Racial and ethnic differences in patterns of service utilization for mental disorders, especially among disadvantaged groups, must be understood in order to address disparities in the United States and provide targeted prevention and intervention strategies. Previous large-scale epidemiologic studies of psychiatric disorders indicate that individuals in the black population are less likely than those in the white population to receive professional mental health treatment (
1,
2,
3,
4,
5,
6 ). In particular, persons who are black are less likely to receive treatment for mood and anxiety disorders, whether defined broadly as any professional treatment (
2,
4,
7 ) or specifically as talking with a mental health professional (
4,
8,
9 ) or using prescription medication (
8,
10 ). Fewer epidemiologic studies have examined racial and ethnic disparities in alcohol and drug treatment utilization, and results were inconsistent (
11,
12,
13,
15,
16,
17,
18 ) because of differences in measurement and design. Several studies were able to estimate racial and ethnic differences in service utilization among individuals with a particular alcohol or drug diagnosis in the general population. Among three U.S. samples of adults diagnosed with an alcohol disorder, two studies comparing a black group with others suggested no racial or ethnic differences in alcohol treatment (
19,
20 ), whereas one found no racial or ethnic differences overall but found less alcoholism treatment among black individuals with higher levels of alcohol severity (
21 ). Data from a general population sample indicated no overall racial or ethnic differences in drug treatment among individuals with a drug use disorder, although black and white populations were not specifically compared (
22 ).
As a theoretical framework to examine effects of race and ethnicity on service utilization, the Andersen behavioral model of health service treatment contact is the most extensively studied model of service utilization (
23,
24 ). This model posits that service utilization is a function of predisposing characteristics (such as gender, age, and race and ethnicity), enabling factors (such as income, education, health insurance, urbanicity or region, and having a regular source of care), and need for services (such as symptom severity, comorbidity, and perceived need for care). Although this model has received much theoretical attention, few nationally representative epidemiologic samples have empirically tested it. Moreover, small samples of respondents with a substance use disorder within racial and ethnic groups have limited the ability to detect effects or control for patterns related to relevant confounders. Studies that have applied the Andersen model in national samples found overall disparities for minority groups; differences within diagnosis remain unstudied (
25 ).
Although prior studies have identified disparities in treatment utilization, many aspects of racial differences in service utilization remain unclear. Mood and anxiety disorders and substance use disorders differ in their symptoms, appropriate treatments, and settings where treatment is provided. Whereas differences in service utilization for a specific diagnosis of depression are extensively documented (
2,
10 ), most studies examining treatment disparities collapse the outcome measure across all disorders, making it unclear whether black-white racial disparities are in the mood and anxiety domain or in the alcohol and drug domain. If category of diagnosis moderates racial and ethnic differences, this information can provide more specific avenues for policy and treatment interventions. For instance, the information can refine diagnostic domains in which disparities exist, specify theory concerning causal pathways to disparities, and ultimately lead to more equal distribution of services.
Difficulty in accurately measuring differences between black and white individuals with substance use disorders also arises in studies based on the World Mental Health version of the Composite International Diagnostic Interview (WMH-CIDI) such as the National Comorbidity Survey Replication study (NCS-R) (
26 ). In a deviation from
DSM-IV, the WMH-CIDI does not assess substance dependence among those without substance abuse (
25,
27,
28 ). Because approximately one-third of patients diagnosed as having substance dependence do not meet criteria for substance abuse (
25,
27,
28,
29 ), and alcohol dependence without abuse is more likely to occur among black individuals than white individuals (
27 ), NCS-R data cannot provide information on racial differences in service utilization for alcohol or drug dependence.
To overcome these methodological problems, we examined racial and ethnic differences in service utilization for mood, anxiety, alcohol use, and drug use disorders in the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). The goals of these analyses were to determine whether black and white populations differed in treatment across these disorders and to determine whether differences observed persisted after other elements described in the Andersen model were controlled for, especially if these elements differed by race. The large sample and complete measurement of alcohol and drug dependence as well as abuse, as defined by DSM-IV, allowed for an accurate and statistically powerful investigation of racial and ethnic differences in treatment use.
