Population surveys have reported that even after adjustment for illness severity, between 35% and 50% of respondents who meet criteria for a mental or substance use disorder do not seek services (
1,
2,
3,
4,
5,
6 ). Other than objective indicators of need, there are numerous perceptual, attitudinal, predisposing, and enabling factors that influence the decision to seek care (
7 ). Those who report a need for help but do not go on to seek services are of particular interest, because perceptions of unmet need may influence health outcomes, attitudes toward health care, and future help-seeking behaviors. Such perceptions are associated with many of the same factors associated with help seeking, including diagnoses of other illnesses, mental health status, disability, and distress (
8,
9,
10,
11,
12 ). In a study of general medical care, unmet needs were related to patients' levels of mistrust and lack of confidence in physicians (
13 ).
The most commonly reported reasons for not seeking mental health care in relation to a perceived need include opting to self-manage symptoms or to work through them without professional help (
8,
9,
12,
14,
15,
16 ). The motivations behind these reasons are unclear. The decision to self-manage may be based on beliefs of general ineffectiveness of mental health care, negative attitudes toward providers, stigma, financial and other systemic barriers to access, or other factors. Wu and colleagues (
17 ) observed that not being ready to stop drinking was the most commonly reported reason for not seeking treatment among young adults with alcohol use disorders (47%). Other common reasons included financial barriers (19%) and stigma (18%).
An understanding of the factors that contribute to unmet needs is essential to prevent potentially negative health and economic outcomes associated with delays and failures to obtain required care. The dearth of empirical research on this topic has been noted elsewhere (
18 ). In a previous analysis, we found that individuals with co-occurring mental and substance use disorders reported twice the prevalence of perceived unmet need for care as those with either disorder alone (
8 ). They also reported greater distress and were more likely to have used services, although they were less satisfied with their care and less likely to perceive it as helpful. Inasmuch as those with co-occurring disorders are more likely to seek care, it is possible that they are more likely to encounter difficulties and, in turn, report unmet need. Other work has supported the notion that perceived unmet needs are more common among service users than nonusers (
9,
19 ).
This analysis builds on previous work by examining the associations between diagnoses and perceived unmet need. It takes into account the individual's level of recent exposure to the health care system and potential predisposing, enabling, and need factors often associated with help seeking. In addition, comparisons are made across sole-disorder and co-occurring disorder groups in the self-reported reasons underlying unmet needs.
Methods
Sample
Participants were respondents to the Canadian Community Health Survey (CCHS) Cycle 1.2 (N=36,984). The CCHS is a cross-sectional population health survey conducted biennially by Statistics Canada. Cycle 1.2, conducted in 2002, focused on mental health and well-being and was the first attempt to generate national estimates of the burden of mental illness in Canada. The target population included all noninstitutionalized adults 15 years of age and older living in the ten Canadian provinces, excluding those on Crown lands and military bases. A multistage stratified cluster design was used to generate the sample. The response rate was 77%. The final sample was weighted to correspond to the general population of Canada (approximately 24 million). A detailed description of the survey is available elsewhere (
20 ). This research was approved by the institutional review board at the Centre for Addiction and Mental Health in Toronto, Canada.
Measures
Perceived unmet need for mental health or addiction-related care was defined as a positive response to the following question: "During the past 12 months, was there ever a time when you felt that you needed help for your emotions, mental health, or use of alcohol or drugs, but you didn't receive it?" Respondents who endorsed this item were asked to state the reasons why care was not obtained.
The diagnostic content was based on the World Mental Health Composite International Diagnostic Interview (
21 ), which uses the categories of the
DSM-IV (
22 ). Diagnostic algorithms were available for five mood and anxiety disorders diagnosed in the past year: major depression, manic episodes, panic disorder, social phobia, and agoraphobia. Respondents were classified as positive for substance dependence if they reported having three or more symptoms in the past year (
21 ).
The analysis focused on those who met criteria for one or more disorders in the year before the survey (unweighted N=4,052/36,984). Respondents were classified into one of three diagnostic groups: substance dependence only (2.1% of the full sample, 20.8% of the diagnostic subsample), mental disorder only (7.4%, or 70.3% of the subsample), and co-occurring substance dependence and mental disorder (.9%, or 8.9 % of the subsample).
