One of the most important questions on the current U.S. domestic policy agenda is how to deliver high-quality, cost-effective health care. Several seminal reports released by the Institute of Medicine (IOM) have prompted a range of public- and private-sector strategies for stimulating improvements in provider accountability, efficiency, service delivery, and outcomes (
1,
2,
3,
4,
5 ). Efforts to pay (or otherwise reward) health care providers differentially on the basis of the quality of their performance are an example of these strategies. There are now over 150 pay-for-performance programs operating across the United States that are sponsored by 130 different health plans, coalitions of health plans, employer groups, Medicare, and Medicaid (
6 ). Together these programs cover 50 million health plan enrollees. Under recent legislation, the Centers for Medicare and Medicaid Services are preparing to provide a financial incentive to eligible professionals in the traditional Medicare fee-for-service program who participate in a voluntary quality reporting program.
Although the effect of these programs has not been examined sufficiently (
7,
8,
9 ), it is clear that current payment systems, if left unchanged, will continue to impede improved health care quality. Still, behavioral health remains conspicuously absent from most public- and private-sector quality improvement initiatives, including pay-for-performance programs. The Rosenthal and colleagues' review (
10 ) makes no mention of pay-for-performance programs in behavioral health, and the Leapfrog Group's compendium lists only two examples among 91 records (
11 ). This is despite the toll that mental and substance use disorders take on the American population.
These disorders are the leading cause of combined disability and death among women and are the second highest among men. Although effective treatments exist and continually improve, deficiencies in care delivery (which are also seen in general health care) prevent many individuals from receiving appropriate treatments. In a 2006 report entitled
Improving the Quality of Health Care for Mental and Substance-Use Conditions (
12 ), the IOM Committee on Crossing the Quality Chasm: Adaptation to Mental Health and Addictive Disorders concluded that "improving our nation's general health, and the quality problems of our general health care system, depends upon equally attending to the quality problems in health care for mental and substance-use conditions." The committee laid out an agenda and road map for building the infrastructure needed to improve the quality of health care for mental and substance use disorders, which adapts the Quality Chasm framework to behavioral health. The report also documents a number of critical distinctions between health care for mental disorders and substance use conditions and general medical care that limit the widespread implementation of quality improvement initiatives in behavioral health, including pay-for-performance programs.
Overall, there is less consensus on and implementation of a common set of quality improvement strategies and measures in behavioral health care than there is in general health care. There are several reasons for this. First, the predominance of numerous state-level public-sector programs in behavioral health reduces the likelihood that such programs will respond to market pressures for increasing quality and efficiency. For some types of care (for example, long-term psychotherapy), the large number of cash payers may further weaken the impetus for quality improvement because, unlike third-party payers, patients who pay out of pocket may be more likely to measure quality based on their personal experience with an individual provider. Second, the consensus-building process is complicated by the large number of disciplines licensed to diagnose and treat behavioral health problems and illnesses and the lack of an obvious means for determining accountability among them. These complications are compounded by the more active involvement of consumers and the complex clinical profiles of those treated in the public sector. Third, the infrastructure to measure, analyze, publicly report, and improve the quality of behavioral health care is less well developed than that for general health care. Fewer established clinical databases exist, and quality measurement and improvement mechanisms are relatively unsophisticated. Finally, the use of electronic health records, decision support, and other information technology applications for data collection, feedback, and reporting are limited in health care overall but even more limited in behavioral health care.
In this article, we present the results of a targeted national effort to identify and describe the core components of pay-for-performance programs currently operating in the field of behavioral health. Our examination includes consideration of the obstacles to program implementation and strategies for success. On the basis of this analysis, a number of actions are recommended to increase the effectiveness and use of behavioral health pay-for-performance programs in the future.
Methods
Between December 2005 and December 2006 the study team conducted a targeted national search to identify, as comprehensively as possible, pay-for-performance programs currently being implemented in the mental health and substance abuse fields (that is, behavioral health). In the context of this study, a pay-for-performance program was defined as the provision of financial or nonfinancial incentives to general medical or behavioral health specialty providers for quality improvement efforts that demonstrably enhance the effectiveness or efficacy of behavioral health care. This study was approved by the University of Pittsburgh's institutional review board.
