Depression and anxiety are two major causes of morbidity and mortality in the United States and are associated with impaired health-related quality of life and social functioning (
1,
2,
3,
4 ), as well as with excess disability (
5,
6,
7 ). In addition, psychiatric conditions, particularly depressive disorders, are associated with increased prevalence of chronic diseases and often precipitate or exacerbate these conditions (
8 ). Fortunately, depression and anxiety can often be successfully treated with medication and psychotherapies (
9 ). However, most adults do not seek care, and those who do often do not receive appropriate care (
9 ).
The state health departments in collaboration with the Centers for Disease Control and Prevention (CDC) and the Center for Mental Health Services, Substance Abuse and Mental Health Services Administration, collaborated on the implementation of the Anxiety and Depression Module for the Behavioral Risk Factor Surveillance System (BRFSS). This module collects information about depression and its severity with the clinically validated eight-item Patient Health Questionnaire depression measure (PHQ-8). Additionally, two questions were included on lifetime diagnosis of depression and anxiety (one each). The BRFSS is the world's largest ongoing telephone health survey system. Given its large sample size, the BRFSS is able to produce local, state, and national estimates. Additionally, the BRFSS collects data on chronic illness, health behaviors, disability, access to health care, and health-related quality of life—items not characteristically found in other data systems collecting mental health data. The purpose of this study was to examine the unadjusted and adjusted prevalence estimates of depression and anxiety at the state level and to examine the odds ratios of depression and anxiety for selected risk behaviors, obesity, and chronic diseases.
Methods
The BRFSS is a state-based surveillance system operated by state health departments in collaboration with the CDC. The cross-sectional data were collected throughout the year in 2006. The objective of the BRFSS is to collect uniform, state-specific data on preventive health practices and risk behaviors that are linked to chronic diseases, injuries, and preventable infectious diseases in the adult population (
10,
11 ). Trained interviewers collect data monthly from a standardized questionnaire by using an independent probability sample of households with telephones in the noninstitutionalized U.S. adult population. The BRFSS has CDC Institutional Review Board approval.
The BRFSS questionnaire consists of three parts: core questions asked in all 50 states, the District of Columbia, Puerto Rico, and the U.S. Virgin Islands; supplemental modules, which are a series of questions on specific topics (for example, adult asthma history, intimate partner violence, and mental health); and state-added questions. In 2006 trained interviewers administered questions about depression severity and lifetime diagnosis of anxiety and depression (Anxiety and Depression Module) in 38 states (Alabama, Alaska, Arkansas, California, Connecticut, Delaware, Florida, Georgia, Hawaii, Indiana, Iowa, Kansas, Louisiana, Maine, Maryland, Michigan, Minnesota, Mississippi, Missouri, Montana, Nebraska, Nevada, New Hampshire, New Mexico, North Dakota, Oklahoma, Oregon, Rhode Island, South Carolina, Tennessee, Texas, Utah, Vermont, Virginia, Washington, West Virginia, Wisconsin, and Wyoming), as well as in the District of Columbia, Puerto Rico, and the U.S. Virgin Islands. Additional methods used in the BRFSS, including the weighting procedure, are described elsewhere (
12 ). All BRFSS questionnaires, data, and reports are available at
www.cdc.gov/brfss . All analyses are from weighted data.
To assess the prevalence of depression and its severity in the general U.S. population, the standardized and validated PHQ-8 was used (
13 ). The PHQ-8 consists of eight of the nine criteria on which the
DSM-IV diagnosis of depressive disorders is based (
14 ). It is half the length of many other depression measures and has comparable sensitivity and specificity (
13 ). The ninth question in the
DSM-IV assesses suicidal or self-injurious ideation and was omitted because interviewers are not able to provide adequate intervention by telephone. Research indicates that the deletion of this question has only a minor effect on scoring because thoughts of self-harm are fairly uncommon in the general population (
13 ). The PHQ-8 has been used in both clinical (
15,
16,
17 ) and population-based settings (
18,
19 ) and in both self-administered (
15,
16,
17 ) and telephone-administered modes (
20 ). Additionally, it has been shown to be effective for detecting depressive symptoms in various racial and ethnic groups (
17,
18,
20,
21 ).