Substance abuse, psychosis, and personality disorders were not assessed in the survey. Although this exclusion results in an underestimation of the burden of mental illness in Canada, the mental disorders covered in the survey are among the most prevalent in the general population. The decision to exclude substance abuse from the survey is unfortunate; however, issues such as disability, perceived need for services, and help seeking are likely to be more closely related to the more severe dependence category (
23 ).
Two variables were included to adjust for variance in exposure to the health system across diagnostic groups; exposure was previously found to be a significant predictor of unmet need. Respondents reported on their use of a wide range of mental health and addiction services in the year before the survey. Two summary variables were derived to represent any use of formal services (that is, community- or hospital-based care from health professionals) and informal services (that is, self-help or Internet support groups and help lines).
Several additional measures were selected that are known or expected to play a role in the help-seeking process (
7 ). Three predisposing variables were included: gender, age, and education (classified as secondary school completed or not completed, some postsecondary education, or postsecondary school completed). Two variables were identified as enabling factors: income adequacy and urban residence. Income adequacy was based on the total household income adjusted for household size: low if household income (in Canadian dollars) was less than $15,000 for one or two people, less than $20,000 for three or four people, or less than $30,000 for five people and middle to high if household income was greater. A category representing those who did not state their income (6.9%) was also included. Urban versus rural residence was differentiated on the basis of population density: a rural area is one with a population concentration of less than 1,000 and population density of less than 400 per square kilometer, discontinuous with an urban area, according to the Statistics Canada definition.
