Involuntary admission for psychosis has increased in recent years (
1 ). Research tends to categorize admissions for psychosis as voluntary or involuntary and generally shows that patients admitted involuntarily have poorer short-term outcomes, compared with those admitted voluntarily (
2,
3 ). Involuntary admissions, however, may occur for different reasons; for example, the patient may be extremely violent (that is, a forensic admission) or may not be able to care for himself or herself (that is, an involuntary admission). This suggests that it is appropriate to differentiate involuntary from forensic admissions. In addition, little is known about the relationship between first-admission status and long-term hospitalization outcomes. Therefore, this study examined the relationship between three types of hospital admission status (forensic, involuntary, or voluntary) at the time of the first psychiatric hospitalization and long-term hospitalization outcomes.
Research in Denmark has compared involuntary and voluntary admission status over 13 years among 53 patients and has shown that involuntary admissions accounted for 12% of admissions, occurred more frequently during the first half of the follow-up period, and were likely to be repeated by the same patients (
4 ). Similarly, research has examined the population-based registry of all first admissions for persons with a diagnosis of schizophrenia in Israel from 1978 to 1992, a period of relative system stability (
5 ). That study showed that a first admission with involuntary legal admission status was generally related to a second admission with involuntary legal admission status and to having more involuntary admissions. Other Israeli epidemiological research conducted during a time of system change (1991–2000) suggested that involuntary first admissions are more likely among males, younger persons, and those with less education (
1 ).
The criteria for involuntary admission vary by nation. The legal criteria for urgent involuntary admission in Israel include the presence of a psychotic state, risk of danger to others or oneself, and a causal relationship between psychosis and dangerous behavior. Nonurgent involuntary admission criteria include the presence of a judgment-impairing condition, lack of self-care, emotional harm to family members, and harm to property (
1 ). Forensic admissions in Israel resemble those in England and Wales (
6 ), because both legal systems include danger to others. Forensic hospitalizations are designated by the criminal justice system and may include referrals to determine competency for trial after a person commits a crime or they may indicate that a patient is too dangerous for a civil facility.
A first forensic admission may be a reason for hospitalization that is associated with poorer outcomes. For instance, research indicates that persistently violent patients show poorer outcomes (
7 ). The relationship between crime and subsequent hospitalization outcomes, however, has received scant attention. To extend past research it is appropriate to differentiate between forensic, involuntary, and voluntary reasons for hospitalization. Accordingly, the study presented here aimed to examine the relationship between the reason (forensic, involuntary, or voluntary) for a first psychiatric hospitalization and the course of hospitalization for schizophrenia, controlling for age at first hospitalization and sex, which have been shown to predict outcomes in schizophrenia (
5,
8 ).
Methods
The Israeli National Psychiatric Case Registry contains a complete listing of all psychiatric hospitalizations in Israel, and it also includes the ICD-9 diagnoses assigned at admission and discharge by an Israeli medical board-certified psychiatrist. Diagnoses recorded in earlier ICD codes are routinely updated by the registry. All psychiatric inpatient admissions to and discharges from psychiatric hospitals in Israel, including those to nonpsychiatric hospitals, are required by law to be reported by the facility to the registry. Reporting is monitored by a special department at the Ministry of Health that verifies reporting compliance, information reliability, and correctness and completeness of registry data.
Registry diagnoses have shown acceptable levels of sensitivity and specificity, when measured against research diagnoses (
9 ), and they have shown acceptable diagnostic stability over time (
10 ). Accordingly, we used a follow-forward study design (
11 ) with data from the National Psychiatric Case Registry to identify all first and subsequent psychiatric hospitalizations among persons with schizophrenia disorders, including schizophreniform disorder, schizoaffective disorder, schizotypal personality disorder, delusional disorders, and nonaffective psychoses. Admission status information (forensic, voluntary, or involuntary admission) was available for the first and second admission. This study received local institutional review board approval.
The population consisted of all 12,071 persons (7,242 males, or 60%, and 4,829 females, or 40%) with a first admission to an Israeli psychiatric facility with a diagnosis of schizophrenia disorders (
ICD-9 295) from 1978 to 1992 who maintained this diagnosis at their last registry entry (
5 ). Removal of cases with missing data left 10,591 cases with complete information available for analysis. The cohort was followed in the registry through 1996 for additional hospital admissions and death. Death dates were included in the data by the Ministry of Health, which accessed this information from the Ministry of the Interior where all deaths are officially recorded. The data are detailed elsewhere (
8 ).
The hospitalization outcomes derived for this analysis included age at first hospital admission, length of first stay, average number of days hospitalized per year, whether the person had more than one hospital admission, and the number of hospital admissions per illness year. For the 745 persons (6.2%) who died during the study period, variables were censored with the death date. The calculation and description of these hospitalization outcomes has been documented more comprehensively elsewhere (
8 ).