Results
Distribution of predispositional factors
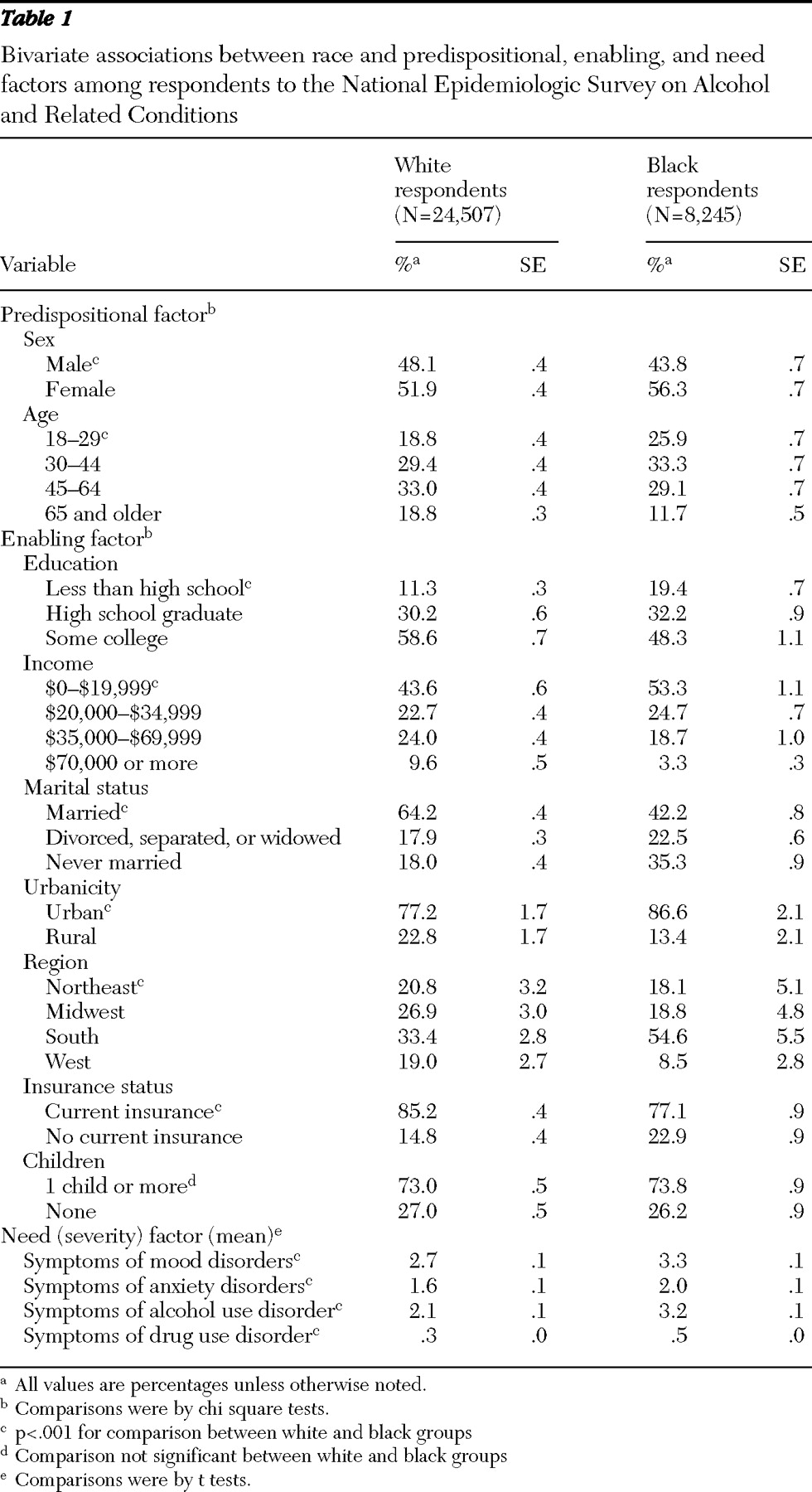
In the full sample of respondents (see
Table 1 ), there were significantly more men in the white group than in the black group (
χ 2 =19.7, df=1, p<.001). On average, black respondents were younger (
χ 2 =74.5, df=3, p<.001).
Distribution of enabling factors
Black respondents were more likely than whites to have not completed high school ( χ 2 =65.7, df=2, p<.001) and to have lower income ( χ 2 =74.0, df=3, p<.001) and were less likely to have health insurance ( χ 2 =44.7, df=1, p<.001). Black respondents were more likely to live in urban environments ( χ 2 =19.6, df=1, p<.001) and were overrepresented in the South ( χ 2 =53.8, df=3, p<.001).