In addition to the diagnostic information, need for services was assessed with two dimensional measures of mental health status: a self-rating of general mental health ranging from poor, 0, to excellent, 4, and the K-10 measure of generalized psychological distress (range 0–40, with higher scores indicating greater distress) (
24 ).
Analysis
Multivariate logistic regression was used to examine the associations between perceived unmet need (yes, 1; no, 0) and diagnostic group (reference category: substance dependence only). Three sequential models calculated the odds of perceived unmet need by diagnostic group: first, unadjusted; second, adjusted for past-year service use; and third, adjusted for predisposing, enabling, and need variables. Differences in the self-reported reasons for unmet need were tabulated across diagnostic groups.
Population weights constructed by Statistics Canada were used to account for nonresponse and align the sample with the Canadian population. These weights were rescaled by their mean such that the weighted samples reported in the descriptive tables preserve the original sample size in addition to the weighting structure devised by Statistics Canada (the weighted N for the diagnostic subsample was 3,890). To account for complex survey design and potential for attenuated standard errors, parameter estimates were bootstrapped. The analysis was conducted with Wesvar 4.2 (
25 ).
Results
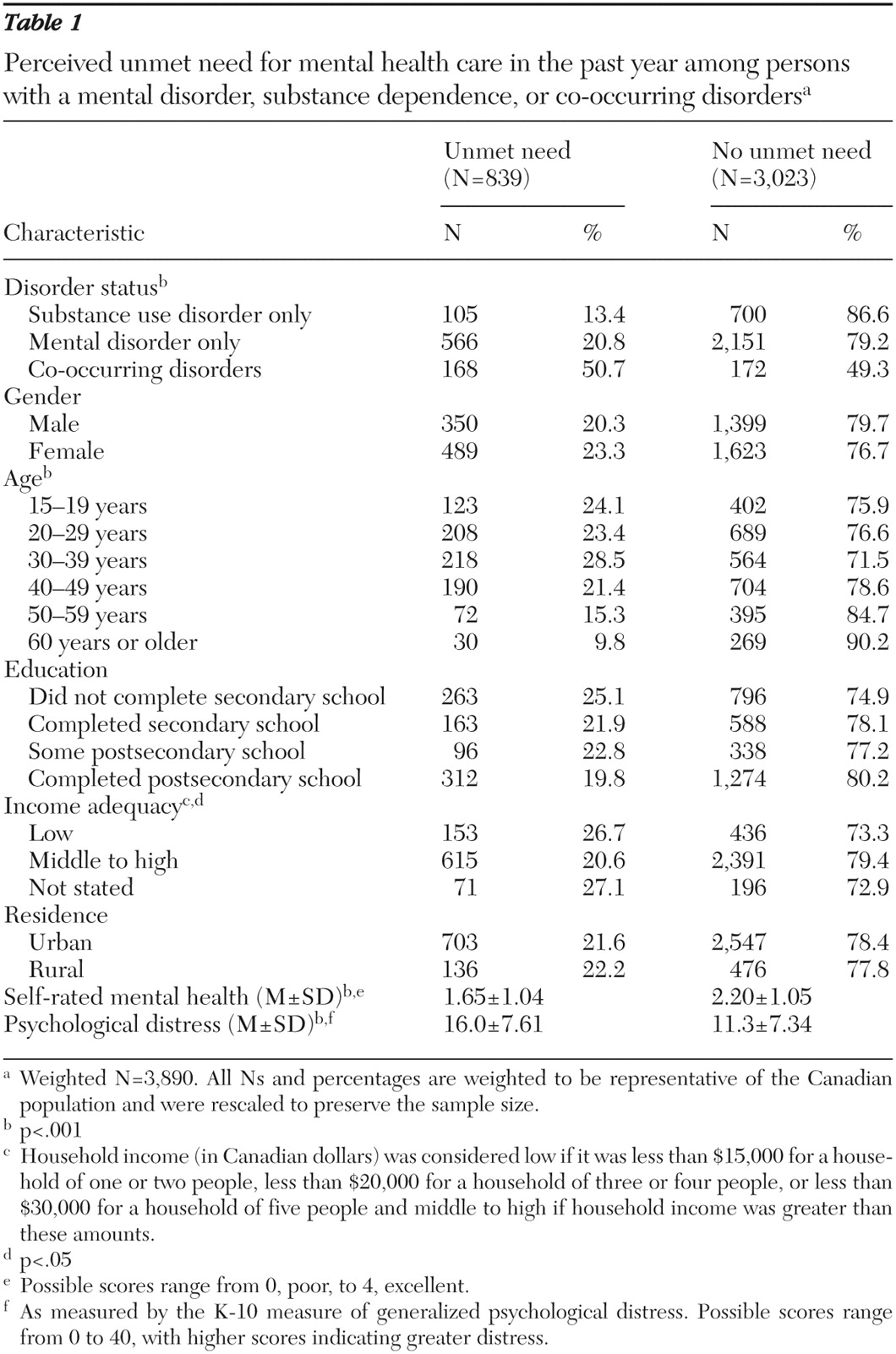
The prevalence of perceived unmet need among those who met criteria for a disorder was 22% (
Table 1 ). This varied from 13% of those with substance dependence only, to 21% of those with mental disorders only, and 51% of those with co-occurring disorders (
χ 2 =57.39, df=2, p<.001). Perceived unmet need was more common among younger adults, particularly those aged 30 to 39 years (
χ 2 =31.09, df=5, p<.001). Lower rates were reported by older individuals and those with middle to high income levels (
χ 2 =6.27, df=2, p=.043). In addition, those with perceived unmet need reported lower mental health status (t=9.73, df=500, p<.001) and greater levels of distress (t=-11.99, df=500, p<.001).