The PHQ-8 response set was standardized to make it similar to other BRFSS questions by asking the number of days in the past two weeks the respondent experienced a particular depressive symptom. The modified response set was converted back to the original response set: zero to one days, not at all; two to six days, several days; seven to 11 days, more than half the days; and 12 to 14 days, nearly every day, with points (0 to 3) assigned to each category, respectively. The scores for each item are summed to produce a total score between 0 and 24 points. A total score of 0 to 4 represents no significant depressive symptoms, whereas a total score of 5 to 9 represents mild depressive symptoms, 10 to 14 represents moderate symptoms, 15 to 19 represents moderately severe symptoms, and 20 to 24 represents severe symptoms (
13 ). Current depressive symptoms were defined as a PHQ-8 score ≥10.
In addition to questions about current depressive symptoms, one question each on lifetime diagnosis of anxiety and depression was asked: "Has a doctor or other health care provider ever told you that you have an anxiety disorder (including acute stress disorder, anxiety, generalized anxiety disorder, obsessive-compulsive disorder, panic attacks, panic disorder, phobia, posttraumatic stress disorder, or social anxiety disorder)?" and "Has a doctor or other health care provider ever told you that you have a depressive disorder (including depression, major depression, dysthymia, or minor depression)?"
Cardiovascular disease was assessed with three questions: "Has a doctor, nurse, or other health professional ever told you that you had a heart attack, also called a myocardial infarction?" "Has a doctor, nurse, or other health professional ever told you that you had angina or coronary heart disease?" "Has a doctor, nurse, or other health professional ever told you that you had a stroke?" Persons were considered to have cardiovascular disease if they responded to all three questions and at least one response was a yes. Persons were considered not to have cardiovascular disease if they answered no to all three questions. Diabetes status was assessed with one question: "Have you ever been told by a doctor that you have diabetes?" Women who reported diabetes only during pregnancy were not considered to have diabetes. Persons were considered to have asthma if they responded yes to the question, "Have you ever been told by a doctor, nurse, or other health professional that you had asthma?"
The BRFSS respondents were also asked about their smoking habits, physical activity, height and weight, and alcohol consumption. Respondents were considered to be current smokers if they had smoked at least 100 cigarettes in their lifetime and currently smoked. Persons were considered to be physically inactive if they had not participated in any leisure-time physical activity or exercise during the past 30 days. Body mass index (BMI=weight [kg] divided by height [m
2 ]) was determined from self-reported height and weight. Persons were considered obese if their BMI was ≥30 kg/m
2 . Heavy drinkers were defined as men who reported drinking more than two drinks per day and as women who reported drinking more than one drink per day (
22 ).
Data were available for 217,379 participants in the 38 states, the District of Columbia, Puerto Rico, and the U.S. Virgin Islands who responded to at least one question in the Anxiety and Depression Module. Approximately 8.6% of PHQ-8 scores were missing, .9% of participants did not respond to the question on lifetime diagnosis of anxiety, and .8% did not respond to the question on lifetime diagnosis of depression. The median cooperation rate, the percentage of eligible respondents who completed the survey, for the 41 states and territories in the 2006 BRFSS, was 75.2%; ranging from 56.9% in California to 89.0% in Puerto Rico. Prevalence estimates, adjusted odds ratios, and standard errors were computed by using SUDAAN release 9.0.1 to account for the complex survey design. Because of the large sample, statistical testing was not emphasized. Five states—Connecticut, Kansas, Maryland, Nebraska, and Washington—collected the Anxiety and Depression Module on a subset of the state sample rather than on the entire sample, a common practice in BRFSS, to increase the number of questions asked in states with large samples. These responses are weighted back to the population of the state. Information on the weighting methodology and the weights to use for each of these states can be found at
www.cdc.gov/brfss/technicalinfodata/surveydata/2006/2006dual.htm .
Results
More than 22.7 million people in the 38 states, the District of Columbia, Puerto Rico, and the U.S. Virgin Islands reported being told by a health care provider that they had depression at some point during their lifetime, and more than 16.3 million people reported being told by a health care provide that they had anxiety at some point during their lifetime. Additionally, more than 11.8 million people had current depressive symptoms at the time of the survey, as assessed by the PHQ-8.