Study population
The survey respondent population was identified through a three-step process. First, we conducted a focused review of the literature and Web sites, augmented by input from professional contacts in the field, to identify organizations and individuals likely to have knowledge of existing pay-for-performance programs. Through this process, we generated a list of 82 potential screening informants from various organizations, including health plans, business health coalitions, and academic centers recognized for work in this area, as well as federal and state agencies.
We then corresponded with each of these screening informants asking them to identify pay-for-performance programs through which health plans (for example, managed care organizations or managed behavioral health organizations) or purchasers (for example, employers or government agencies) offer financial or nonfinancial (for example, public recognition) incentives to individual clinicians, provider organizations, hospitals, or other general medical or specialty behavioral health facilities for quality improvement efforts designed to enhance the effectiveness or efficiency of behavioral health care and achieve better clinical outcomes. Through this process, we identified an additional 27 informants. Based on responses from 109 screening informants, we identified 24 specific pay-for-performance programs as defined above, and we interviewed 28 individuals associated with these programs. Informants most familiar with their organization's program were selected to respond. Additional informants were contacted to obtain further information when necessary.
The interviews were scheduled in advance and conducted over the phone by a member of the study team. To facilitate the interview process, a summary of the topics to be covered was sent to the respondents via e-mail several days before the scheduled call. Each interview took approximately one hour. All respondents reviewed our descriptions of their programs for accuracy before publication. Changes were suggested by the respondents to reflect updated information and clarify any ambiguous language.
Instrument and analysis
The semistructured interview protocol consisted of 36 questions assessing the core components of pay-for-performance programs adapted from the methodology used by Rosenthal and colleagues (
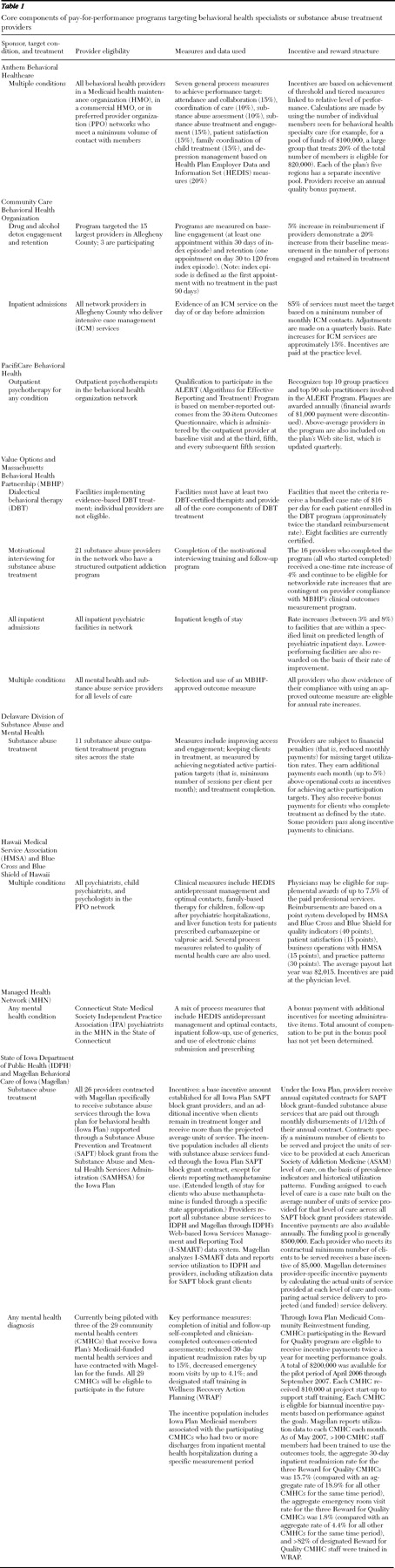
10 ). For each program, we collected information on seven core components: types of sponsors (for example, private or public), targeted disorders and treatments, provider eligibility, measures and data used, incentive and reward structure, obstacles to program implementation, and strategies for success. The program descriptions were organized into two tables: core components of pay-for-performance programs targeting behavioral health specialists and substance abuse treatment providers (