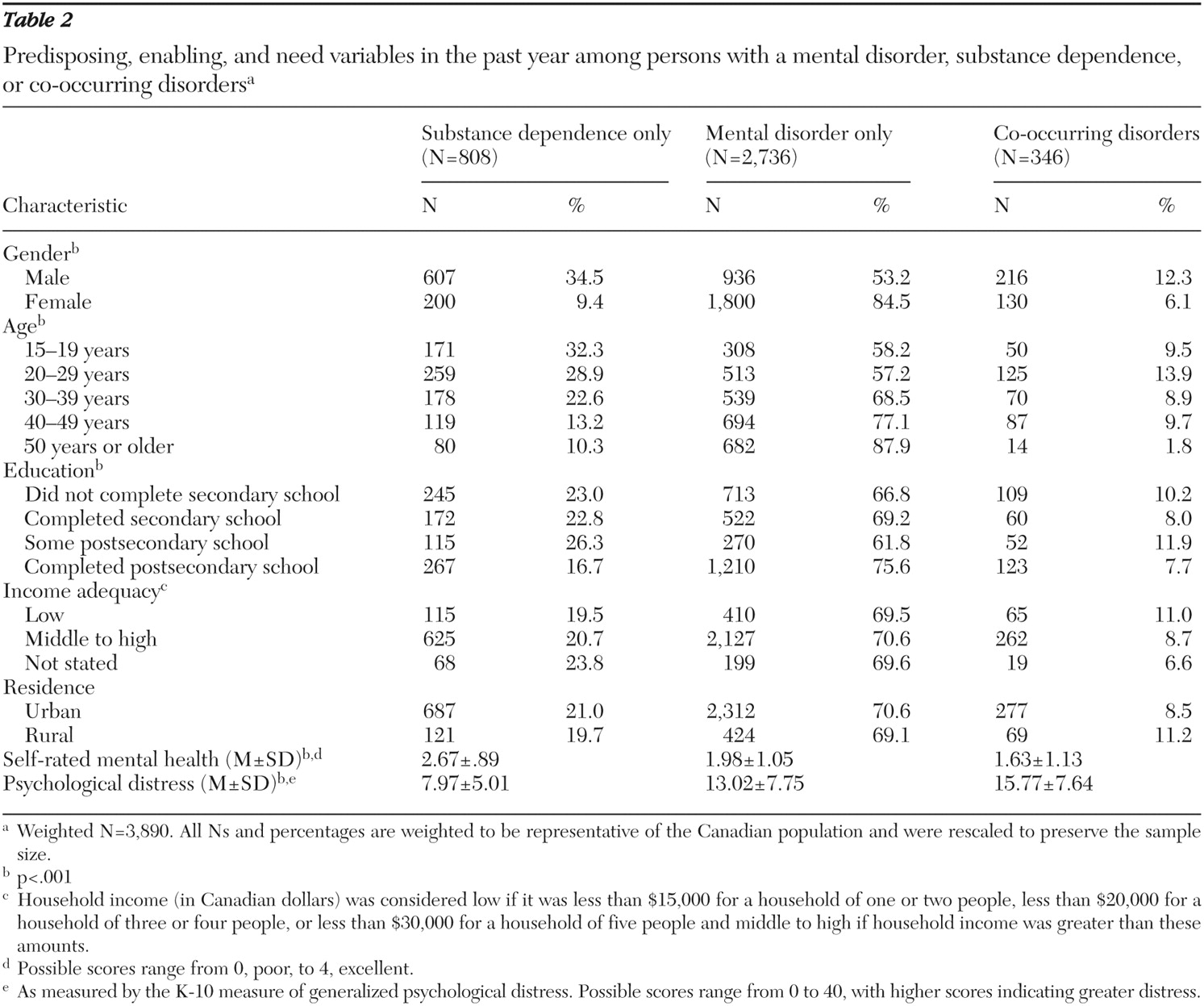
Table 2 presents these predisposing, enabling, and need characteristics by diagnostic group. Substance dependence, with or without a co-occurring mental disorder, was more common among men (
χ 2 =222.89, df=2, p<.001) and younger individuals (
χ 2 =132.64, df=8, p<.001), whereas mental disorders without co-occurring substance dependence were more common among women and older individuals. Persons with substance dependence alone or with co-occurring disorders were less likely to have a postsecondary degree, whereas those with mental disorders alone were slightly more likely than others to have a postsecondary education (
χ 2 =20.92, df=6, p=.002). Self-rated mental health was highest among persons with substance dependence and lowest among those with co-occurring disorders (t=-12.77, df=500, p<.001). Similarly, psychological distress was lowest among those with substance dependence and highest among those with co-occurring disorders (t=15.68, df=500, p<.001).
