In recent years, although there has been an increasing social acceptance of mental disorders such as depression and eating disorders, this has not been the case for schizophrenia (
1 ). [Additional references are available as an online supplement at ps.psychiatryonline.org.] In several contexts, people with this disorder are still viewed as unpredictable, aggressive, and dangerous (
2,
3 ). The common opinion that schizophrenia is "different" from any other physical and mental disease implies higher levels of discrimination by affected people in social and occupational roles (
4 ), delays in access to appropriate treatments, and obstacles to being able to achieve life goals.
Stigma against persons with schizophrenia has been rarely investigated from the perspective of patients themselves (
2,
5,
6,
7 ). This is probably related to the beliefs that these persons are not reliable in providing information on their own condition and are fickle in their opinions (
8 ). Consequently, the personal experience of persons with schizophrenia has rarely been taken into account in planning sensitization campaigns and educational programs for target populations and in allocating resources for mental health care (
8 ). In addition, despite a growing consumer movement (at least in the United States [
9 ]), persons with schizophrenia are rarely involved in designing surveys on their own disorder and do not usually have access to study results (
8,
10 ). In fact, most studies have involved patients only in the initial phase (consultation studies) (
3,
8 ), and only a few have pulled together researchers' technical competencies and patients' personal experiences throughout all research phases (participatory research) (
5,
8 ).
Since the late 1970s the Italian mental health policy has been strongly community oriented. The long-term contact between people with mental disorders and the general population may have had a significant impact on patients' beliefs about their own disorder, as it has had on lay people (
11 ). However, up to now, no study has specifically explored the effect of community mental health care on patients' opinions about schizophrenia in this country.
In 2005, on the basis of previous studies of representative samples of professionals, patients' relatives, and the general population (
11 ), we carried out a participatory survey on the opinions of patients with schizophrenia about the causes of their disorder, the usefulness of treatments, and the social consequences of their own mental disorder. The study, conducted in collaboration with patients attending ten Italian mental health centers, included the following phases: development and validation of a self-reported questionnaire exploring patients' opinions of schizophrenia; evaluation of the beliefs about schizophrenia in a sample of 241 persons with schizophrenia; and presentation of the study results to the participants, in order to get their input about how to use the results for release and practical purposes.
In this brief report, we report results from the last two phases of the study (that is, evaluating patients' beliefs about schizophrenia and discussing with patients how best to use study findings). Data analyses were planned to test whether respondents' knowledge of their own diagnosis, their confidence that they will be well again, and their perception of being limited in their own life because of the disorder were related to sociodemographic and clinical variables or to their opinions about the social consequences of schizophrenia.
Methods
The study was carried out at the Department of Psychiatry of the University of Naples SUN; at the mental health centers of Arezzo, Campobasso, Battipaglia, Ferrara, Ravello, Rho, Torino, and Trieste; and at the Fatebenefratelli Institute of Brescia.
In each center, 25 patients with schizophrenia were consecutively recruited if they met the following criteria: between 18 and 60 years of age, no hospital admission in the previous three months, at least one psychotic episode in the previous five years, and current treatment with antipsychotic drugs. Each individual was asked to complete the Users' Opinions Questionnaire (UOQ).
After a complete description of the study was given to the participants, written informed consent was obtained. Data were collected from May 2005 to February 2006.
From November 2006 to February 2007, a workshop was conducted in each center to present the results of the study to patients and staff and to collect suggestions on how to use them.
The study protocol was approved by the reference review board of the Second University of Naples, Faculty of Medicine.