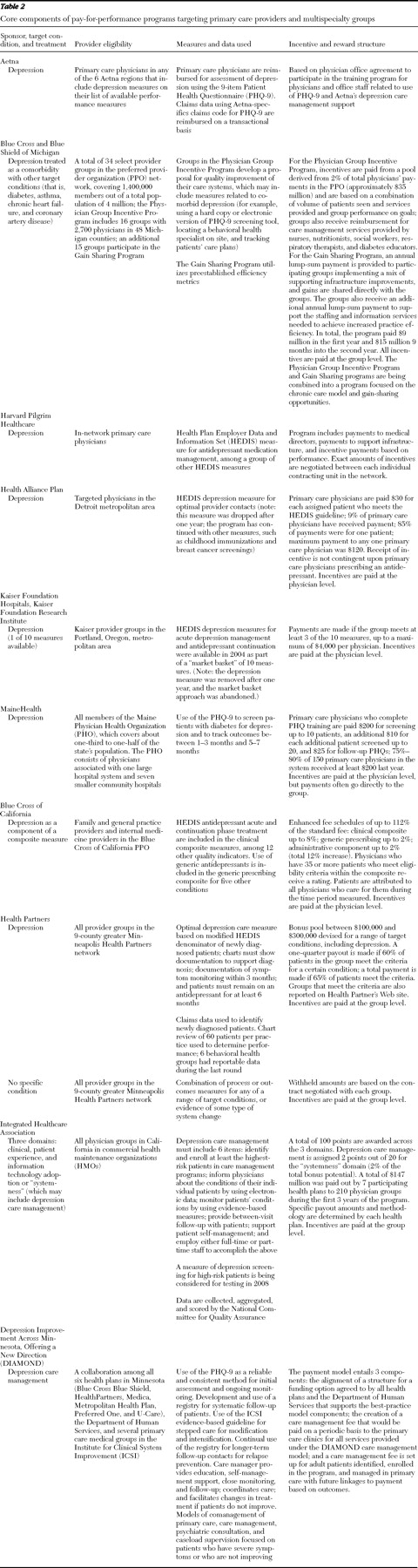
Table 1 ) and core components of pay-for-performance programs targeting primary care providers and multispecialty groups (
Table 2 ). This differentiation in overall program type reflects the fact that the implementation of pay-for-performance programs targeting behavioral health occurs differently in the behavioral health treatment sector than in the primary care sector.
Results
Through interviews with 28 informants, we identified 24 programs that met our inclusion criteria for pay-for-performance programs targeting behavioral health outcomes. Some organizations are listed more than once because they had separate pay-for-performance programs targeting different groups of providers.
Types of sponsors
Of the 13 programs targeting behavioral health specialists or substance abuse treatment providers, nine were sponsored by behavioral health plans, one was sponsored by a health plan, and three were sponsored by a state purchaser (
Table 1 ). Of the 11 programs targeting primary care providers or multispecialty groups, nine were sponsored by health plans and two were sponsored by a regional health consortium (
Table 2 ).
Targeted disorders and treatments
Ten of the 24 programs focused on depression as a target condition, and one additional program included depression among other target activities. Ten programs targeted a range of mental health or substance abuse treatment modalities, including drug and alcohol detox engagement (defined as the number of initial assessments) and retention (defined as the length of time in treatment), inpatient care admissions, dialectical behavioral therapy, motivational interviewing, and outpatient psychotherapy. Four programs targeted multiple disorders or allowed participating providers to work with the sponsors to select the target condition or treatment.
Provider eligibility
The behavioral health pay-for-performance programs targeted a wide array of health care providers. In some cases, the eligible groups were narrowly specified, such as therapists who use dialectical behavioral therapy to treat patients with a personality disorder or large addiction treatment providers in a single metropolitan area. In others, the eligible groups were quite broad, including all physicians in a region. Some programs focused on individual providers, whereas others targeted medical single-specialty and multispecialty groups. The programs were evenly split between those targeting behavioral health providers and those targetting general medical providers.