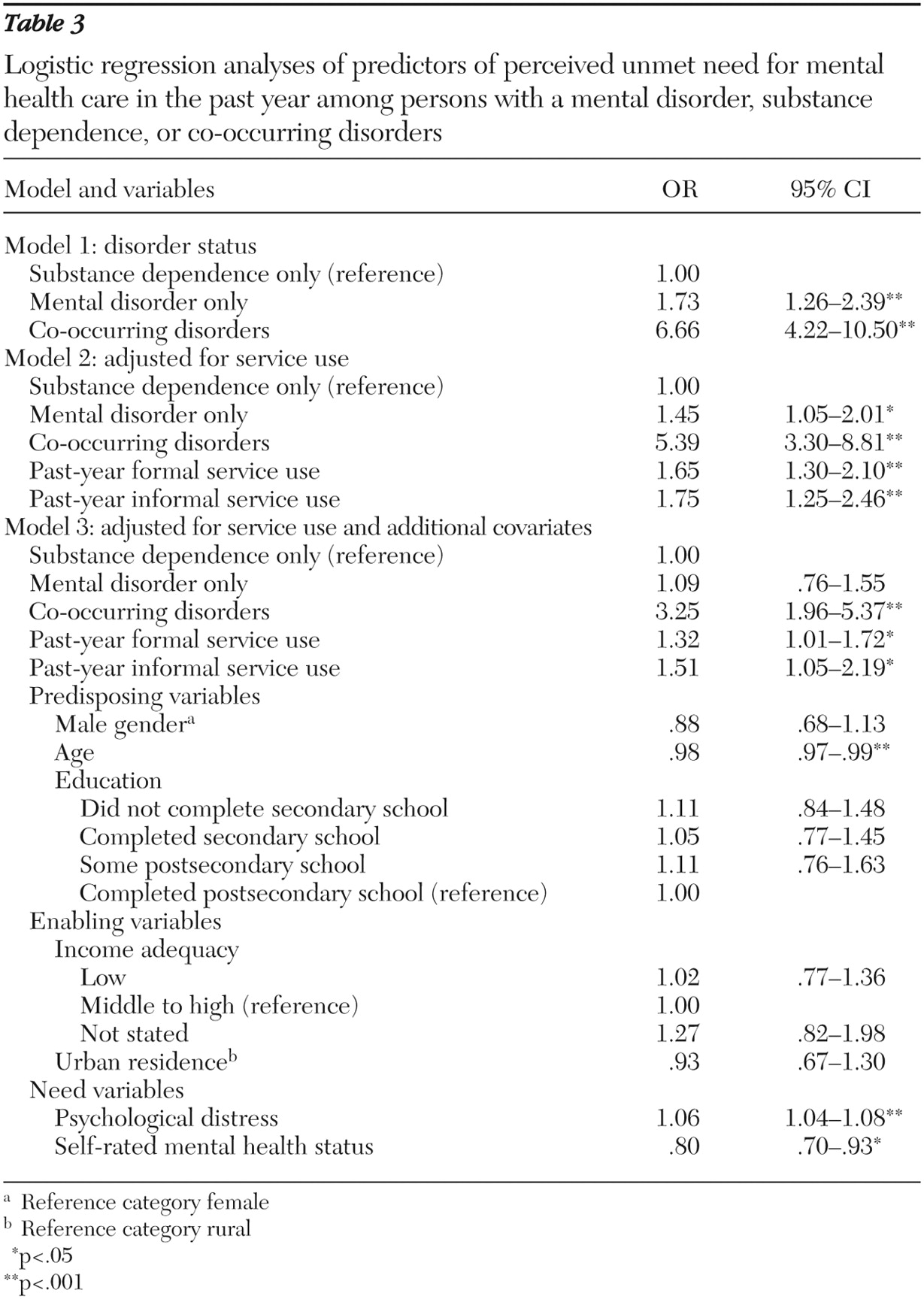
The odds of perceived unmet need were significantly greater among those with mental illness (odds ratio [OR]=1.73) or co-occurring disorders (OR=6.66) than among those with substance dependence (
Table 3, model 1). This effect was largely unchanged after adjustment for past-year service use (
Table 3, model 2).