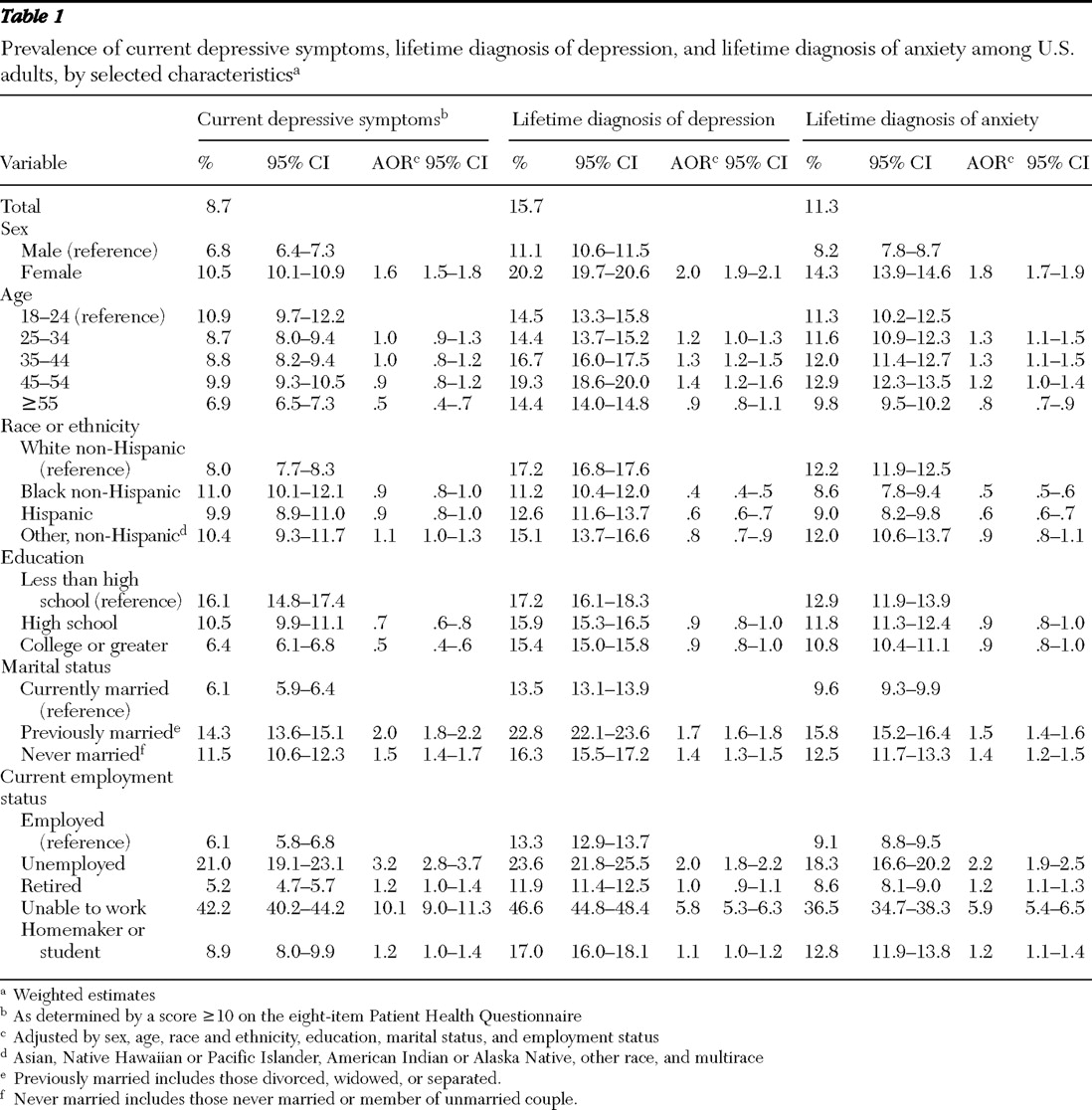
After adjustment for sex, age, race or ethnicity, education, marital status, and employment status, women were significantly more likely than men to have current depressive symptoms, as were those previously married or never married (compared with those married), and as were those who were unemployed or unable to work (compared with those currently employed) (
Table 1 ). Additionally, adults aged 55 years and older were less likely than those aged 18 to 24 years to have current depressive symptoms, as were those with at least a high school education (compared with those with less than a high school education).