Distribution of need (severity)
White respondents had significantly more symptoms for mood (t=5.6, df=65, p<.001), anxiety (t=4.9, df=65, p<.001), and alcohol use (t=13.8, df=65, p<.001) disorders. Black respondents had significantly higher drug use disorder symptoms (t=5.7, df=65, p<.001).
Associations with service utilization
Predispositional, enabling, and need factors were all significantly (p<.05) associated with service utilization in bivariate analysis (not shown). Those having lower income, residing in the western region of the United States, and having more disorder-specific symptoms were more likely to use each diagnosis-specific treatment type. Women, respondents in middle age, and respondents who were widowed, separated, or divorced were more likely to utilize mood and anxiety services. Men, younger respondents, respondents who had never married, and respondents with insurance were more likely to utilize alcohol treatment services or drug treatment services.
Likelihood of treatment utilization in diagnostic subsets
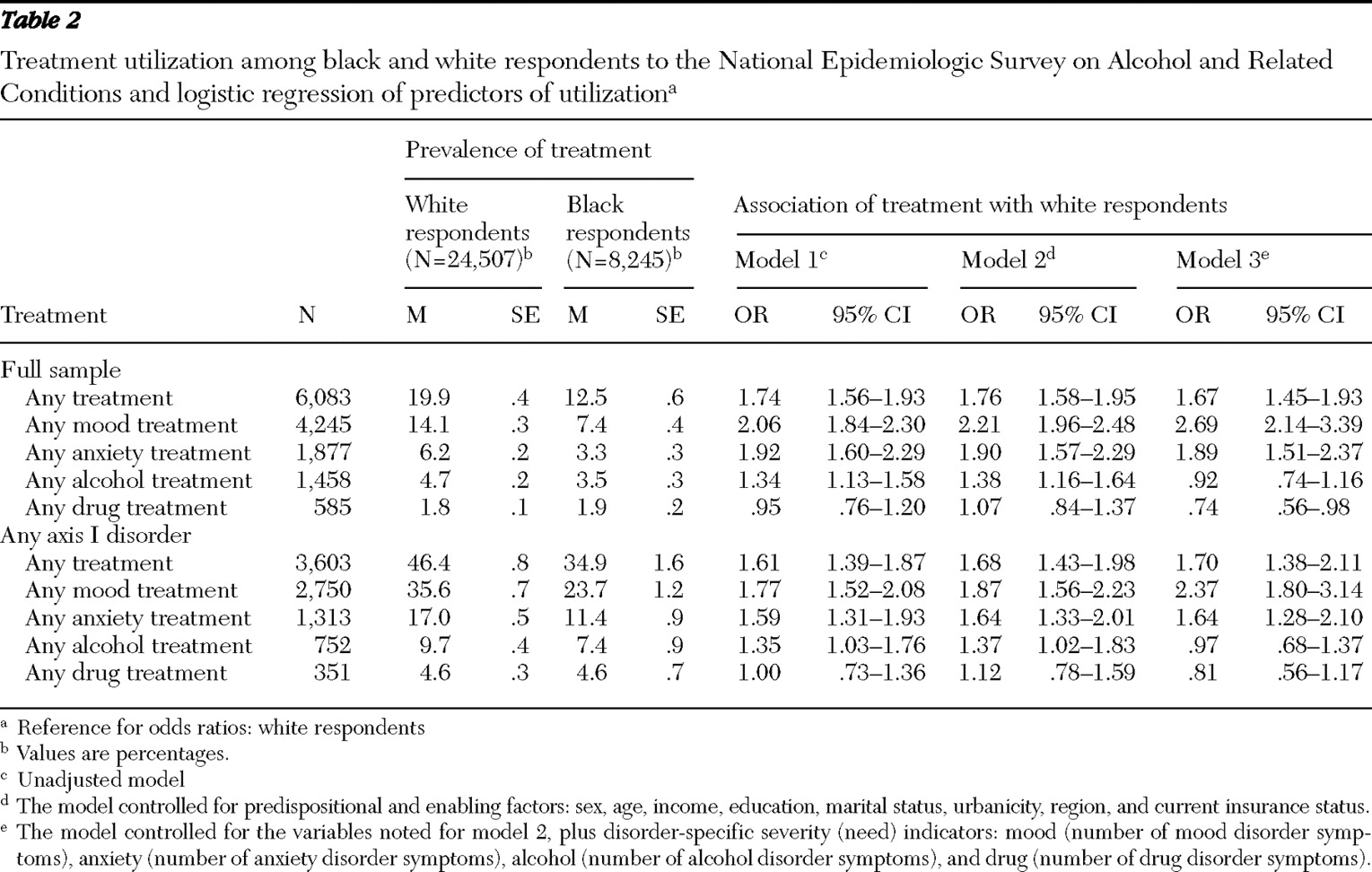
All screened respondents. Lifetime prevalence of any service utilization for mental or substance use disorders was 19.9% among white respondents and 12.5% among black respondents (
Table 2 ). Three models are presented. Model 1 indicates the unadjusted association between race and ethnicity and treatment, model 2 indicates that the association controlled for predispositional and enabling factors, and model 3 further controlled for need (severity). In all three models, the likelihood of any service utilization was significantly higher among white respondents than black respondents. In addition, the white group was significantly more likely than the black group to receive treatment services for mood disorders (OR= 2.69) and anxiety disorders (OR= 1.89) with all other factors controlled for (model 3). In contrast service utilization for alcohol treatment was not significantly different by race; however, white respondents were significantly less likely to utilize drug treatment services (OR=.74). Further subdivision into inpatient care versus outpatient care yielded similar magnitude and direction of effect (not shown).