The elevated odds of perceived unmet need among individuals with co-occurring disorders persisted after adjustment for predisposing, enabling, and need variables (model 3), although the adjusted OR was reduced by approximately half (adjusted OR=3.25). The odds of perceived unmet need were significantly greater among younger individuals (OR=.98) and those who reported greater distress (OR=1.06) and poorer mental health status (OR=.80). Gender, education, adequacy of income, and urban residence were not significantly associated with perceived unmet need in the full model.
Table 4 presents the distribution of respondents' reported reasons for unmet need across diagnostic group. Because of the small numbers of individuals in some of these categories, most differences were not statistically significant, although we found some interesting trends. A preference to self-manage symptoms was commonly reported across diagnostic groups. However, it was relatively more common among persons with substance dependence only. Those with substance dependence alone were also less likely to report that they did not know how to get help but were more likely to state that they were afraid to ask. Those with co-occurring disorders were more likely to report that they did not obtain care because they "did not get around to it" (30% versus 13%–16%;
χ 2 =8.37, df=2, p=.015) or that care was unavailable when needed.
Discussion
In conjunction with previous studies of mental health service use in this population, these findings highlight several issues and potential problems that individuals with mental and substance use disorders face in accessing services. More than one in five Canadians who met criteria for a 12-month mental disorder or substance use disorder—and fully half of those with co-occurring disorders—perceived an unmet need for mental health care in the year before the survey.
In Canada, hospitalizations and visits to most health professionals, including mental health and addiction services, are paid for by government health insurance plans that are regulated at the provincial level. The costs of pharmaceuticals are covered by personal or employer health insurance plans or are paid for by consumers out of pocket. Similar to the situation in most Western nations, primary care providers are typically the first point of contact in the system, and many, but not all, types of specialist mental health care require a physician referral. Most addiction services, on the other hand, do not require a physician referral. Previous work has noted that despite universal health insurance, the rate of specialist mental health care in Canada varies inversely with socioeconomic indicators (
26 ).
Findings from the multivariate analysis suggest that the greater level of perceived unmet need for mental health care among those with co-occurring disorders was largely unaffected by a greater likelihood of exposure to the health care system. It is, however, at least partially accounted for by additional variables related to help seeking, such as elevated psychological distress and poorer self-rated mental health. Because of the cross-sectional nature of the data, it was not possible to determine whether elevated distress and poorer mental health status contributed to a decreased ability to mobilize existing resources, which resulted in a perceived unmet need, or whether the perceived unmet need itself contributed to increased distress levels. Unraveling the causal connections between these factors remains an important area for future work.
It is important to note that after we adjusted for these factors, persons with co-occurring disorders still had approximately three times the odds of reporting unmet need relative to those with either type of disorder alone. Clearly, other factors must be identified to explain the higher perceived unmet need in this population. Because the outcome of interest is perceptual in nature, it is likely that additional perceptual measures, such as former experiences with mental health care and beliefs and attitudes related to mental health and mental health professionals will play an important role. Other potential explanatory factors include motivation for behavior change, availability of social supports, and the presence of co-occurring physical problems. To the extent that these additional factors influence help-seeking patterns and attitudes toward mental health and health care providers, they may also influence perceptions of need.
The different reasons for unmet need reported across the disorder groups provide interesting insight into consumers' perceptions and experiences of the mental health and addiction treatment system. Most of these findings were not statistically significant, however, and therefore warrant further investigation with larger samples. Fewer persons with substance dependence than those in the other two diagnostic groups did not know where to get help, which may be related to the high profile and availability of groups such as Alcoholics Anonymous and Narcotics Anonymous. The higher prevalence of preferring to self-manage symptoms and being afraid to ask for help among those with substance dependence may reflect greater stigmatization of the disorder and seeking care, or it may indicate low motivation and unreadiness to change substance-using behaviors (
17 ). In another study of perceived unmet needs, a diagnosis of substance use disorder increased the odds of reporting embarrassment as a barrier to seeking required care (
12 ). Given the higher proportion reporting a preference to self-manage symptoms, it is equally possible that substance dependence, as experienced in the general population, is not experienced as a disorder for which treatment is perceived to be required.