Women were also significantly more likely than men to have a lifetime diagnosis of depression, as were adults aged 35 to 54 years of age (compared with those aged 18 to 24 years), those previously married or never married (compared with those married), and those unemployed or unable to work (compared with those currently employed). Moreover, black non-Hispanics, Hispanics, and other non-Hispanics were less likely than white non-Hispanics to have a lifetime diagnosis of depression. Finally, women were more likely than men to report a lifetime diagnosis of anxiety, as were adults aged 25 to 44 years (compared with those aged 18 to 24 years), those previously married or never married (compared with those currently married), and those currently unemployed, retired, or unable to work and homemakers or students (compared with those currently working). Moreover, adults aged 55 years or older were less likely than those aged 18 to 24 years to report a lifetime diagnosis of anxiety, as were black non-Hispanics and Hispanics (compared with white non-Hispanics).
Approximately 8.4% (95% CI=8.1%–8.6%) of respondents had a lifetime diagnosis of depression only, 4.0% (CI=3.8%–4.2%) had a lifetime diagnosis of anxiety only, and 7.3% (CI=7.1%–7.5%) had a lifetime diagnosis of both depression and anxiety. A lifetime diagnosis of depression was much more likely among adults currently depressed than among adults not currently depressed (54.7% [CI=52.9%–56.5%] versus 11.9% [CI=11.6%–12.2%], respectively). Similarly, current depressive symptoms were much more likely among those with a lifetime diagnosis of depression than those with no prior depression (30.5% [CI=29.4%–31.6%] versus 4.7% [CI=4.4%–4.9%], respectively). Among those with no current depressive symptoms, 8.8% (CI=8.5%–9.1%) had a lifetime diagnosis of depression, as did 26.2% (CI=25.2%–27.2%) of those with mild current depressive symptoms, 46.7% (CI=44.4%–49.1%) of those with moderate current depressive symptoms, 63.3% (CI=60.6%–66.4%) of those with moderately severe current depressive symptoms, and 73.5% (CI=69.2%–77.4%) of those with severe current depressive symptoms.
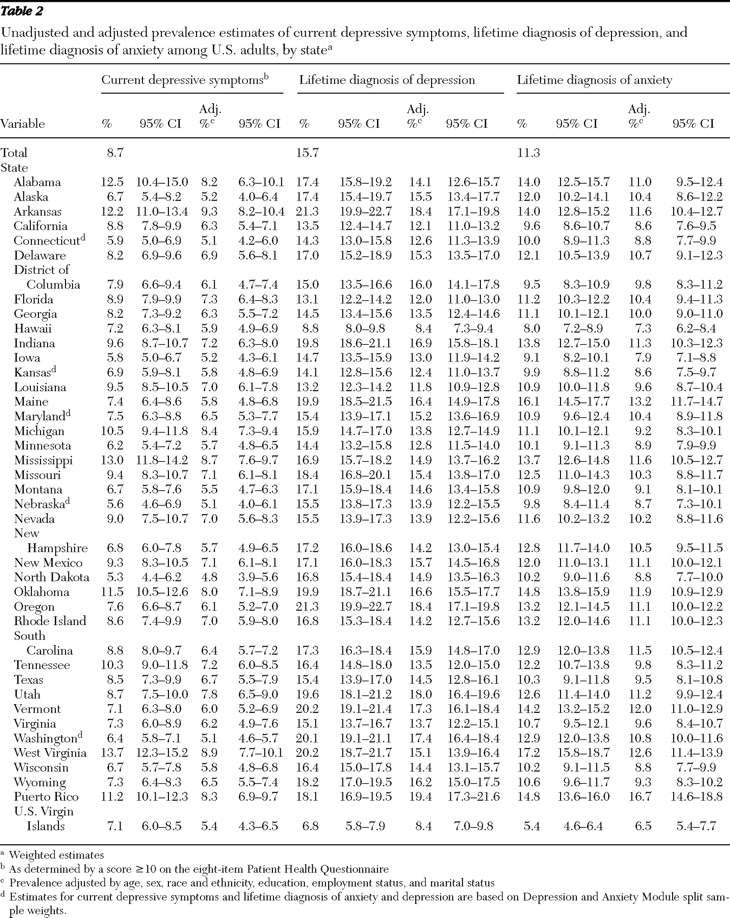
There was considerable geographic variation in rates of depression and anxiety, as shown in
Table 2 . [Maps showing variation by state in rates of depression and anxiety are available as an online supplement at
ps.psychiatryonline.org .] The highest rates (<10%) of current depressive symptoms were found in Alabama, Arkansas, Michigan, Mississippi, Oklahoma, Tennessee, West Virginia, and Puerto Rico, whereas the lowest rates (<6%) were observed in Connecticut, Iowa, Nebraska, and North Dakota. A similar degree of regional variation was found in lifetime diagnoses of depression and anxiety: lifetime diagnosis of depression ranged from 6.8% to 21.3%, and lifetime diagnosis of anxiety ranged from 5.4% to 17.2%. Notably, variability still existed among the states after adjusting by age, sex, race and ethnicity, education, employment status, and marital status.