Respondents with any axis I disorder. Among persons with any axis I disorder, the pattern of results paralleled that seen in the full sample. In fully adjusted models (model 3), white respondents were more likely than black respondents to utilize services for mood and anxiety disorders, and there were no significant differences between groups in alcohol or drug treatment utilization.
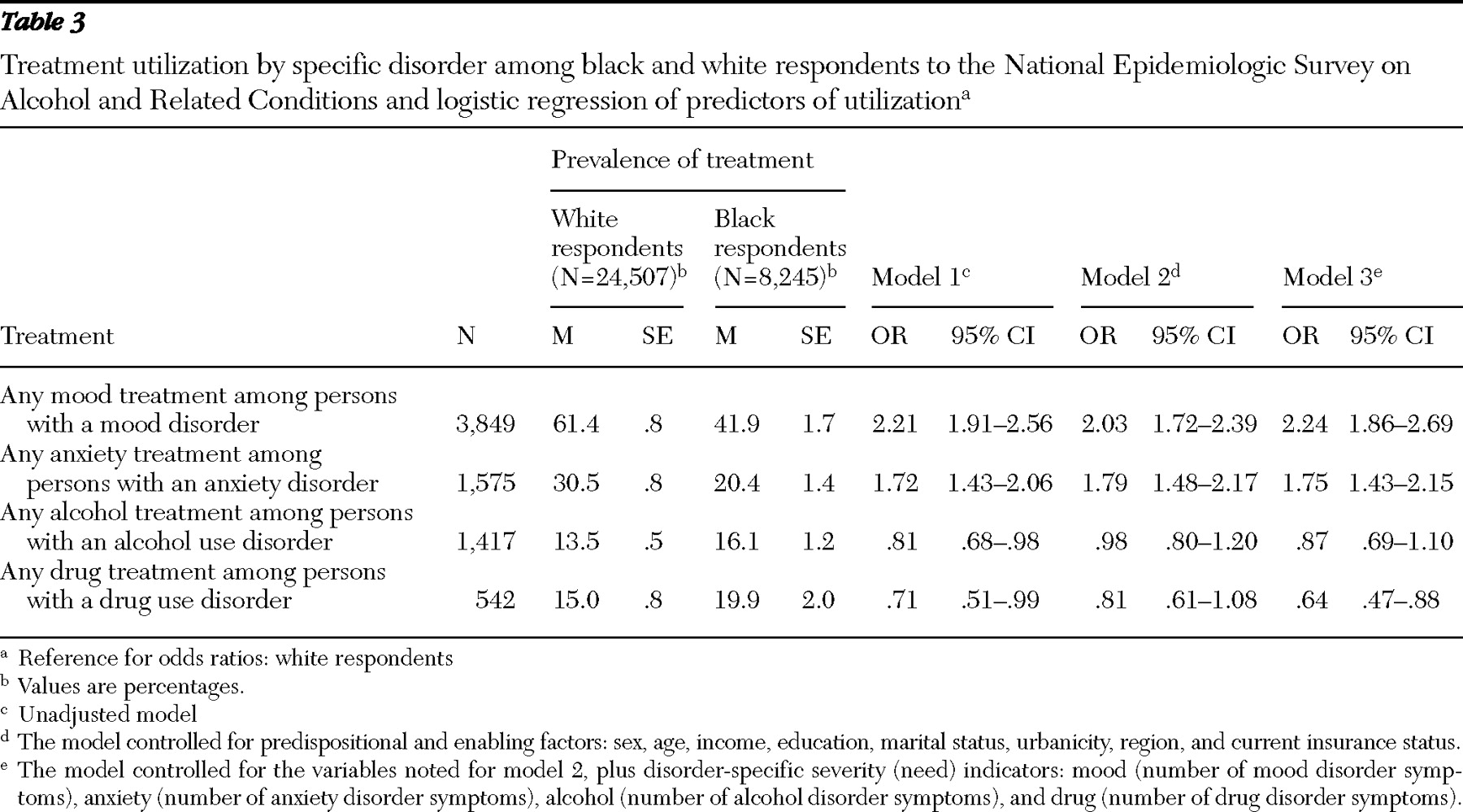
Respondents with a mood or anxiety disorder. Among respondents with mood disorders, 61.4% of white respondents and 41.9% of black respondents sought treatment (
Table 3 ). In the fully adjusted model (model 3) white respondents were significantly more likely than black respondents to use such services (OR=2.24). Among persons with anxiety disorders, white respondents were significantly more likely than black respondents to use such services in fully adjusted models (OR=1.75).
Respondents with a drug or alcohol use disorder. Among respondents with an alcohol disorder, 13.5% of whites and 16.1% of blacks utilized alcohol treatment services (
Table 3 ). Whereas with the unadjusted model black respondents were less likely than white respondents to utilize these services (
Table 3, model 1), these differences were explained by predispositional and enabling factors (
Table 3, models 2 and 3). Among respondents with a drug use disorder, 15.0% of the white group and 19.9% of the black group utilized drug services. Controlling for all predisposing, enabling and need factors, analyses showed that white respondents were significantly less likely than black respondents to utilize drug treatment services (OR=.64). Subdivision of treatment into more specific categories yielded similar magnitude and direction of effect.
Discussion
The major finding of this study is that service utilization patterns among black and white respondents depended on the specific disorder and type of treatment considered. Black respondents were consistently less likely than white respondents to receive services for mood and anxiety disorders, even after we adjusted for predispositional, enabling, and need factors associated with treatment utilization. This was true for the full sample, persons with any axis I disorder, and those whose need was specific—in other words, a mood or anxiety disorder—confirming prior findings that the black population receives fewer mental health services than the white population for treatment of mood and anxiety disorders (