The relatively higher prevalence of "not getting around to" seeking care among persons with co-occurring disorders (a statistically significant finding) may similarly reflect issues of stigma, embarrassment, or low motivation to change substance-using behaviors. Given previous analyses of these data in which persons with co-occurring disorders were more likely to have sought services in the year before the survey and were more likely to be dissatisfied with these services (
8 ), it is possible that satisfaction with the care received in prior treatment episodes affects the individual's desire to further seek services. Other research has found that individuals with multiple mental disorders have more serious problems in several life areas (
1,
27,
28 ), which may suggest that these individuals face greater challenges in managing illness burden and mobilizing available resources for help. The data do not allow for a direct analysis of these hypotheses, which therefore remain important areas for further work.
Persons with co-occurring disorders also were more likely to report that care was unavailable when needed. Although this result might be due to factors at the individual level (for instance, a lack of knowledge about services), it may also indicate a lack of preparedness of the health care system to deal with co-occurring diagnoses. Systemic, structural, and attitudinal barriers to effective interventions with this subpopulation are commonly cited by clinicians and administrators (
29,
30,
31 ). Given the central role of general practitioners in treating those with mental health and addiction problems in Canada (
8,
32 ) and elsewhere (
1,
4,
33,
34 ), the potential for shared care approaches with addiction and mental health professionals should be explored further.
Two reasons (preferring to self-manage symptoms and not getting around to seeking help) accounted for half (45%–55%) of the perceived unmet need across diagnostic groups. Given the nature of these reasons, this may suggest that many individuals did not have disorders that were sufficiently severe to require treatment. Mechanic (
35 ) noted that a self-reported desire to self-manage symptoms and distress should be interpreted to indicate the absence of a perceived need for care. It is therefore relevant that in this study perceived unmet need was identified by the respondents themselves, who were explicitly directed to consider occasions when care was perceived to be needed but was not sought. In this sense, our definition does not impose restrictions on the reasons for not obtaining care, nor does it specify that these must be externally mediated. That such a large proportion of respondents went on to cite internal or attitudinal reasons for not obtaining care is an interesting finding in and of itself. A preference for self-managing symptoms or not getting around to seeking help may, but does not necessarily, imply a disorder of lower severity or an absence of real need. It may equally indicate the presence of significant barriers to access or fears of stigma and embarrassment associated with help seeking for mental health or addiction.
Given that the data are cross-sectional, it was not possible to determine causal relationships between the experience of disorders, use of services, unmet need, and the potential impact on prognosis. It also was not possible to identify the specific disorder that initiated help seeking or resulted in the unmet need or to empirically examine the role of provider factors in these processes. Diagnosis and caregiver biases likely have implications for service use and unmet needs.
Conclusions
Notwithstanding these limitations, this work adds to a small but growing literature on the correlates of unmet needs. By incorporating perceptions, we have moved beyond overly simplistic methods used in previous work on this topic, such as the presence of diagnoses. Consumer perspectives represent a central concept within need for mental health care, along with disease burden or objective need, availability of treatment, and clinical judgment (
36 ). To understand need in its entirety, a clear appreciation of the determinants of consumer perceptions is essential (
18 ). Other recent work is available that assessed the population prevalence and correlates of unmet need for mental health care using objective indicators, such as disability-adjusted diagnoses (
6,
37 ) and clinician-evaluated need for care (
38 ). These studies have similarly reported that a large proportion of need for mental health care, between 50% and 70% with differing definitions, goes unmet.
Moreover, the results of this analysis clearly indicate the need to consider specific diagnostic subgroups, particularly those with co-occurring substance dependence and mental disorders, when examining issues of unmet need. The elevated occurrence of perceived unmet need in this group is relatively less affected by contact with the health care system than by other conceptualizations of generalized distress and problem severity. Further research is needed to more fully elucidate the impact of co-occurring disorders on service use, including the role of satisfaction with previous care and occasions of perceived unmet need in future help-seeking behaviors.