Among patients with a second admission (N=7,281), we conducted a series of chi square tests to examine the relationship between admission status (voluntary, involuntary, or forensic) at the first and second admission. To examine differences in first admission status we used analysis of variance (ANOVA). To predict the hospitalization outcomes we used multivariate analysis of covariance (MANCOVA) and entered the hospitalization outcomes as the dependent variables. Predictors in the MANOVA included age at first hospitalization and first admission status as a factor, with voluntary admission as the reference category. Binary logistic regression modeling was conducted to predict whether a patient had more than one admission as a function of age at first hospitalization and first admission status. The analyses controlled for age at first hospitalization and sex, because they have been shown to predict outcomes in schizophrenia research (
8,
12 ).
Results
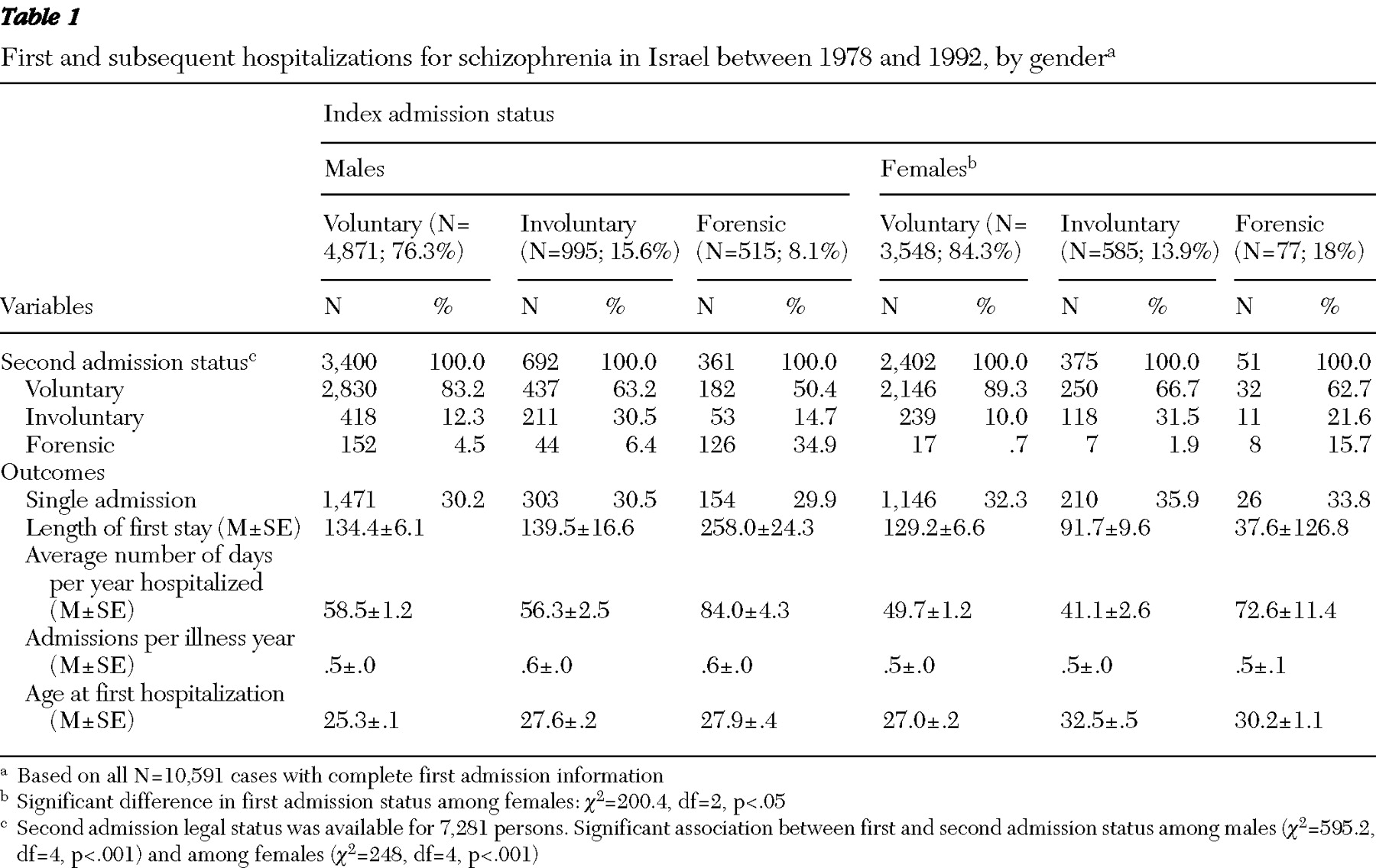
The descriptive statistics showed that a higher proportion of males than females had forensic admissions (87% versus 13%). The association between first and second admission status was examined. This association was considered clinically relevant because it provides information about whether the patient was consistently seen as dangerous (
5 ). There was a significant association between first and second admission status among males and females (
Table 1 ). The transition patterns from first to second voluntary and involuntary admissions were similar for men and women. However, 34.9% of men compared with 15.7% of women repeated their first forensic admission with a second forensic admission.
To examine the relationship between first admission status and age at first hospitalization ANOVAs were conducted for each sex. ANOVAs indicated that irrespective of sex, the voluntary first admission group had the youngest age at first hospitalization, compared with the other two admission groups (males: F=53.17, df=2 and 6,378, p<.001; females: F=83.13, df=2 and 4,207, p<.001). Post hoc tests indicated that the involuntary and forensic groups did not differ in age at first admission.