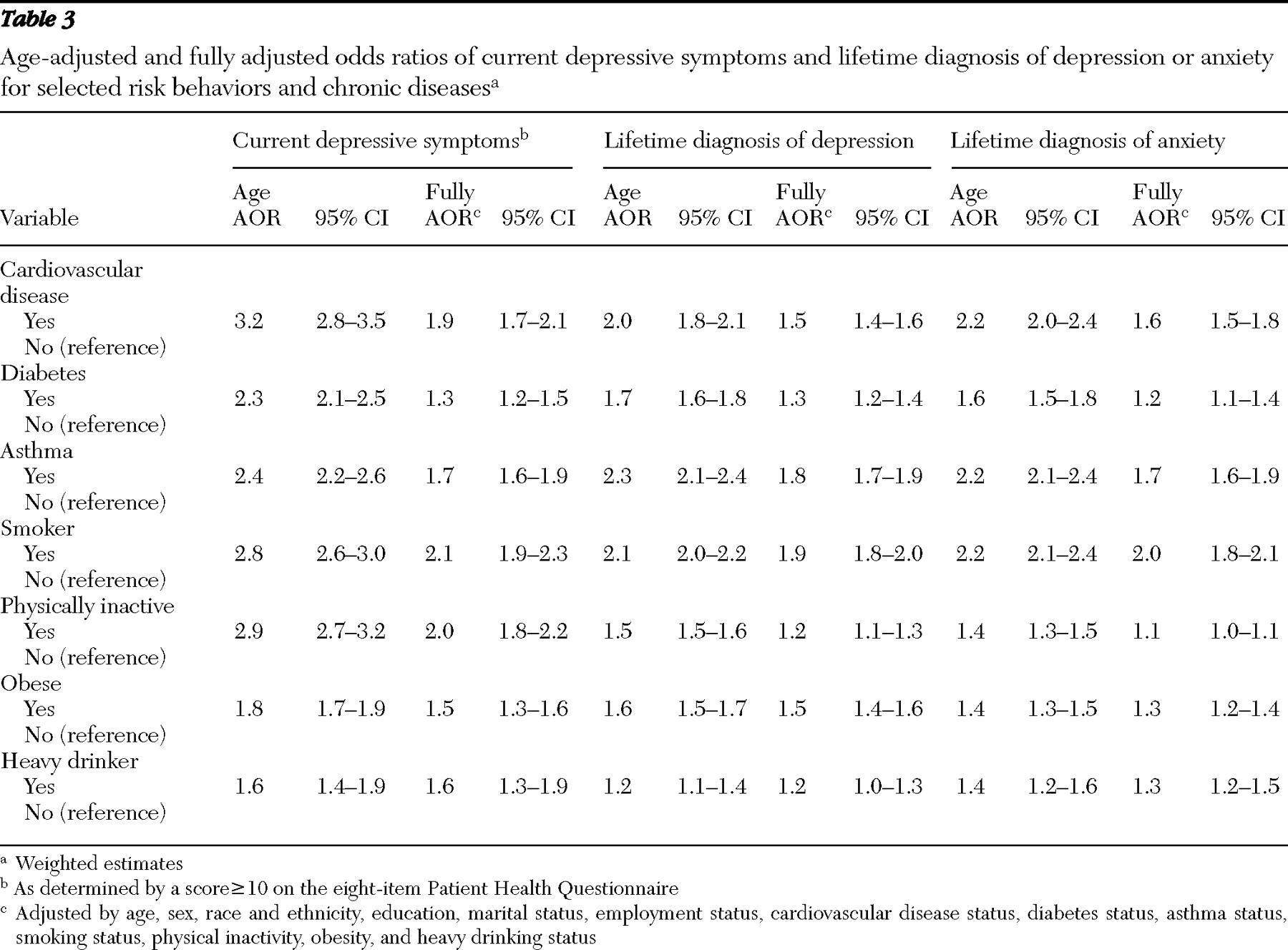
Unadjusted prevalence estimates indicated that cardiovascular disease, diabetes, asthma, smoking, physical inactivity, obesity, and heavy drinking were all significantly associated with current depressive symptoms, as well as with lifetime diagnoses of depression and anxiety (p<.001) (data not shown). After adjustment for the above conditions, behaviors, and sociodemographic characteristics, people with cardiovascular disease, diabetes, or asthma were significantly more likely than those without each condition to have current depressive symptoms, a lifetime diagnosis of depression, or a lifetime diagnosis of anxiety (
Table 3 ). People who were current smokers or were obese were also significantly more likely than persons who did not have each of these characteristics to have current depressive symptoms or a lifetime diagnosis of depression or anxiety. Physically inactive adults were significantly more likely than those who were physically active to have current depressive symptoms or a lifetime diagnosis of depression, whereas those who drank heavily were significantly more likely than those who did not to have current depressive symptoms or a lifetime diagnosis of anxiety.
Discussion
To our knowledge, this is the first U.S. study to examine the relationships between current depressive symptoms as assessed by the PHQ-8, chronic illness, and health risk behaviors. Additionally, it is the first study to examine unadjusted and adjusted prevalence estimates of anxiety and depression at the state level. Our study indicates a strong association between current depressive symptoms, a lifetime diagnosis of anxiety, and a lifetime diagnosis of depression and cardiovascular disease, diabetes, asthma, obesity, and several adverse health behaviors, such as smoking, physical inactivity, and heavy drinking. Moreover, it suggests that there is wide variation in the prevalence of anxiety and depression by state, even after adjusting for sociodemographic characteristics.
Notably, there is recent research indicating that the association between mental illness and chronic illness is based on physiological links, behavioral links, or both. For example, major depression and bipolar disorder are associated with an increased risk of both incident cardiovascular disease and subsequent death after a cardiovascular event (
