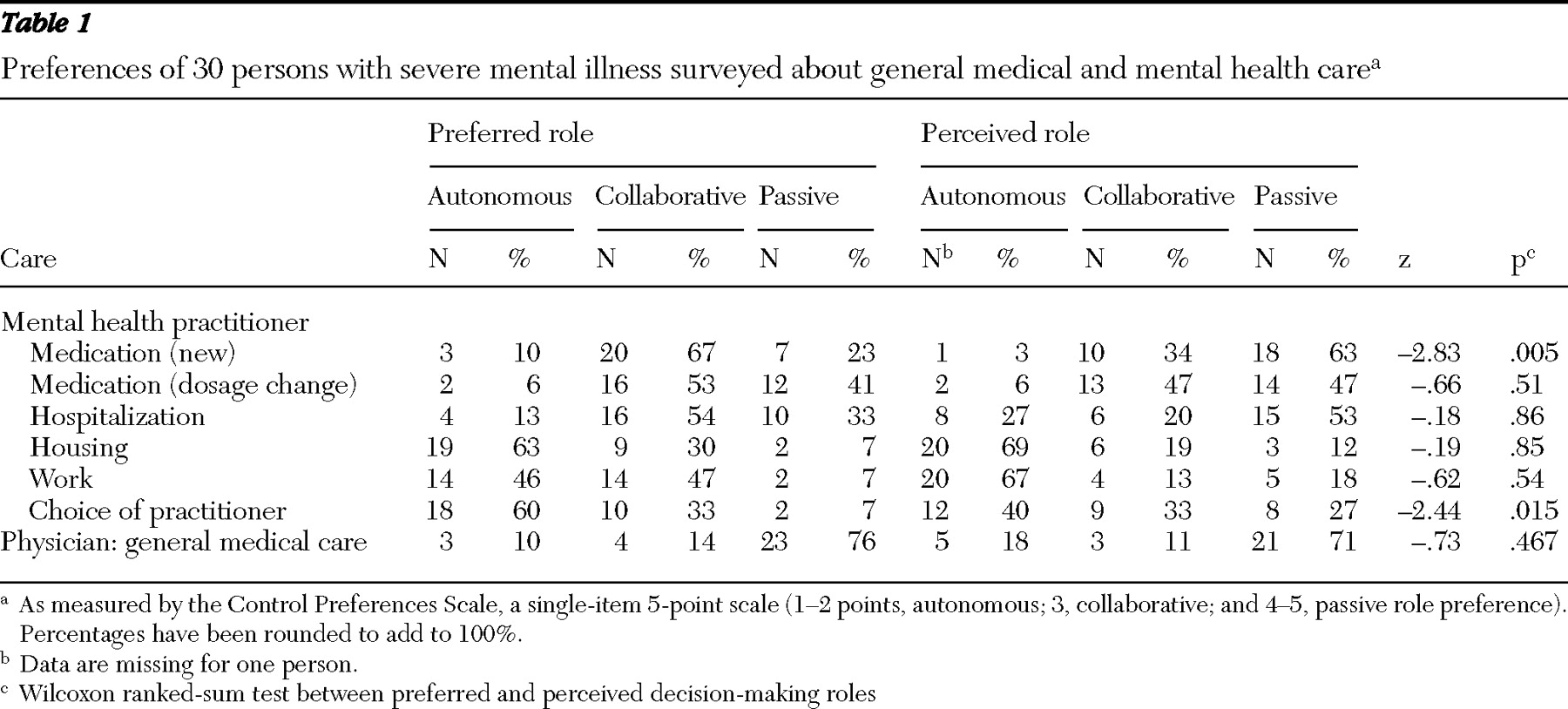
Table 1 shows preferred and perceived decision-making roles—that is, the roles that clients felt they wanted and those they had experienced. One client had missing data for perceived roles. Clients appeared to vary among themselves and across different decision areas in their preferences for decision-making style. A statistically significant difference emerged in the area of decisions regarding starting new medications, where 39% (derived by subtracting the percentage of clients who experienced a passive role, 62%, from the clients who preferred a passive role, 23%) of clients indicated they would prefer a more active or collaborative role than the one they experienced. In comparing mental health care and general medical care, clients were less likely to prefer a passive role in medication decisions in psychiatry than in general medical care (23% compared with 76%, z=-3.01, p=.003). The CPS was validated by answers to open-ended questions. Clients understood the scale questions and responded in ways consistent with their more detailed answers.
Discussion and conclusions
This pilot study not only identified usable scales to study decision making in the population but also indicated that many clients with severe mental illnesses express a preference for shared decision making. Two previous studies used the API-D to assess people with severe mental illness (
8,
9 ). Hill and Laugharne (
9 ) reported a mean score of 47.7±16.0 among 111 clients of their community health team in England (54% response rate) and a mean score of 54±16 among 49 users of a mental health forum (31% response rate). Hamann and colleagues (
8 ) reported a mean score of 46±18 among a convenience sample of 122 inpatients with schizophrenia in Germany. These numbers are equidistant between the two poles of autonomy and passivity on the CPS. The findings of these studies, including our own finding of a mean score of 51±9, are slightly higher than those that Ende and colleagues (
6 ) reported for outpatients with diabetes (API-D: 33.2±12.6), indicating a relatively greater desire for participation in decision making. Degner and colleagues (
7 ) used the CPS and found a heterogeneous preference among persons being treated for breast cancer (N=223, or 22% autonomous; N=445, or 44% collaborative; and N=344, or 34% passive); only 425 (42%) were in their preferred role. Our results for individuals with severe mental illness resemble those for people with other long-term disorders in expressing varied preferences for decision-making styles, although our clients were more likely to prefer a passive role in general medical care than in psychiatric care.
This pilot study has several limitations. The study included a relatively lengthy interview and was designed to examine in depth the usefulness of standardized instruments as well as outcomes. The study group was small, and the statistical tests therefore lacked power. The study group also was skewed toward educated and employed clients in a mental health center. People with less education or motivation or those in other settings may differ in their desires for participating in shared decision making. Larger and more representative study groups are needed to establish stable confidence intervals. The study did not address concerns regarding temporary decisional incapacity. Although not a limitation, the large discrepancies between preferred and perceived roles in new medication, hospitalization, and choice of psychiatrist may indicate that these areas make incorporating patient preferences in the decision-making scheme more difficult.
Nevertheless, our data suggest several clinically relevant implications that are worthy of further attention. First, clients with severe mental illnesses appear to differ among themselves in their preferences for shared decision making, but many prefer active and collaborative roles, similar to those with other medical conditions. Second, clients appear to prefer greater participation in mental health treatment decisions than they are accorded. This finding is consistent with qualitative research on psychiatric decision making (
10 ) and with the conclusions of the President's New Freedom Commission on Mental Health (
11 ) and the
Improving the Quality of Health Care for Mental and Substance-Use Conditions: Quality Chasm Series (
12 ), all of which stress the importance of care that is guided by patients' preferences and by shared knowledge that stems from the free flow of information. Finally, clients' preferences appear to vary in relation to different types of decisions, but they are particularly interested in active roles in relation to psychotropic medications.
Acknowledgments and disclosures
This work was sponsored by the Foundation for Informed Medical Decision Making George Bennett Fellowship and by the West Foundation.
The authors report no competing interests.