To examine the relationship between admission status and hospitalization outcomes, MANCOVA was conducted independently for each sex, controlling for age at first hospitalization, which was a significant predictor across outcomes. Among males and females a forensic first admission predicted a higher average number of days hospitalized per year (males: β =29.54, t=7.79, p<.01; females: β =26.69, t=3.31, p<.01) and a longer length of first stay (males: β =134.74, t=6.38, p<.01; females: β 217.71, t=4.74, p<.01). Among males, but not females, a forensic first admission was significantly associated with more admissions per illness year ( β =.06, t=3.07, p<.01). Binary logistic regression was conducted to examine whether type of first admission was associated with whether a patient had more than one admission, but findings were not statistically significant, irrespective of sex.
Together these findings generally highlight the prognostic value of forensic first admission status, rather than involuntary first admission status, after adjusting for age at first hospitalization. This was found to be true slightly more so among males than females. To control for differences in follow-up times, the analyses were repeated for those with only ten years of follow-up data, and the results showed a similar trend.
Discussion
This study used population-based data to examine the relationship between first admission status and hospitalization outcomes, controlling for age at first hospitalization and sex. This study is the first to compare short- and long-term hospitalization outcomes for persons with forensic, voluntary, and involuntary first admissions. A significant relationship was found between first and second admission status.
The results also suggest that although the groups with first forensic and first involuntary admissions do not significantly differ by age at first hospitalization, a forensic first admission has long-term prognostic utility, after controlling for the age at first hospitalization. This finding is slightly more consistent among males than females. Possible reasons include that, compared with women, men are more likely to begin offending at a younger age (
13 ) and have an earlier onset of psychotic symptoms, and so generally may not attain as many social skills prior to onset (
8 ). A tentative reason, therefore, is that females achieve better premorbid social functioning, compared with males, which results in a less severe onset. Thus these findings corroborate other schizophrenia research indicating that males have poorer outcomes than females (
8,
12 ). Collectively, this suggests that among males and, to a lesser extent, females, having a forensic first admission is a risk factor for poorer hospitalization outcomes, which provides long-term incremental information beyond age at first admission.
Probable reasons for longer first hospitalizations for patients with a forensic commitment are that many may have committed a violent crime and thus may be serving criminal sentences in the hospital or there may have been a reluctance to release them into the community because of their dangerousness. These reasons, however, do not adequately explain why those with a forensic admission had a longer average number of days per year hospitalized, which may be a better index of symptom severity. Nonetheless, this highlights the predictive utility of forensic first admissions among males and females.
This study has some limitations. As in other registry studies, readmission rates were used as an outcome, because there were no clinically based measures of symptom severity. Also, because symptom severity was not known, it was not possible to examine whether persons with involuntary admissions had more severe symptoms. Accordingly, it was not possible to ascertain whether all psychiatric hospitalizations among persons with a diagnosis of schizophrenia were directly attributable to symptomatic exacerbation of schizophrenia.
Future research should examine illness outcomes by using direct measures of symptomatology. Such measures are not available in this study and are relevant because readmission may vary by factors such as symptom severity and functional outcomes.
Future research should also examine the relationship between need for involuntary treatment and lack of insight, nonadherence to treatment, substance misuse, and violence. The lack of significant effects among females for more admissions per illness year may be attributable to the small number of females in the forensic first admission group. An alternative explanation is that females are older than males when they experience their first forensic admission and when they experience the onset of psychiatric symptoms. Thus the better premorbid functioning of females is associated with better outcomes, compared with those of males.
It is difficult to extrapolate these findings to other countries, because the Israeli population may be in some respects more homogeneous than those of large nations. Nevertheless, Israel is a country of immigrants reflecting many cultures, and the reasons for admission here resemble those in other countries. Also, service use in this study, which is a proxy measure of the course of illness, can be influenced by external factors, such as bed availability. However, during the study period the health system was hospital based, free and equal to all, and relatively stable, irrespective of location (
8,
14 ). During the past decade the mental health system has been in flux with the reform of the health care system.
Despite the limitations of this study, it has several strengths, including the use of a high-quality data set compiled independently of the hypotheses, documented psychiatric admissions, a population-based sample, and a considerable follow-up period; and it was conducted during a period when free and equal access to health services were offered to all residents of Israel.
Conclusions
The results presented here suggest that greater attention should be paid to patients who are hospitalized for the first time and have a forensic admission, because they are at increased risk for poor outcomes. The results show that although age at first admission for persons with forensic and involuntary admissions did not differ, among males a first forensic hospitalization for schizophrenia is a particularly robust risk factor that provides prognostic utility in addition to age at first admission. This study is the first population-based demonstration that a first forensic admission, a proxy variable of dangerousness, has prognostic value.
Acknowledgments and disclosures
Dr. Levine was supported by a grant from the Israel Foundations Trustees from 2008 to 2009.
The author reports no competing interests.