The UOQ is a self-report questionnaire developed through focus groups with patients with schizophrenia and with mental health professionals (
12 ). The instrument includes 24 items grouped into six subscales, exploring the respondent's opinions about the usefulness of drug and psychosocial treatment, affective problems (that is, difficulties that persons with schizophrenia may experience in family and affective relationships and in caring for children), social distance (that is, feelings of being excluded and being perceived as dangerous because of mental illness), right to be informed, recognizability (that is, feelings of being identifiable by other people as mentally ill), and social equality (that is, perception of the likelihood of recovering and of being treated like other people). Each item is rated on a 3-point scale, from 3, completely true, to 1, not true; there was also an "I don't know" answer, which was given a score of 5. Possible scores range from 24 to 72, with higher scores indicating a higher level of agreement.
Moreover, the questionnaire includes 12 open-ended questions on topics covered by the above items and on the respondent's opinions on the causes of his or her own mental disorder, knowledge of his or her own diagnosis, opinions on the possibility of recovery, and perception of personal limitations resulting from schizophrenia. The psychometric properties of the UOQ have been formally tested and found to be satisfactory (intrarater reliability: Cohen's kappa coefficient ranged from .55 to .92; Cronbach's alpha coefficient, performed on the six subscales, ranged from .55 to .74; factor analysis accounted for 53% of total variance).
Statistical analysis was focused on the following variables: respondents' knowledge of the diagnosis of schizophrenia, respondents' perception of personal limitations resulting from the disorder, and respondents' confidence that they would be well again. These variables were explored in relation to sociodemographic and clinical variables and respondents' opinions about the social consequences of schizophrenia, using analysis of variance or the chi square test, as appropriate. A logistic regression model was used to test the simultaneous effects of the sociodemographic and clinical variables and of respondents' opinions about social consequences of schizophrenia on each of the above-mentioned variables (dependent variables)—that is, knowledge of diagnosis, perception of personal limitations, and confidence of recovery. Independent variables were included in the logistic model only if they had reached a statistical level of p<.01 in the univariate analysis.