1,
2,
4,
5,
6,
8,
57,
58,
59 ).
In contrast no evidence emerged of service utilization disparity between black and white respondents for alcohol or drug use disorders, despite statistical power to detect a difference. Black respondents in the full sample and among respondents with a drug use disorder were significantly more likely than white respondents to receive drug services once differences between the groups on predispositional, enabling, and need factors were controlled for. Some general population studies on race differences in substance treatment indicated no differences (
3,
4,
5 ), whereas others have suggested that the black population is less likely to utilize mental health services for substance use disorders (
17,
18,
60 ); however, these studies lacked specific diagnostic information on a full range of adults in a national sample. It should be noted that less than 20% of people with a drug or alcohol use disorder used any service, which highlights the disparity of service utilization across racial and ethnic lines.
The contrast between lower service utilization rates for black respondents with mood and anxiety disorders and equal to or higher rates than whites with alcohol use or drug use disorders raises important questions about differential service utilization patterns. Although several past studies showed that racial and ethnic differences in mental health service utilization are substantially attenuated by socioeconomic status differences (
7,
11,
15 ), this investigation indicated that disparities persisted despite differences in income or education. Other explanations may include cultural and policy-level factors. Culturally, black communities may react more negatively than white communities to hazardous drinking (
61 ) and provide greater social support for sobriety (
62 ). Cultural influences may affect conceptions of causes and treatments of mental health problems, including perceived need for treatment (
11 ), resulting in differences between black and white communities (
63 ).