Measures and data used
Eight of the 11 programs addressing depression used the National Committee for Quality Assurance's Health Plan Employer Data and Information Set (HEDIS) measures for antidepressant medication management or optimal provider contacts. However, only two of these programs relied solely on the HEDIS scores for determining their performance metrics. Five programs required additional targets, such as additional HEDIS measures or inclusion of depression only when it co-occurred with other chronic medical conditions, so that the HEDIS score constituted only one part of an overall performance rating. Two programs targeting depression required the use of the nine-item Patient Health Questionnaire (PHQ-9) as a screening tool—one in addition to HEDIS measures and one to identify depression comorbid with other medical disorders. None of the program's incentives were based on outcomes derived from the use of the PHQ-9.
Generally speaking, pay-for-performance programs developed by behavioral health plans tended to be more innovative in the use of measures, such as staff members' completion of training in motivational interviewing or the use of certified dialectical behavioral therapists (
Table 1 ). In contrast, pay-for-performance programs in behavioral health targeting primary care providers used existing measures (that is, half of the programs described in
Table 2 used HEDIS measures for depression and three used the PHQ-9).
Incentive and reward structure
Programs offered incentives at both the individual physician and group levels. The dollar amounts of the incentives varied widely, from $120 per provider to several thousand dollars per group. Not all programs were able to provide the exact amount of incentives. Only one program offered a nonfinancial incentive: recognition as a top-tier provider on the health plan's Web site. The types of incentives were as varied as the disorders and treatments that were targeted. Eight programs provided incentives in the form of increased reimbursement for either the specific services targeted or an overall increase in the fee schedule. Three programs made lump-sum payments on an annual basis to providers who met their targets, and two programs paid a specified amount to providers either for the number of patients screened or for each patient who met the specified target. Two programs withheld a percentage of fees that were then paid back to groups that met their targets.
Obstacles to program implementation
The most common obstacle to program implementation cited was the lack of valid and practical quality measures in behavioral health. The seven programs that used the HEDIS measures for depression primarily did so only because sponsors and participating providers were able to agree on these standardized measures. However, respondents indicated that the lack of well-accepted measures for disorders other than depression made it impossible to address those disorders in their programs.
Tying incentives to specific behavioral health outcomes was also difficult. For the two programs that used the PHQ-9 to identify and monitor depression, the incentives were based solely on using the tool, and not on the outcomes achieved. One program, sponsored by PacifiCare Behavioral Health, based its incentives on improvements in outcomes (for psychotherapy), requiring therapists to fax in the results of their outcome measurements to the health plan. Although this program afforded an opportunity for individual therapists to be recognized as quality providers, the process is likely to be too burdensome (for both providers and plans) to be widely implemented across a range of providers and plans.
Many respondents indicated that providers were often either unwilling or unable to collect additional performance measurement data, so many of the programs had to rely on existing administrative data. However, a small number of programs did require more intensive data reporting from providers, and one program also used chart reviews.
Other barriers reported by respondents included providers' concerns about the validity of the data used to calculate incentive metrics as well as their doubts about receiving the promised incentives if certain targets were met. In some cases where incentives were available to groups or clinics, individual providers may not have been aware that the incentives existed.
Strategies for success
A majority of respondents agreed that obtaining buy-in from participating providers on the measures to be used was important to the overall success of their programs. Most program measures were chosen on the basis of a collaborative approach involving all stakeholders. The one health plan coalition interviewed—Integrated Healthcare Association—achieved a relatively higher degree of success because it was able to get all of the major health plans in the market to agree on one common set of performance measures. Each health plan then negotiated the specific financial inventive with each provider group. The medical groups being measured were satisfied because they were required to meet only one set of performance criteria.
Other issues of relevance to successful program implementation included the amount of the incentive and the size of the provider group. According to the payers who were interviewed, programs that used larger financial incentives reported fewer problems motivating provider involvement, and health plans that involved large provider groups or networks in their programs were more successful because larger groups had more resources at their disposal to make changes in their systems of care. For example, larger groups were more likely to have an electronic medical record allowing the provider to incorporate screening and tracking tools with less disruption to his or her practice. Larger practices were also able to absorb the added costs of devoting staff resources to deliver care management services by nurses or other allied health professionals. Many plans did not even offer the incentive programs to small groups, and even if they did, the groups were often not eligible because they failed to meet the specified minimum threshold of patient volume.