Results
Of the 250 patients with schizophrenia approached to participate in the study, nine (4%) refused, leaving a final sample of 241. The mean±SD age of the sample was 39.4±9.6 years. A total of 149 (62%) were male, 181 (75%) were single, 65 (27%) were employed, and 111 (46%) had completed an eight-year school degree (equivalent to completing junior high school). The mean duration of illness was 15.6±10.3 years, and 63 (26%) had previous suicide attempts. All patients were being treated with antipsychotic drugs. Ninety-two patients (38%) were receiving individual psychological support, 140 (58%) were participating in social group activities, and ten (4%) were participating in a vocational skills program.
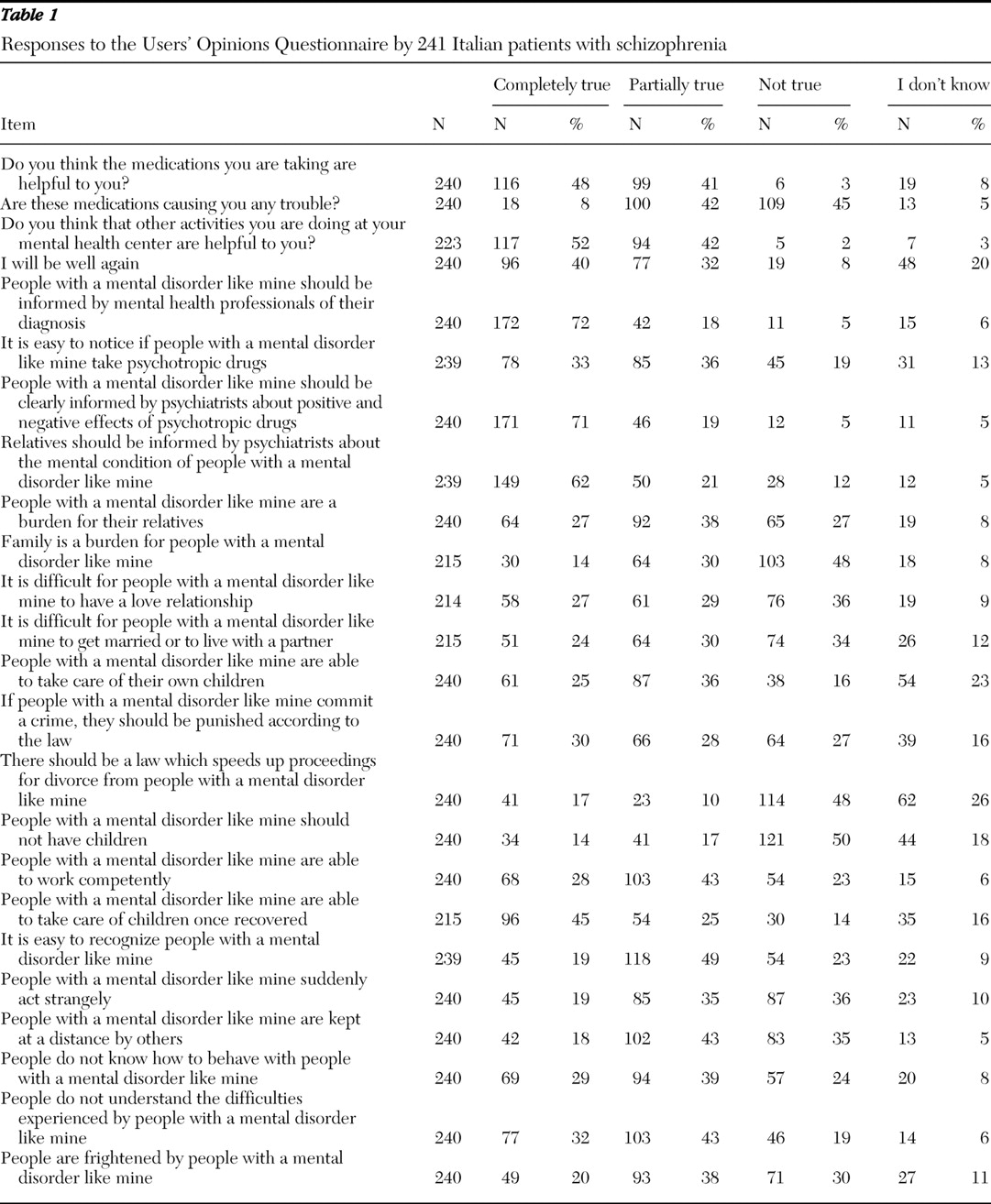
Seventy-two respondents (30%) reported they had been informed by psychiatrists that they have schizophrenia. As shown in
Table 1, most of them maintained that psychiatrists should provide patients with information on their mental disorder and its treatments. The closed-ended questions showed that 163 (68%) found that it is easy to recognize persons treated with psychotropic drugs, and 118 (49%) complained about side effects of medications. Among the 122 respondents who answered the related open-ended question, the most frequently reported side effects were drowsiness or tiredness or feeling dazed (74 patients, or 61%) and weight gain (18 patients, or 15%).
From the closed-ended questions, we found that 163 of 239 respondents (68%) thought that it was completely true or partly true that persons with schizophrenia are easily recognizable. By using the open-ended questions, we found that 163 respondents thought these persons were easily recognizable because of their behaviors (59 patients, or 36%), movements (30 patients, or 18%), appearance (28 patients, or 17%), speech (20 patients, or 12%), and walking style (16 patients, or 10%).
From the closed-ended questions, we found that persons thought it was completely true or partly true that it is difficult for persons with schizophrenia to have a love relationship (119 of 214 persons, or 56%) and to get married or live with a partner (115 of 215 persons, or 53%). A total of 150 of 215, or 70%, expressed the opinion that persons with schizophrenia are able to take care of their children once recovered, but 75 of 240 persons, or 31%, stated that they should not have children.