23,
24 ). This could be due to a number of different behavioral and physiological associations: noncompliance with medical regimens; risk factors such as smoking, hypertension, diabetes, hypercholesterolemia, and obesity; hypothalamic-pituitary-adrenal axis hyperactivity and cortisol elevation; decreased heart rate variability; elevated plasma levels of proinflammatory cytokines leading to atherosclerosis; platelet activity and hypercoagulability; and psychological distress (
25 ).
Among persons with asthma, psychiatric disorders have been linked to more severe disease, poor asthma control, increased length of hospital stays, frequent visits to health care providers, increased use of steroid medication, noncompliance with medical regimens, and adverse behaviors, such as smoking, physical inactivity, and obesity (
26 ). Moreover, current research suggests that depression affects certain asthma symptoms, such as dyspnea, awakening at night with asthma symptoms, and morning symptoms (
27 ). Additionally, among persons with diabetes, recent research suggests that depressive symptom severity is associated with poorer diet and medical regimen adherence, functional impairment, and higher health care cost (
28,
29 ). Conversely, depression has been associated with a significantly increased likelihood of developing type II diabetes (
30 ).
Five of the main sources of epidemiological data for major depressive disorder—the Epidemiologic Catchment Area (ECA) study, the National Comorbidity Survey (NCS), the National Comorbidity Replication Survey (NCS-R), the National Epidemiologic Survey on Alcoholism and Related Conditions (NESARC), and the National Survey on Drug Use and Health—report a current depressive symptoms rate between 3.0% and 8.6%, a 12-month depression rate between 5.3% and 7.7%, and a lifetime depression rate of between 5.2% and 16.2% (
31,
32,
33 ). Although the BRFSS point estimate of 8.7% for current depressive symptoms is within the range found in these previous studies, it should be reiterated that a cutoff score of ≥10 on the PHQ-8 rather than a structured interview was used, and thus the BRFSS's estimate includes a proportion of individuals who may not meet criteria for major depressive disorder.