Discussion
Despite the proliferation of pay-for-performance programs focusing on general medical care, few pay-for-performance efforts specifically address behavioral health care. Our comprehensive review of the literature and interviews with key informants resulted in the identification of only 24 pay-for-performance programs that included any measurement of quality of care for mental or substance use disorders. Nevertheless, careful analysis of these programs revealed several preliminary lessons regarding pay-for-performance programs in general medical care and behavioral health. The results also point to a number of actions that can be taken in order to increase the effectiveness and use of behavioral health pay-for-performance programs in the future.
Preliminary lessons learned
The "Rewarding Results" pay-for-performance initiative conducted by the Leapfrog Group identified ten lessons learned about pay-for-performance (
11 ). Our study validates the importance of these lessons for both general medical care and behavioral health. For example, key factors that were identified in the successful implementation of behavioral health pay-for-performance programs by leaders of these programs include the engagement of providers in the design of measures and incentives, the use of incentives that are meaningful (financially), and outreach efforts to increase providers' awareness and knowledge.
At the same time, more work needs to be done on other components viewed as critical to the success of pay-for-performance programs. The financial incentives offered in behavioral health pay-for-performance programs were often small. Many programs struggled with the ability to obtain accurate and valid data on performance because of the combination of a lack of validated performance measures in behavioral health as well as the difficulty of data collection on behavioral health outcomes.
Furthermore, the public reporting of results was not widespread among the programs interviewed. In addition, only a small number of pay-for-performance programs in behavioral health have in place or plan to implement a rigorous evaluation. The resulting lack of data about the impact of behavioral health pay-for-performance programs on outcomes or cost-effectiveness significantly limits the extent to which such programs are likely to proliferate.
Increasing the effectiveness and use of programs in the future
Considering the results of this study in the context of the unique characteristics of behavioral health, we have identified a number of actions that can be taken in order to increase the effectiveness and use of behavioral health pay-for-performance programs in the future.
Adopt a longitudinal perspective on quality measurement. Recognizing that quality measurement in behavioral health lags behind related developments in other areas of health care, pay-for-performance programs in behavioral health should focus initially on offering incentives to providers for developing structures of care that support quality improvement, followed by incentives for using these structures to enhance the quality improvement process and, ultimately, for measuring the outcomes of these processes.
Develop outcome measures that are valid, practical to implement, and have buy-in from multiple stakeholders. Only after the measurement conundrum is resolved can we begin to examine the potential for performance incentives to affect the quality of behavioral health care. Feasible data collection processes need to be identified to ensure widespread implementation.
Link accountability to responsibility. Greater efforts must be made to ensure that all providers who are responsible for a particular patient's care are held accountable for the quality of care they provide; a pay-for-performance program that offers incentives based on patient outcomes to primary care providers might also offer similar incentives to the behavioral health specialist who is also participating in that patient's care.
Enhance the focus on behavioral health so that it is large enough to have an impact on provider behavior. It is likely that most pay-for-performance programs will continue to include behavioral health outcomes as a subset of other general medical care outcomes. However, if the quality of behavioral health care is to improve, the focus on behavioral health and the incentives that are offered to enhance provider performance must be large enough to matter to the provider.
Experiment with new models for improving performance and rewarding quality. Newly emerging programs—such as the Depression Improvement Across Minnesota, Offering a New Direction (DIAMOND) project—can serve as useful models for expanding stakeholder engagement, realigning financial policies to support evidence-based practices, and monitoring outcomes via electronic data submission.
Do not assume that one size fits all. Targeted approaches need to be designed for specific providers; incentives for substance abuse treatment providers, mental health centers, psychiatric hospitals, and outpatient psychotherapists will need to be tailored to the very different ways that these providers and facilities do business.
Conclusions
We conclude with a reaffirmation of the Rewarding Results finding that pay-for-performance is not a magic bullet that, in and of itself, will improve quality and control costs. Although pay-for-performance programs hold great promise for advancing the overall performance of the U.S. health care system, more comprehensive, systematic research is required in order to determine the desirability of using this approach in the context of behavioral health care. Intensive efforts aimed at strengthening the quality infrastructure in behavioral health will be a prerequisite for ensuring the implementation of more robust programs.
Acknowledgments and disclosures
This work was supported by grants 51814 and 55816 from the Robert Wood Johnson Foundation and by grant RR-024156 from the National Institutes of Health.
The authors report no competing interests.