From the closed-ended questions, we found that 96 of 240 respondents (40%) reported that they believe that it is completely true that they will be well again. Compared with those who did not report this belief, they had a shorter duration of contact with mental health services (72.6±62.8 months versus 107.1±82.6 months; F=10.5, df=1 and 188, p<.01) and a less pronounced perception of affective difficulties attributed to the illness (UOQ score of 1.6±.5 versus 1.8±.5; F=6.5, df=1 and 189, p<.01) and social distance attributed to the illness (UOQ score of 1.8±.6 versus 2.0±.5; F=6.8, df=1 and 189, p<.01). Logistic regression revealed that respondents' conviction to recover was predicted by a shorter duration of contact with mental health services ( β =–.006, p<.001; χ 2 =18.4, df=3, p<.001).
Ninety-two respondents (38%) felt that their mental problems did not limit their personal life. Among the 146 of 238 respondents (61%) who felt limited in their personal life as a result of schizophrenia, 51 (35%) pointed out limitations in work or study activities, 38 (26%) reported problems in having an independent life (such as planning daily activities or performing household duties), 31 (21%) reported problems in social life (such as participating in social and sports activities or going to bars or pubs), and 29 (20%) reported limitations in planning their own future (such as having a "normal life"). Furthermore, 18 respondents (12%) reported affective limitations (for example, in maintaining a stable love relationship, getting married to someone, or having children).
The respondents who perceived being limited in their own life as a result of schizophrenia were more likely to be unemployed (116 of 146 patients, or 79%, versus 58 of 91 patients, or 64%; χ 2 =7.1, df=1, p<.01) and were more likely to have previously attempted suicide (51 of 147 patients, or 35%, versus 12 of 92 patients, or 13%; χ 2 =13.7, df=1, p<.001). In addition, these respondents acknowledged higher levels of social distance (UOQ score of 2.1±.4 versus 1.7±.5; F=35.3, df=1 and 235, p<.001), inequality (UOQ score of 1.9±.5 versus 1.5±.4; F=32.7, df=1 and 235, p<.001), and affective difficulties (UOQ score of 1.9±.5 versus 1.6±.4; F=24.7, df=1 and 235, p<.001) as a result of the illness, and they expressed more skepticism toward the usefulness of available treatments (UOQ score of 2.3±.4 versus 2.6±.4; F=28.4, df=1 and 236, p<.001). By using logistic regression, we found that the respondents' conviction that they were limited in their personal life as a result of schizophrenia was associated with higher levels of perceived social distance ( β =–.9, p<.02) and inequality ( β =–1.0, p<.005) and more skepticism toward the usefulness of treatments ( β =1.7, p<.001; χ 2 =75.8, df=6, p<.001).
The study results were presented to a total of 183 persons, including 123 patients, 46 professionals, and 14 relatives or volunteers. During the meetings, 60 persons provided feedback on how to use study results, of which 40 (67%) were patients. Thirty-six (60%) participants suggested that the results should be used as a starting point to design educational group sessions on the clinical characteristics and management of schizophrenia. Eighteen participants (30%) maintained that the study results should be shared with other patients and professionals. [Suggestions about the use of the study results are available as an online supplement at ps.psychiatryonline.org.]
Discussion and conclusions
This survey is the first collaborative effort carried out in Italy that set out to gather and make use of the rich information that individuals with schizophrenia can share with professionals as active participants in their care.
In some centers, the study has led to a constructive debate between patients and professionals on the practical consequences of schizophrenia and on patients' empowerment. In others, it has prompted the organization of educational groups on topics such as mental health care, clinical characteristics of schizophrenia, pharmacotherapies, and coping strategies for daily life difficulties.
The use of a self-report questionnaire available in different versions could facilitate the replication of this experience in other contexts and allow for a comparison of opinions on schizophrenia in different target populations (11).
Although the study sample was quite large, it was not a probability one, and it may not be representative of the population of persons with schizophrenia receiving community care in Italy. The lack of a control group with other mental disorders is a further limitation (
4 ). Moreover, the UOQ has been validated in only one study and relies on self-report.