Medical research has consistently shown that black persons are more likely to distrust the medical community and the health care system (
16,
64 ). There may also be important subgroup differences within the black community; for example, recent evidence indicates that African Americans may utilize more mental health services than Caribbean blacks (
65 ). Future studies using more refined racial and ethnic categories could further specify mediators of racial and ethnic differences, including nativity and acculturation, which may affect perception of the mental health care system. Racial and ethnic attitudes toward anxiety or depression have not been directly compared with attitudes toward alcohol or drug use disorders, an important direction for future research.
Furthermore, questions about the reasons for the different patterns of services in black and white populations could focus on potential confounding caused by specific subgroups within the general samples we examined. This is addressed in part elsewhere (
59 ) by examining treatment disparities among the subgroup of whites and blacks that had mood or anxiety disorder co-occurring with an alcohol or drug use disorder. In this subgroup analysis, we also found significant differences: white respondents were 2.05 times as likely as black respondents to use mood or anxiety services during their lifetime and .80 times as likely to use drug services, and again we found no difference in using alcohol services (OR=.99). Thus patterns of racial-ethnic differences in the comorbid subgroup were generally similar to the patterns shown above, despite the potential greater severity of illness among those with more than one type of disorder. This is important information because comorbidity is a strong predictor of treatment entry. Further, we examined whether the patterns of axis I treatment utilization were different among the subset of respondents with an axis II diagnosis. Results were generally similar, although there were no significant racial and ethnic differences in drug treatment service utilization among individuals with a drug use disorder. Taken together, the results of both investigations indicate that racial and ethnic differences in treatment utilization are not substantially attenuated or modified by comorbidity, and furthermore, the magnitude of difference is remarkably similar in the comorbid subgroups compared with the broader group of all individuals who received a diagnosis as analyzed in this study.
At a policy level, social coercion through law enforcement—an "external environment" enabling characteristic of the Andersen model (
23 )—might indirectly explain higher service utilization for substance use disorders among black individuals because drug policies and laws disproportionately affect black communities (
66,
67 ). At similar toxicology levels, more persons in minority groups than whites are mandated to receive alcohol treatment by the criminal justice system (
68,
69 ). Also, some evidence indicates that black persons who enter the mental health system are more likely than whites to have entered through coercion (
70,
71,
72,
73 ). Future studies should determine how social pressure and legal coercion influence entry into services for different disorders and how this affects larger perceptions of treatment for the different disorders by race and ethnicity. In addition, mental health service delivery systems have changed over time; determining that disparities vary across changes in the mental health service system over time would suggest mechanisms through which disparities exist.
We now address limitations of the study. First, in the examination of lifetime disorders and service utilization, respondents' recall bias might have affected estimates, particularly among older respondents. To investigate this, we reran our analysis limited to current (past 12 months) disorders. The magnitude and direction of effects were virtually unchanged, suggesting that recall bias did not substantially affect our estimates. Smaller numbers of respondents in diagnostic categories limited the power to detect effects, so for this reason, as well as the high quality of the lifetime diagnoses provided by the AUDADIS-IV (
35,
36,
37,
38,
39,
40,
41,
46,
47,
48,
49,
50,
55 ), we reported lifetime measures. Recall bias can also affect the type and timing of treatment reported. We assume that there would be no racial or ethnic difference in recall, but evidence (which is lacking) on the accuracy of this assumption would assist in interpreting the results.
Second, individuals institutionalized for mental disorders or incarcerated throughout the data collection were not included; disparities in institutionalization could bias the findings. Persons from the black community have higher incarceration rates, but studies are inconsistent on whether persons belonging to minority groups receive fewer mental health services in prison than whites do (
74,
75,
76,
77 ). Racial and ethnic differences in rates of long-term mental health institutionalization are also unclear (
15,
78 ), so institutionalization effects on our findings are uncertain. Third, these data were cross-sectional. Longitudinal data would allow prospective examination of factors predicting entry into mental health services, which will be possible when NESARC follow-up data become available.
The NESARC did not focus solely on treatment utilization; additional detail on treatment in future surveys would be helpful. However, differences in questions regarding mood and anxiety treatment and alcohol or drug treatment utilization reflect true differences in both the services and service delivery systems for these disorders. In addition, racial and ethnic differences reflect differences in services available as well as individual treatment choices. Future surveys should include information on services available to the respondent. Finally, this study addressed disparities in service utilization but could not address other important disparities, such as quality, appropriateness, and efficacy of care. Although disparities in quality of care within treatment services have been shown (
68 ), this study highlights disparities in receiving any care at all.