In regard to anxiety disorders, the ECA and NCS report a one-year rate of between 10.1% and 17.2%, and the ECA, NCS, and NCS-R report a lifetime rate between 14.6% and 28.8% (
34,
35 ). These rates are slightly higher than those found in this study. Because the ECA, NCS, and NCS-R used diagnostic tools to determine anxiety status and because the BRFSS asked whether the respondent had ever been diagnosed by a health care provider as having anxiety, it may be reasonable to assume that people with anxiety are not seeking medical care, do not recall a previous diagnosis of anxiety, or are not receiving an anxiety diagnosis from their clinician. This may be particularly true for simple phobias, which account for an important proportion of anxiety diagnoses on epidemiological surveys but are less frequently inquired about or diagnosed in clinical practice. Moreover, social anxiety disorder is often greatly underdiagnosed in clinical practice (
36 ). Finally, differences from previous studies are likely due to differences in methodology, especially in terms of the types of anxiety disorders being asked about.
There was substantial variability among states in the rates of depression and anxiety. These differences are not explained by variables available in BRFSS, such as demographic factors. This is not unique for depression and anxiety, as certain medical conditions (for example, diabetes and obesity) also exhibit geographic variability (
37 ). It is possible that regional differences in provision of mental health services could be a contributory factor. The existence of regional variability is important both to better understand risk factors for depression and anxiety as well as to target public health efforts and resources for detection and management.
Fortunately, depression and anxiety can often be successfully treated with medication and psychotherapy. In fact, it is quite possible that the difference between the prevalence of current and lifetime diagnosis of depression is attributable to current or past mental health treatment. However, most adults with probable depression or anxiety receive care exclusively from a primary care physician, and less than 20% of those receive medication or counseling that is consistent with treatment guidelines (
9 ). Additionally, among people with depression who are referred for psychotherapy from a primary care physician, only 20% ever entered treatment, and half of those did not complete treatment (
38 ). Moreover, persons from racial or ethnic minority groups have a higher prevalence of current depressive symptoms than whites but have lower rates of lifetime diagnosis, suggesting a need to eliminate disparities and to increase the availability of and access to mental health services in this population.
Many of the associations that this study found between health behaviors and depression and anxiety have been noted in the past. For example, not only does physical activity reduce the risk of coronary heart disease and diabetes and help build and maintain healthy bones, muscles, and joints (
39 ), it is also considered an adjunctive intervention to standard therapies for mild to moderately severe depression (
40 ) and anxiety (
41 ). Smoking is a risk factor for chronic illnesses such as asthma, cardiovascular disease, and lung cancer. Moreover, among adolescents and young adults, smoking might even increase the risk of developing certain anxiety disorders (
42 ). Smokers with major depression or anxiety smoke more and have higher rates of nicotine dependence, prolonged nicotine withdrawal symptoms, and lower abstinence rates than smokers without anxiety or depression (
43,
44,
45 ). Finally, mood and anxiety disorders have consistently been linked with substance use disorders such as alcohol dependence (
46,
47,
48 ). According to NESARC, 16.4% of people with major depression and 13.0% of those with an anxiety disorder have a comorbid alcohol use disorder (
48 ). Given these associations, using an integrated approach to health care that evaluates the comorbidity between physical, behavioral, and mental disorders is essential.
This study has several limitations. First, the rates in this study may be underestimated because BRFSS possibly excludes some people of low socioeconomic status and those with severely impaired physical or mental health; it also excludes those who are institutionalized or hospitalized and those without telephones or who block unknown outside calls from their phone. Second, depression and anxiety data were available for only 38 states, the District of Columbia, Puerto Rico, and the U.S. Virgin Islands; therefore, our results may not be representative of the entire country. Third, comparison of lifetime symptoms in different age groups should be interpreted with caution because there is a longer period of time in older groups over which one could have developed symptoms. Moreover, it is possible that lower lifetime prevalence among elderly persons is due to the possible greater likelihood of mortality among those with depressive symptoms. Finally, it is not possible to infer a causal relationship between depression, anxiety, cardiovascular disease, diabetes, asthma, and adverse health behaviors, although the cross-sectional data support the conclusion that these characteristics are associated.