Only 30% of the respondents reported that they had been informed by their psychiatrists of having schizophrenia. This finding, in line with previously published data (13), probably reflects the common belief of psychiatrists in the United States and other developed countries that communication of the diagnosis of schizophrenia could be frightening or demoralizing for patients and relatives (14). This attitude is likely to be perceived by patients as further evidence that schizophrenia is unavoidably a severe and untreatable disease, thus contributing to their withdrawal and skepticism toward treatments. We cannot exclude the possibility, however, that some respondents had been informed of their diagnosis but had not retained that information.
As outlined by patients attending the meetings on study results, the discovery of the diagnosis of schizophrenia by reading a clinical report may be a stressful experience. However, receiving clear information on schizophrenia from professionals may increase trust in therapies and facilitate the adoption of effective coping strategies (
5,
15 ).
Forty percent of the respondents expressed confidence that they will be well again. This percentage is significantly higher than the ones that we previously found in samples of relatives and professionals (10% and 2%, respectively) (
11 ). Maybe the meaning of the concept of "being well again" is understood differently by professionals and patients, and this discrepancy negatively affects patients' compliance with therapies and satisfaction with care (
9 ). Sixty-one percent of respondents felt they were limited in their life by their mental disorder. Unfortunately, the cross-sectional nature of this study and the structure of the questionnaire do not allow us to explore whether respondents' opinions on these issues are due to internalized self-prejudice or to concrete personal experiences.
Respondents agreed that it is difficult for persons with schizophrenia to have a love relationship (56%) or to get married or live with a partner (53%). This finding, which is consistent with previous reports (
4,
8 ), indicates that affective relationships is an area perceived as highly problematic by the patients. Interventions aimed at increasing patients' self-esteem and interpersonal skills are clearly needed to support them in the achievement of these emotional goals.
The closed-ended questions showed that 68% of respondents thought that persons with schizophrenia are easily recognizable, and a majority of these respondents felt that persons with schizophrenia can suddenly act strangely. These findings, which are consistent with those from a general population sample (
11 ), document that stigma and feelings of unpredictability are largely shared even by patients. These views are likely to negatively influence patients' social participation and achievement of life goals (
7 ).
As suggested by the participants, the results of this study are being used as a starting point in some of the participating centers to run a psychoeducational group intervention program on schizophrenia and its psychosocial consequences. Details on this ongoing program will be provided in forthcoming papers.
Acknowledgments and disclosures
This study was supported by grant 2-18-8 from the M. Lugli Foundation. The Users' Opinions Questionnaire Working Group includes the following mental health center professionals: Camillo Avino, M.D., Ada Orrico, M.D., Corrado De Rosa, M.D., Teresa Vitale, R.N., Generoso Troiano, R.N., Elisabetta Truglia, M.D., Franco Veltro, M.D., Carmela Coladangelo, M.S.W., Fabrizia Pizzale, L.C.P., Rosa D'Ambrogio, R.N., Carla Bachelet, L.C.P., Simonetta Canetti, L.C.P., Paola Zanus, M.D., Rosaria Pioli, M.D., and Silvia Bresadola, L.C.P. The authors thank Rosa Colacino, M.A., for her linguistic help in preparing the text. They also thank the heads of the participating centers who facilitated the conduction of the study: Matteo Forte, M.D., Ferdinando Pellegrino, M.D., Federico Perozziello, M.D., Aldo D'Arco, M.D., Giampiero Cesari, M.D., Francesca Fulgosi Cigala, M.D., Roberto Pasquino, M.D., Farida Ferrato, M.D., Carmine Munizza, M.D., Giuseppe Tibaldi, M.D., Ugo Zamburru, M.D., Giuseppe Dell'Acqua, M.D., and Paolo Maria Rossini, M.D. The authors are grateful to the 241 participating patients for their active involvement in the project.
The authors report no competing interests.